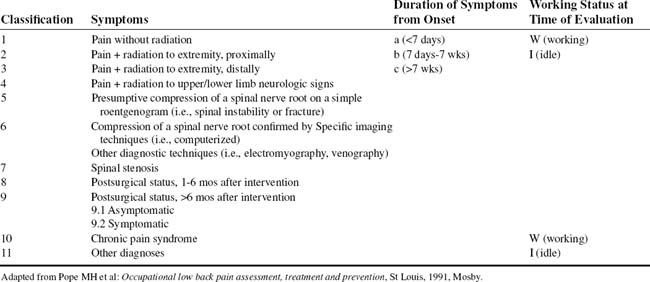
CHAPTER EIGHT LUMBAR SPINE
AXIOMS IN ASSESSING THE LUMBAR SPINE
INTRODUCTION
As many as 90% of patients with back pain have a mechanical reason for their pain. Mechanical low back pain may be defined as pain secondary to overuse of a normal anatomic structure or pain secondary to trauma or deformity of an anatomic structure. The age of a patient is helpful in determining the potential cause of back pain. In considering spondyloarthropathies, clinical characteristics help in differentiating the diseases belonging in this group (Table 8-3 and Table 8-4). The sex of the patient may also help select potential causes of low back pain. Certain disorders occur more often in men, whereas others are associated more commonly with women. Others occur equally in both sexes (Table 8-5).
HLA, Human leukocyte antigen.
Adapted From Kelley WN et al: Textbook of rheumatology, ed 5, Philadelphia, 1997, WB Saunders.
TABLE 8-4 DISEASES BELONGING TO THE SPONDYLOARTHROPATHIES
Adapted From Kelley WN et al: Textbook of rheumatology, ed 5, Philadelphia, 1997, WB Saunders.
TABLE 8-5 GENDER PREVALENCE IN LOW BACK PAIN
| Male predominance | |
| Female predominance |
Data from Klippel JH, Dieppe PA: Rheumatology, vol 1-2, ed 2, London, 1998, Mosby.
Even if treatment involves only a localized part of the lumbar spine, in each case, the lumbar spine has to be considered as a functional unit consisting of bones, ligaments, intervertebral discs, muscles, and all other soft tissues. Because of their central location, spinal elements represent the focal point for the equilibrium of the body. Because of the many connections and relations, spinal changes influence some organs directly, and the functional equilibrium of the spine depends on the efficient performance of other organs.
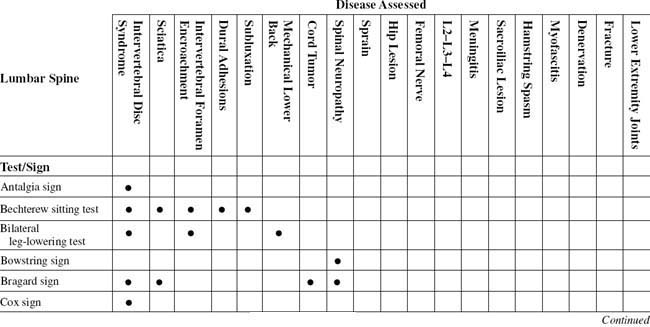
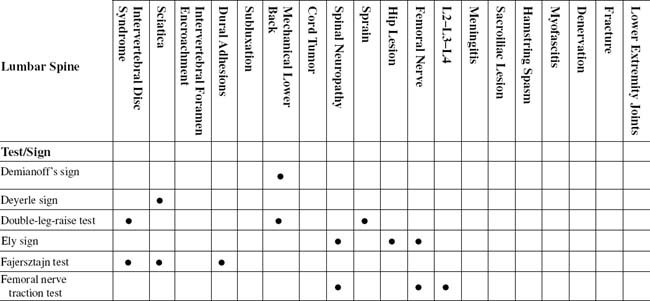
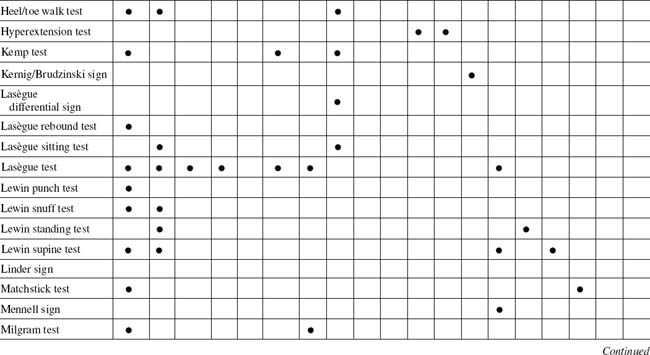
