CHAPTER 24 Lunotriquetral Tears
After a thorough history, physical examination, and ancillary radiographic imaging, wrist arthroscopy further characterizes a wrist injury to better guide treatment. Arthroscopic evaluation is particularly valuable to examine the anatomy and pathoanatomy of ulnar-sided wrist disorders.1 Lunotriquetral (LT) interosseous ligament tears may exist in isolation but often are part of a broader spectrum of wrist pathology. The arthroscopic treatment of ulnar-side pathology with LT interosseous ligament tears often includes débridement and synovectomy, repair of chondral injuries and triangular fibrocartilage tears, and LT joint arthroscopic reduction and internal fixation (ARIF).
ANATOMY
The LT interosseous ligament is thicker volarly and dorsally,2 with a membranous central portion that is not uncommonly torn without resulting in instability; these tears are clinically insignificant. Clinically significant LT instability arises from intrinsic and extrinsic ligamentous injuries.3–5 Key anatomy for the arthroscopic treatment of LT tears is based on the normal ulnar-sided anatomy. Ulnar-sided stability is imparted from the integrity of the LT ligament3 in association with the ulnolunate (UL), ulnotriquetral (UT),3–5 dorsal radiotriquetral, and scaphotriquetral ligaments.3,4,6 Ulnar wrist forces also pass through the triangular fibrocartilage complex (TFCC) to help stabilize the ulnar carpus and transmit axial forces to the ulna.7,8 The volar and dorsal aspects of the LT ligament merge with the ulnocarpal extrinsic ligaments volarly and the dorsal radiolunotriquetral ligament dorsally, anchoring the triquetrum.9 The UL and UT ligaments originate on the volar TFCC and insert on the volar lunate and volar triquetrum, respectively, as well as on the LT ligament.10–12 Just palmar lies the ulnocapitate ligament, which provides a direct attachment from the ulna to the palmar ulnar ligamentous complex.
Ligament plication has been implemented to manage capitolunate instability.13 Arthroscopic treatment of LT tears is based on the anatomic and biomechanical contributions of the ulnocarpal ligaments (UL and UT) to LT joint stability. In addition to ARIF of the LT, suture plication augments capsular repair and shortens the ulnocarpal ligaments (reminiscent of ulnar shortening), reducing their contribution to the LT joint to enhance the extrinsic ligament contribution to stability. The ulnocarpal ligaments diverge from their origin on the volar TFCC to insert distally on the triquetrum and lunate in a V formation. Suture plication of the ulnar ligaments closes the V and serves to shorten the ulnar carpal ligaments and augment the palmar capsular tissue of the LT joint.
The TFCC often is a component of more extensive ulnar-sided injuries14 and does not preclude arthroscopic treatment. Severe LT instability with significant damage to both the dorsal the radiotriquetral and the scaphotriquetral ligament results in volar intercalated segment instability (VISI)3,4,6; static instability (VISI) is not readily amenable to complete arthroscopic repair.
PATIENT EVALUATION
History and Physical Examination
Historically, patients may not recall a specific inciting event. Commonly, LT interosseous ligament tears associated with instability result from a single traumatic event, such as a twisting injury or a fall on an outstretched hand with a pronated forearm. The axial and dorsally directed forces result in wrist extension with radial deviation.15,16 With intercarpal pronation, disruption of the LT interosseous ligament, and associated injury to the disk-triquetral and disk-lunate ligaments, tearing occurs, and LT instability may be greater.