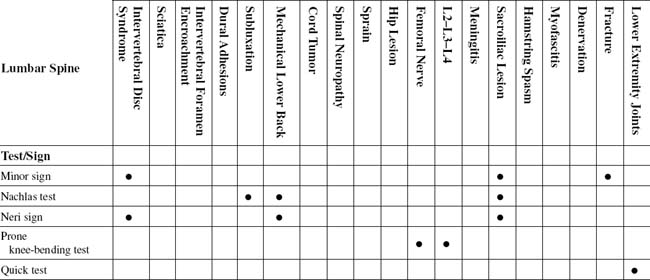
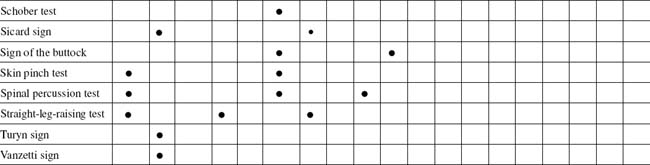
TABLE 8-2 LUMBAR SPINE CROSS-REFERENCE TABLE BY SYNDROME OR TISSUE
| Cord tumor | |
| Denervation | |
| Dural adhesions | |
| Femoral nerve | |
| Fracture | |
| Hamstring spasm | Lewin standing test |
| Hip lesion | |
| Intervertebral disc syndrome | |
| Intervertebral foramen encroachment | |
| L2–L3–L4 | |
| Lower extremity joints | Quick test |
| Mechanical lower back | |
| Meningitis | Kernig/Brudzinski sign |
| Myofascitis | |
| Sacroiliac lesion | |
| Sciatica | |
| Spinal neuropathy | |
| Sprain | |
| Subluxation |
During fetal development, the spine may be exposed to many influences, such as drug-induced malformations, lack of oxygen, or radiation.
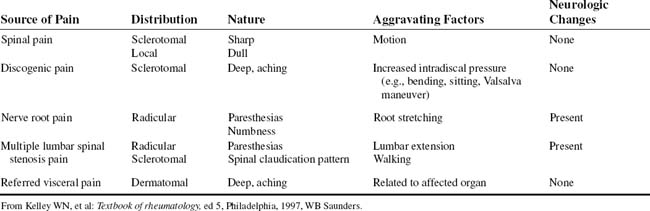
The anatomic structures of the lumbosacral spine receive specific types of sensory innervation that are associated with distinct qualities of pain (Table 8-6).
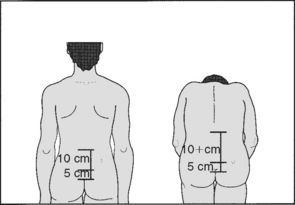
ESSENTIAL MOTION ASSESSMENT
To assess the contribution made to flexion by the lumbar spine, the examiner should mark the spine at the lumbosacral junction and then 10 cm above and 5 cm below this point. On forward flexion, the distance between the two upper marks should increase by approximately 4 cm, the distance between the lower two remaining unaltered (Figs. 8-1 to 8-4).
ESSENTIAL MUSCLE FUNCTION ASSESSMENT
Useful in screening is muscle testing of the legs, which measures strength on a 5-point scale for extension and flexion (knee), abduction and adduction (hip), and eversion and inversion, as well as dorsiflexion and plantar flexion (foot) (Table 8-7).
For patients in whom the objective findings do not match the subjective complaints, close observation helps identify the inconsistencies (Table 8-8). A finding of three or more of the five signs of the Waddell index is clinically significant. Isolated positive signs are ignored.
TABLE 8-8 NONORGANIC PHYSICAL SIGNS INDICATING ILLNESS BEHAVIOR
| Physical Disease/Normal Illness Behavior | Abnormal Illness Behavior | |
|---|---|---|
| Symptoms | ||
| Pain | Anatomic distribution | Whole leg pain |
| Tailbone pain | ||
| Numbness | Dermatomal | Whole leg numbness |
| Weakness | Myotomal | Whole leg giving way |
| Time pattern | Varies with time and activity | Never free of pain |
| Response to treatment | Variable benefit | Intolerance of treatments |
| Emergency admissions to hospital | ||
| Signs | ||
| Tenderness | Anatomic distribution | Superficial |
| Widespread nonanatomic | ||
| Axial loading | No lumbar pain | Lumbar pain |
| Simulated rotation | No lumbar pain | Lumbar pain |
| Straight leg raising | Limited on distraction | Improves with distraction |
| Sensory | Dermatomal | Regional |
| Motor | Myotomal | Regional, jerky, giving way |
From Demeter SL, Andersson GBJ, Smith GM: Disability evaluation, St Louis, 1996, Mosby.
The iliacus arises from the iliac fossa and joins the psoas under the inguinal ligament. The iliacus then crosses the hip joint capsule and inserts into the lesser trochanter of the femur. These muscles flex the lumbar spine and bend it toward the same side. The quadratus lumborum, which lies lateral to the vertebral column, arises from the posterior part of the iliac crest and iliolumbar ligament and inserts into the twelfth rib and the tips of the transverse processes of the upper four lumbar vertebrae. This muscle fixes the diaphragm during inspiration and bends the trunk toward the same side when it acts alone (Figs. 8-5 to 8-7).
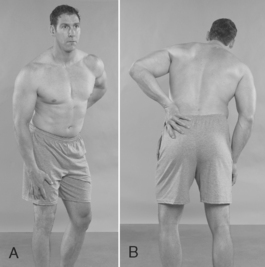
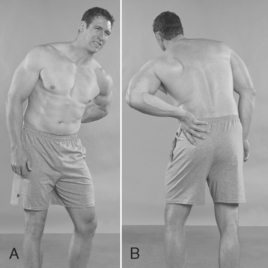
ANTALGIA SIGN
Assessment for Posterolateral, Posteromedial, and Posterocentral Intervertebral Disc Protrusion
Comment
Two major types of low back abnormalities center on the intervertebral disc: acute impairment from herniated discs and chronic impairment from degenerative disc disease (Table 8-9).
| Lumbar Herniated Nucleus Pulposus | Degenerative Disc Disease | |
|---|---|---|
| Physical examination findings |
CT, Computed tomography; MRI, magnetic resonance imaging.
Adapted from Brier SR: Primary care orthopedics, St Louis, 1999, Mosby.
ORTHOPEDIC GAMUT 8-2 DISC INJURIES
Definitions of disc injuries are as follows:
PROCEDURE
PROCEDURE
BOWSTRING SIGN
Assessment for Lumbar Nerve Root Compression
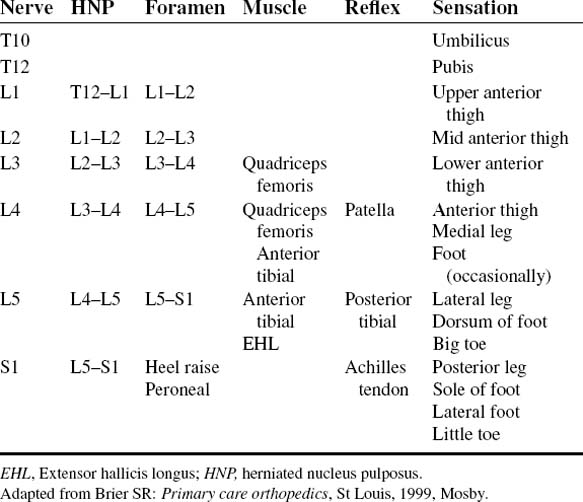
ORTHOPEDIC GAMUT 8-3 LUMBOSACRAL NERVE ROOTS
ORTHOPEDIC GAMUT 8-4 WALLERIAN DEGENERATION SEQUENCE
PROCEDURE
PROCEDURE
COX SIGN
Assessment for Prolapse of Intervertebral Disc Nucleus
Comment
Several maneuvers tighten the sciatic nerve and compress an inflamed nerve root against a herniated lumbar disc. With the straight-leg-raising tests, the L5 and S1 nerve roots move several millimeters at the level of the foramen. The L4 nerve root moves a smaller distance, and the proximal roots show little motion. The straight-leg-raising tests are most important and valuable for detecting lesions of the L5 and S1 nerve roots. Young patients with herniated discs have marked propensities for positive straight-leg-raising tests. Although the test itself is not pathognomonic, a negative test rules out the possibility of a herniated disc. After age 30, a negative straight-leg-raising test no longer precludes this diagnosis. Lumbosacral transitional vertebrae complicate this further (Table 8-10).