After a general wrist examination, including inspection, palpation, and general range of motion and stability, an examination focused on ulnar-sided pathology is carried out. Patient localization of pain is helpful; diffuse, nonlocalizing pain is not typical of ulnar-sided instability. The dorsal and volar aspects of the TFCC, the dorsal LT joint, and the extensor carpi ulnaris (ECU) are the main areas to palpate. Depending on the acuteness of the injury, tenderness may or may not be present. Maneuvers to provoke pain caused by excessive unwanted translation of the triquetrum and lunate further elucidate ulnar-sided pain complaints. Although none of the tests is diagnostic in isolation, when performed as part of the comprehensive evaluation, the tests can better characterize pain complaints. Provocative stability maneuvers used to assess the LT joint include LT ballottement (compressing the triquetrum against the lunate), the shuck test as described by Reagan and colleagues,6 the shear test as described by Kleinman,17,18 and distal radioulnar translation (to infer stability).9,19 In addition to ulnar impaction testing, ulnar deviation should be performed with the wrist in flexed, extended, and neutral positions. The stability of the distal radioulnar joint is also assessed. Assessing the patient response to provocative maneuvers and comparing perceived translation with the contralateral wrist are useful.
Diagnostic Imaging
The radiographic evaluation of a painful wrist should start with a minimum of a zero rotation posteroanterior20,21 view and a true lateral view of the wrist. Comparison views of the contralateral wrist are useful. In these radiographic views and after assessment of the soft tissue shadows, specific osseous relationships should be documented. The focused analysis includes ulnar variance,22 LT interval, integrity of the subchondral joint surfaces, greater and lesser arc continuity,23 and radiolunate and scapholunate angles.
The clinical value of advanced radiographic evaluation of the wrist is subject to geographic variability. Magnetic resonance imaging (MRI) with or without the addition of arthrography is beneficial, provided an expert radiologist is available. Variations in the accuracy of MRI and diagnostic arthroscopy may simply be related to skills of the radiologist and the arthroscopic surgeon. In general, a high field magnet with a dedicated extremity helps to optimize spatial resolution.24 Assessment of the LT joint is variable25 and should be made in the context of the history and physical examination.
TREATMENT
Surgical Management
With failure of conservative treatment or unstable injuries, arthroscopic treatment of is a reasonable option and includes radiocarpal and midcarpal arthroscopy. The first step is to assess the degree of instability26 and associated injuries. Partial LT injuries may be treated with débridement alone.27,28 In 1995, Osterman and Seidman29 combined débridement with isolated pinning of the LT joint and reported good results. Nonarthroscopic treatment, although not the focus of the chapter, has been described. In a comparison of techniques,30 subjective results tended to be better for direct repair or reconstruction than for LT fusion.
Arthroscopic Technique
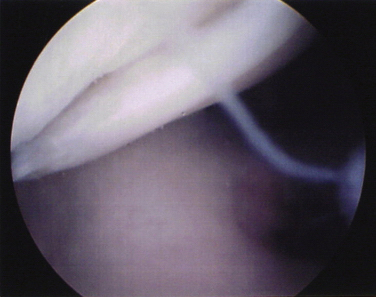
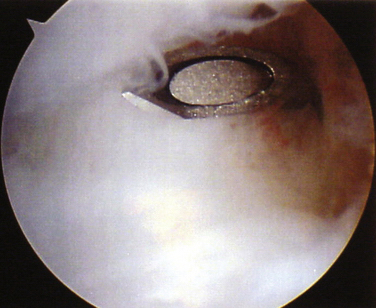
An arthroscopic video system should be positioned to allow a clear view of the monitor by the surgeon and assistant. After the limb is exsanguinated, a traction tower is used, and 8 to 10 pounds of traction is applied through finger traps with the arm strapped to the hand table. The portals used for arthroscopic stabilization include the 3-4, 6-R, volar 6-U, and radial and ulnar midcarpal portals for the arthroscopic capsulodesis and ARIF. Depending on each unique case, the addition of a 4-5 portal as a working or viewing portal can be helpful. The LT joint can be visualized directly from an ulnar portal (6-R or 4-5) to ensure complete, dorsal to palmar visualization of the LT ligament (Fig. 24-1) and débridement as necessary. After identification of pathology and débridement, an ulnar portal at the level of the volar ligaments, volar 6-U, is created after midcarpal assessment and is used for suture passing.