TABLE 8-10 CASTELLVI CLASSIFICATION OF LUMBOSACRAL TRANSITIONAL VERTEBRA
PROCEDURE
DEMIANOFF SIGN
PROCEDURE
DEYERLE SIGN
Assessment for Sciatic Nerve Irritation
From Kirkaldy WH: Managing low back pain, ed 4, Philadelphia 1999, Churchill Livingstone.
PROCEDURE
PROCEDURE
ELY SIGN
ELY HEEL-TO-BUTTOCK TEST
Assessment for Lumbar Radicular or Femoral Nerve Inflammation
Comment
The size of the lumbar vertebral canal ranges from 12 to 20 mm in its AP dimension at the mid sagittal plane and 18 to 27 mm in its transverse diameter. Stenosis has been defined as a narrowing below the lowest value of the range of normal (Table 8-12).
TABLE 8-12 DIMENSIONS OF THE LUMBAR VERTEBRAL FORAMINA (VERTEBRAL CANAL)*
| Dimension | Size (Range)† |
|---|---|
| Anteroposterior (in midsagittal plane) | 12–20 mm |
| Transverse (interpedicular distance) | 18–27 mm |
‡ A typical vertebral foramen is rather triangular (trefoil) in shape. However, the upper lumbar vertebral foramina are more rounded than the lower lumbar foramina. L1 is the most rounded, and each succeeding lumbar vertebra becomes increasingly triangular, with L5 the most dramatically trefoil of all. From Dommisse GF, Louw JA: Anatomy of the lumbar spine. In Floman Y, editor: Disorders of the lumbar spine, Rockville, Md, and Tel Aviv, Israel, 1990, Aspen and Freund Publishing House.
* Dimensions below the lowest value indicate spinal (vertebral) canal stenosis.
† Dimensions of lumbar vertebral foramina are usually smaller than those of the cervical region but larger than those of the thoracic region. From Cramer GD, Darby SA: Basic and clinical anatomy of the spine, spinal cord, and ANS, St Louis, 1995, Mosby.
ORTHOPEDIC GAMUT 8-7 MODIFIED ARNOLD INTERNATIONAL CLASSIFICATION OF LUMBAR SPINAL STENOSIS AND NERVE ROOT ENTRAPMENT SYNDROMES
ORTHOPEDIC GAMUT 8-8 COMPLEX REGIONAL PAIN SYNDROME DIAGNOSTIC CRITERIA (INTERNATIONAL ASSOCIATION FOR THE STUDY OF PAIN)
PROCEDURE
FAJERSZTAJN TEST
PROCEDURE
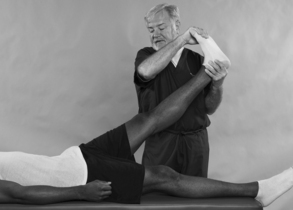
FEMORAL NERVE TRACTION TEST
Assessment for Mid Lumbar Nerve Root Involvement (L2, L3, and L4)
Comment
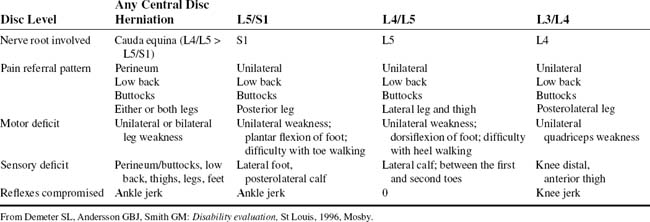
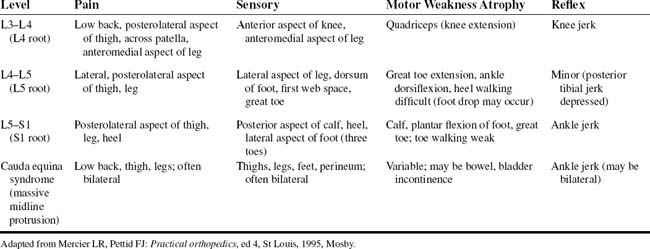
A large, midline disc herniation can compress several nerve roots of the cauda equina and can mimic an intraspinal tumor. Usually, lower back and perineal symptoms predominate, with radicular symptoms being masked. Difficulty with urination, such as frequency or overflow incontinence, may develop early. In men, a recent history of sexual impotence may be elicited. The patients experience pain down the posterior thighs to the soles of the feet accompanied by weakness of the legs and feet. L2, L3, and L4 radiculopathies are less common than the L5 and S1 radiculopathies, probably because of their relatively short course within the cauda equina, which makes them less susceptible to compression (Table 8-13).
ORTHOPEDIC GAMUT 8-10 UPPER LUMBAR RADICULOPATHY
HEEL/TOE WALK TEST
Assessment for L5 or S1 Nerve Root Motor Deficiency
Comment
Muscle weakness, atrophy, or the inability to perform functional testing maneuvers all suggest the presence of nerve root compression that is more significant than the alteration of sensation (Table 8-14).
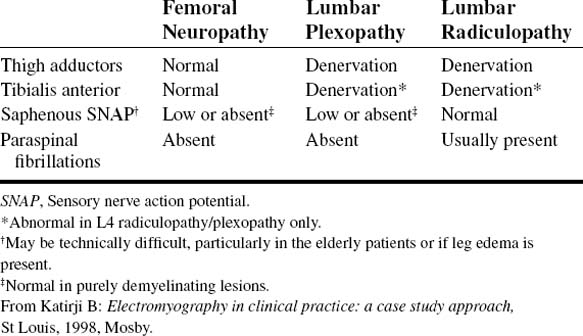
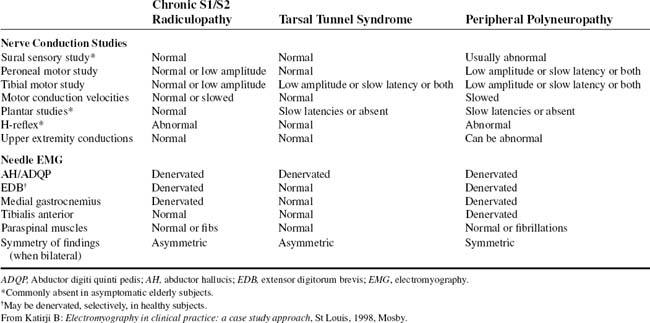
When the leg is shaken, such as during the test for alternating motion rate, the foot will be unstable and flop about. The foot is less floppy with central disorders (upper motor neuron lesions) and may be fixed in plantar flexion. When dorsiflexion of the ankles and toes is weak, the toes of the spastic leg are dragged during walking. Before the examiner concludes that weakness of dorsiflexion is present, the foot should be passively dorsiflexed to be certain that previous weakness, now healed, did not permanently shorten the gastrocnemius. Not unusual is for patients with severe L5 radiculopathy, in whom significant motor axon loss has occurred, to have foot drop (Table 8-15).
TABLE 8-15 ELECTROPHYSIOLOGIC DIFFERENCES BETWEEN L5 RADICULOPATHY AND PERONEAL NEUROPATHY
| L5 Radiculopathy | Peroneal Neuropathy | |
|---|---|---|
| Nerve Conduction Studies | ||
| Peroneal CMAP, recording extensor digitorum brevis | Normal or low amplitude | Conduction block at fibular head, low amplitude, or both |
| Peroneal CMAP, recording tibialis anterior | Normal or low amplitude | Conduction block at fibular head, low amplitude, or both |
| Superficial peroneal SNAP | Normal | Low or absent; normal in deep peroneal or purely demyelinating lesions |
| Needle EMG | ||
| Tibialis anterior | Abnormal | Abnormal |
| Extensor digitorum brevis | Abnormal | Abnormal |
| Extensor hallucis | Abnormal | Abnormal |
| Peroneus longus | Abnormal | Abnormal; normal in selective deep peroneal lesions |
| Tibialis posterior | Abnormal | Normal |
| Flexor digitorum longus | Abnormal | Normal |
| Gluteus medius | May be normal | Normal |
| Tensor fasciae latae | May be normal | Normal |
| Lumbar paraspinals | May be normal | Normal |
CMAP, Compound muscle action potential; EMG, electromyography; SNAP, sensory nerve action potential.
From Katirji B: Electromyography in clinical practice: a case study approach, St Louis, 1998, Mosby.