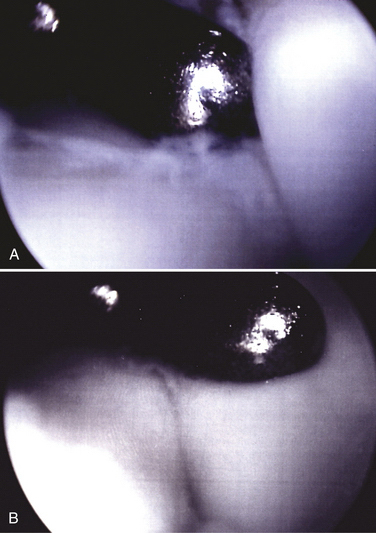
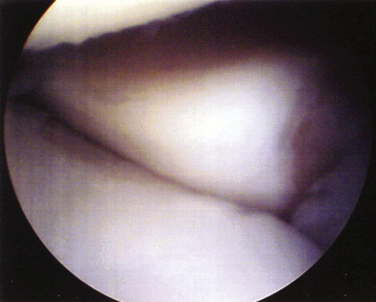
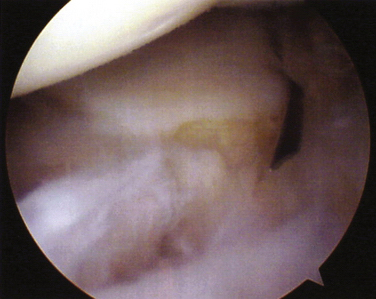
Starting with the arthroscope inserted into the radial midcarpal portal, the surgeon creates an ulnar midcarpal portal for the working portal. The LT joint is assessed for congruency and laxity of the triquetrum. The lunate and triquetrum should be colinear. If the view of the LT joint from the midcarpal radial portal is blocked by a separate lunate facet,31 the arthroscope is placed in the midcarpal ulnar portal to gain visualization. Under these conditions, the radial articular edge of triquetrum should be aligned with the most ulnar articular edge of the hamate facet of the lunate (Fig. 24-2). The LT joint may be unstable because of excessive laxity while still being congruent. Laxity should be assessed both on triquetral rotation and on separation from the lunate. From the midcarpus, the dorsal portion of the triquetrum is often rotated so that its articular surface is distal to the lunate in an unstable LT joint (Fig. 24-3). The triquetrum can be translated to a reduced state in which the articular surfaces of the triquetrum and lunate are collinear. Further, the triquetrum can be ulnarly translated so as to “gap open” the LT joint. Normal scapholunate joint laxity can be used as a reference. Also, the dorsal radiocarpal and dorsal intercarpal ligaments attached to the lunate and triquetrum may be avulsed (Fig. 24-4) and should be repaired.
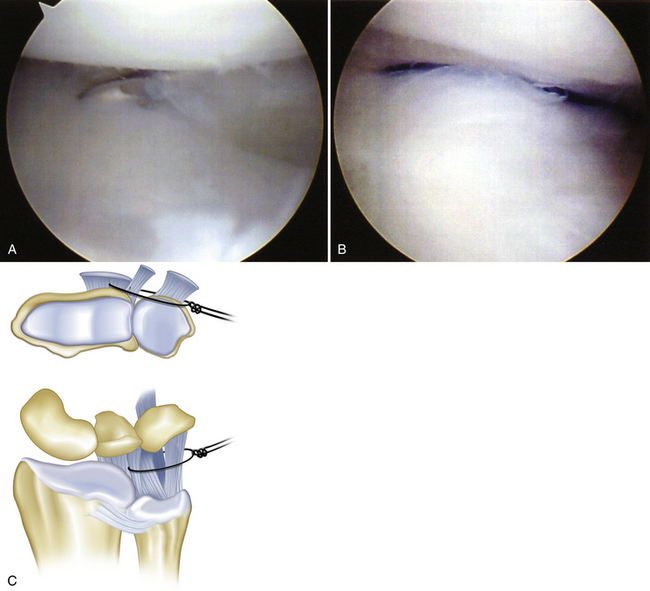
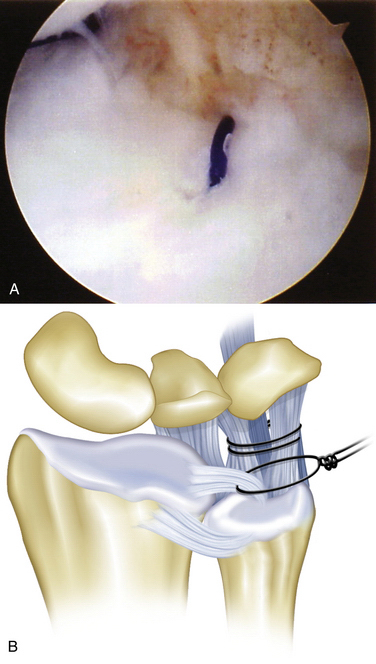
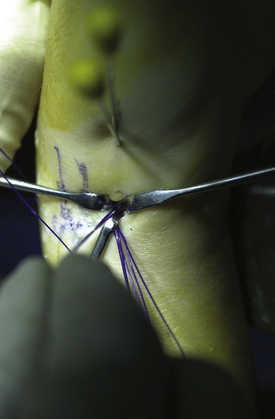
After confirmation of LT instability, the arthroscope is placed in the 3-4 portal during ulnocarpal (UL, ulnocapitate, UT) ligament plication. The volar 6-U (v6-U) portal is established. The v6-U portal is similar to the normal 6-U portal, but it is placed just dorsal to the disk-carpal ligaments (Fig. 24-5). Care is taken to avoid injury to the dorsal sensory branches of the ulnar nerve during placement. The UL and UT ligaments are gently débrided to induce a vascular response. Through the v6-U portal, an 18-gauge spinal needle is passed just volar to the ulnocarpal ligaments and enters the wrist at the radial edge of the UL ligament, just distal to the articular surface of the radius (Fig. 24-6A). A 2-0 polydioxone (PDS) suture is placed through the needle into the joint. The suture is retrieved through the 6-R or the v6-U and tagged as the first plicating suture (see Fig. 24-6B and C). In a similar fashion, the second plicating suture is placed approximately 5 mm distal to the first (Fig. 24-7A), so that the suture loops are parallel to the lunate and triquetrum, and is tagged as the second plicating suture (see Fig. 24-7B and C). Tension on the first stitch often facilitates a second needle passage through the UL and UT ligaments. Adequacy of the plication (tension on the stitch) and its effect on LT interval stability should be assessed after each suture passage. Finally, the spinal needle is passed through the volar aspect of the capsule at the volar-most aspect of the TFCC at the prestyloid recess, as in peripheral repair techniques (Fig. 24-8A). The three sets of sutures are tied at the termination of the procedure, after the LT joint has been congruently reduced and stabilized with Kirschner wires (see Fig. 24-8B).
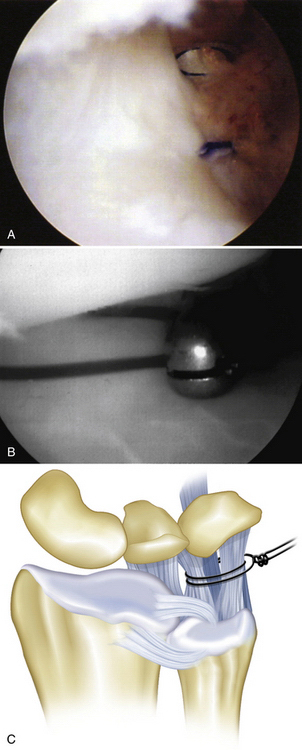
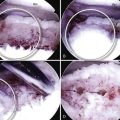
FIGURE 24-7 A, The ulnotriquetral ligament is to the left. The first plicating suture is seen below and to the right (ulnar), exiting ulnarly through the volar 6-U portal. The spinal needle is seen distally as it is ready to be passed for the second plicating suture. B, The second 2-0 polydioxone (PDS) plication suture is placed. Tension on the first suture facilitates placement of the second suture, which is placed approximately 5 mm distal to the first suture. C, The plication sutures are represented diagrammatically.