PROCEDURE
HYPEREXTENSION TEST
Assessment for L3 and L4 Nerve Root Inflammation
ORTHOPEDIC GAMUT 8-12 MODIFIED WILTSE CLASSIFICATION OF LUMBAR SPONDYLOLISTHESIS ETIOLOGY
PROCEDURE
KEMP TEST
Assessment for Intervertebral Nerve Root Encroachment, Muscular Strain, Ligamentous Sprain, or Pericapsular Inflammation
ORTHOPEDIC GAMUT 8-13 MECHANISMS OF LUMBAR FACET PAIN
ORTHOPEDIC GAMUT 8-14 DISC PROLAPSE
Disc prolapse usually follows lifting or twisting while the trunk is in flexion:
PROCEDURE
KERNIG/BRUDZINSKI SIGN
CSF, Cerebral spinal fluid.
PROCEDURE
LASÈGUE DIFFERENTIAL SIGN
Assessment for Intervertebral Radiculopathy Versus Hip Joint Disease
Comment
Examination often reveals restriction of low back motion. Bending toward the affected side typically exacerbates the pain. Variable degrees of local tenderness and muscle guarding are present. In an attempt to relieve tension on the nerve root, the patient may list or bend away from the painful side and stand with the affected hip and knee slightly flexed. A characteristic clinical picture may be present, depending on the level of nerve root involvement (Table 8-16).
ORTHOPEDIC GAMUT 8-16 MODIFIED ALTMAN CLASSIFICATION OF HIP OSTEOARTHRITIS
PROCEDURE
LASÈGUE REBOUND TEST
Assessment for Intervertebral Nerve Root Lesion, Piriformis Muscular Spasm, Ischiotrochanteric Groove Adhesion, or Intervertebral Disc Syndrome
ORTHOPEDIC GAMUT 8-18 DISC HERNIATION VERSUS OTHER CAUSES OF BACK PAIN
PROCEDURE
LASÈGUE SITTING TEST
Assessment for Sciatic Nerve Inflammation
ORTHOPEDIC GAMUT 8-19 ETIOLOGY OF NEUROGENIC CLAUDICATION PAIN
ORTHOPEDIC GAMUT 8-20 LUMBAR CANAL STENOSIS
Electromyographic (EMG) findings in lumbar canal stenosis include the following:
ORTHOPEDIC GAMUT 8-21 LUMBOSACRAL RADICULOPATHY
Electromyographic (EMG) limitations in lumbosacral radiculopathy are as follows:
ORTHOPEDIC GAMUT 8-22 DISTINGUISHING FEATURES OF RESTLESS LEGS SYNDROME
ORTHOPEDIC GAMUT 8-24 DIAGNOSTIC CRITERIA OF RESTLESS LEGS SYNDROME*
PROCEDURE
LASÈGUE TEST
ALSO KNOWN AS LASÈGUE SIGN
Assessment for Sciatica Resulting from Lumbosacral or Sacroiliac Lesions, Lumbar Subluxation Syndrome, Intervertebral Disc Lesion, Spondylolisthesis, Dural Sleeve Adhesions, or Intervertebral Foramen Occlusion (Encroachment)
ORTHOPEDIC GAMUT 8-25 LASÈGUE TEST
Interpretations of the Lasègue test:
ORTHOPEDIC GAMUT 8-26 PRECAUTIONS FOR LASÈGUE TEST
Two precautions to observe in performing Lasègue test:
PROCEDURE
PROCEDURE
PROCEDURE
PROCEDURE
LEWIN SUPINE TEST
Assessment for Lumbar Arthritis, Lumbar Fibrosis, Spondylosis, Sacroiliac or Lumbosacral Arthrosis, or Sciatica
Comment
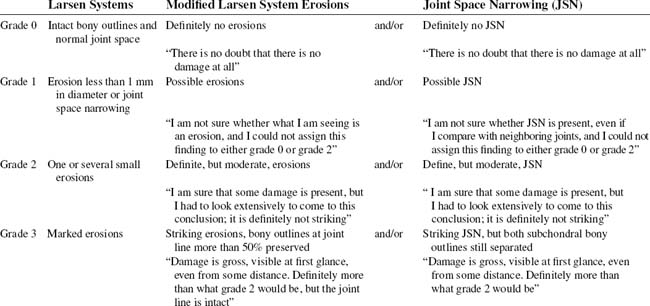
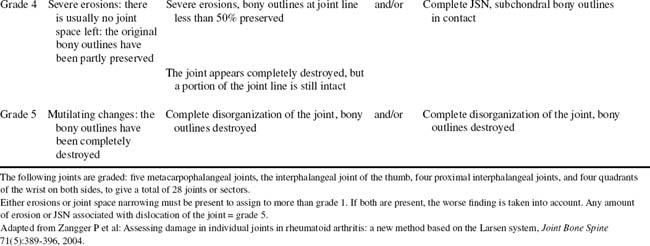
With lumbar spondylosis accompanied by a stenotic lumbar spinal canal, the physical examination is unrevealing despite intermittent symptoms that are often severe. Flexion and straight leg raising are often performed without difficulty. Severe pain during lumbar extension may be the only positive result. Rheumatoid arthritis must be included in the differential diagnoses (Tables 8-18 and 8-19).