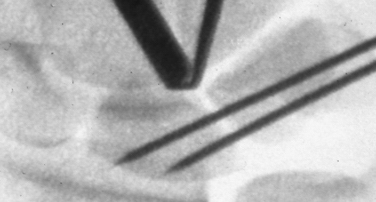
With the arthroscope in the midcarpal radial portal, a spinal needle can be placed from the ulnar to the radial side across the distal aspect of the LT as a guide for percutaneous Kirschner wire placement with or without concurrent fluoroscopy (Fig. 24-9). After the triquetrum has been reduced through the midcarpal ulnar portal with a probe and traction on the plication sutures, the initial 0.045-inch smooth Kirschner wire is inserted just proximal to the spinal needle and drilled across the LT joint. The second Kirschner wire is placed just proximal to the first (Fig. 24-10). Traction is released after Kirschner wire stabilization, and the forearm is held in neutral rotation while the plication sutures are tied (Fig. 24-11). The Kirschner wires are either cut subcutaneously or bent outside the skin.
In the presence of a peripheral triangular fibrocartilage tear, sutures should be passed after the plication sutures and tied separately in the dorsal incision; central triangular fibrocartilage tears can be débrided during the initial débridement. Patients with LT tears often have positive ulnar variance.32,33 In the presence of ulnar-positive ulnar impaction, an arthroscopic wafer procedure should be considered.
CONCLUSIONS
An initial case series of 21 patients were examined retrospectively at a mean of 2 years 6 months (range, 1 week to 5.5 years) after treatment. Seventeen of the patients recalled a specific injury (hyperextension, 12; twisting, 2; unknown, 3), and four described a gradual onset of symptoms without specific recollection of an acute injury. Three patients had additional significant injuries to the affected extremity: elbow dislocation, humeral shaft fracture, and anterior shoulder dislocation. The patients were uniformly experienced tenderness over the LT joint. Provocative tests for LT instability were specifically positive in nine patients and tests for TFCC injury were positive in six. Crepitus was produced with pronosupination or ulnar deviation in 10 patients. The mean preoperative Mayo wrist score was 50, and the mean postoperative score was 88; 19 of 21 patients had excellent and good results, and two had fair results. Three patients had complications including prolonged tenderness along the extensor carpi ulnaris, and one patient had persistent neuritis of the dorsal branches of the ulnar nerve.
1. Kulick M, Chen C, Swearingen P. Determining the diagnostic accuracy of wrist arthroscopy. Toronto: Paper presented at the annual meeting of the American Society for Surgery of the Hand; 1990.
2. Ritt MJ, Bishop AT, Berger RA, et al. Lunotriquetral ligament properties: a comparison of three anatomic subregions. J Hand Surg Am. 23, 1998; 425-431.
3. Horii E, Gacias-Elias M, An K, et al. A kinematic study of lunato-triquetral dislocations. J Hand Surg Am. 1991;16:355-362.
4. Viegas S, Peterson P, Peterson PD, et al. Ulnar-sided perilunate instability: an anatomic and biomechanical study. J Hand Surg Am. 1990;15:268-278.
5. Trumble T, Bour C, Smith R, et al. Kinematics of the ulnar carpus to the volar intercalated segment instability pattern. J Hand Surg Am. 1990;15:384-392.
6. Reagan DS, Linscheid RL, Dobyns JH. Lunotriquetral sprains. J Hand Surg Am. 1984;9:502-514.
7. Palmer A, Werner F. Triangular fibrocartilage complex of the wrist: anatomy and function. J Hand Surg Am. 1981;6:153-162.
8. Werner F, Palmer A, Fortino M, et al. Force transmission through the distal ulna: effect of ulnar variance, lunate fossa angulation, and radial and palmar tilt of the distal radius. J Hand Surg Am. 1992;17:423-428.
9. Green D. Carpal dislocation and instabilities. In: Green D, editor. Operative Hand Surgery. New York, NY: Churchill Livingston; 1988:878-879.
10. Palmer A, Werner F. Biomechanics of the distal radioulnar joint. Clin Orthop. 1984;187:26-35.
11. Garcias-Elias M, Domenech-Mateu J. The articular disc of the wrist: limits and relations. Acta Anat. 1987;128:51-54.
12. Melone C, Nathan R. Traumatic disruption of the triangular fibrocartilage complex: pathoanatomy. Clin Orthop. 1992;275:65-73.
13. Johnson R, Carrera G. Chronic capitolunate instability. J Bone Joint Surg Am. 1986;68A:1164-1176.
14. Melone CJr, Nathan R. Traumatic disruption of the triangular fibrocartilage complex: pathoanatomy. Clin Orthop. 1992;275:65-73.
15. Palmer C, Murray P, Snearly W. The mechanism of ulnar sided perilunate instability of the wrist. Minneapolis, MN: Paper presented at the 53rd annual meeting of the American Society for Surgery of the Hand; 1998.
16. Shin AY, Deitch MA, Sachar K, Boyer MI. Ulnar-sided wrist pain: diagnosis and treatment. Instr Course Lect. 2005;54:115-128.
17. Kleinman W. Physical examination of lunatotriquetral joint. Am Soc Surg Hand Corr Newsl. 51, 1985.
18. Kleinman W. Long-term study of chronic scapho-lunate instability treated by scapho-trapezio-trapezoid arthodesis. J Hand Surg Am. 1989;14:429-445.
19. Palmer A. Triangular fibrocartilage complex lesions: a classification. J Hand Surg Am. 1989;14:594-606.
20. Palmer A, Glisson R, Werner F. Ulnar variance determination. J Hand Surg Am. 1982;7:376-379.
21. Hardy DC, Totty WG, Reinus WR, Gilula L. Posteroanterior wrist radiography: importance of arm positioning. J Hand Surg Am. 1987;12:504-508.
22. Steyers C, Blair W. Measuring ulnar variance: a comparison of techniques. J Hand Surg Am. 1989;14:607-612.
23. Gilula L. Carpal injuries: analytic approach and case exercises. Am J Radiol. 1979;133:503-517.
24. Tanaka T, Yoshioka H, Ueno T, et al. Comparison between high-resolution MRI with a microscopy coil and arthroscopy in triangular fibrocartilage complex injury. J Hand Surg Am. 2006;31:1308-1314.
25. Zanetti M, Saupe N, Nagy L. Role of MR imaging in chronic wrist pain. Eur Radiol. 2007;17:927-938.
26. Geissler WB, Freeland AE, Savoie FH, et al. Intracarpal soft-tissue lesions associated with an intra-articular fracture of the distal end of the radius. J Bone Joint Surg Am. 1996;78:357-365.
27. Weiss AP, Sachar K, Glowacki KA. Arthroscopic debridement alone for intercarpal ligament tears. J Hand Surg Am. 1997;22:344-349.
28. Ruch DS, Poehling GG. Arthroscopic management of partial scapholunate and lunotriquetral injuries of the wrist. J Hand Surg Am. 1996;21:412-417.
29. Osterman AL, Seidman GD. The role of arthroscopy in the treatment of lunatotriquetral ligament injuries. Hand Clin. 1995;11:41-50.
30. Shin AY, Weinstein LP, Berger RA, Bishop AT. Treatment of isolated injuries of the lunotriquetral ligament: a comparison of arthrodesis, ligament reconstruction and ligament repair. J Bone Joint Surg Br. 2001;83:1023-1028.
31. Viegas S, Wagner K, Patterson R, et al. Medial (hamate) facet of the lunate. J Hand Surg Am. 1990;15:564-571.
32. Pin P, Young V, Gilula L, et al. Management of chronic lunatotriquetral ligament tears. J Hand Surg Am. 1989;14:77-83.
33. Osterman A, Sidman G. The role of arthroscopy in the treatment of lunatotriquetral ligament injuries. Hand Clin. 1995;11:41-50.