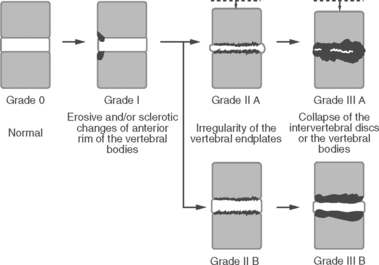 |
Grades II and III are further divided into two types. Type A includes grade IIA (presence of disc narrowing) and grade IIIA (disc space collapsed and vertebral bodies fused), and type B includes grade IIB (absence of disc narrowing) and grade IIIB (vertebral body collapsed but intervertebral disc remains or appears ballooned).
From Sakai T et al: Radiological features of lumbar spinal lesions in patients with rheumatoid arthritis with special reference to the changes around intervertebral discs, Spine J 8(4): 605–611, 2008.
PROCEDURE
LINDNER SIGN
Assessment for Lumbar Nerve Root Irritation or Inflammation
ORTHOPEDIC GAMUT 8-28 UNILATERAL DISC HERNIATION BETWEEN L3 AND L4
ORTHOPEDIC GAMUT 8-29 UNILATERAL DISC HERNIATION BETWEEN L4 AND L5
ORTHOPEDIC GAMUT 8-30 UNILATERAL DISC HERNIATION BETWEEN L5 AND S1
PROCEDURE
MATCHSTICK TEST
Assessment for Denervation Hypersensitivity
Comment
Many cases of acute low back pain that are not correctly identified evolve into a chronic spinal problem with significant disability at the muscular level (Table 8-20). Patients with muscular dysfunction of the lumbar spine can have varying types of clinical findings and case histories.
TABLE 8-20 SITES OF LUMBOPELVIC SOFT-TISSUE SYNDROMES/MYOFASCIAL TRIGGER POINTS
| Diagnosis | Site of Complaint |
|---|---|
| Quadratus lumborum syndrome | Gluteal region, anterior iliac spine, greater trochanter of femur |
| Gluteus maximus or medius syndrome | Sacral and gluteal region, lateral hip |
| Gluteus minimus syndrome | Lateral hip, thigh, and calf |
| Chronic lumbar strain (spinal erector muscles) | Laterally to ribs, caudally toward lumbosacral junction |
| Piriformis syndrome | Sacroiliac region; posterior hip, thigh, calf; possibly sole of foot |
Adapted from Brier SR: Primary care orthopedics, St Louis, 1999, Mosby.
ORTHOPEDIC GAMUT 8-31 MUSCLE SYNDROMES OF THE LUMBOPELVIC SPINE
Common findings in muscle syndromes of the lumbopelvic spine are as follows:
PROCEDURE
MENNELL SIGN
Assessment for Pathologic Involvement of the Sacroiliac Joint Structures
ORTHOPEDIC GAMUT 8-33 SACROILIAC PAIN
The radicular component of sacroiliac pain is referred pain similar to pain associated with:
ORTHOPEDIC GAMUT 8-34 LUMBOPELVIC TENDERNESS
Common areas of palpable lumbopelvic tenderness:
PROCEDURE
MILGRAM TEST
Assessment for Intervertebral Disc Syndrome or Space-Occupying Mass
ORTHOPEDIC GAMUT 8-36 OTHER CAUSES OF SCIATICA
Causes of sciatica not related to disc herniated nucleus pulposus:
ORTHOPEDIC GAMUT 8-37 ACTIVE STRAIGHT-LEG-RAISING TEST
PROCEDURE
PROCEDURE
NACHLAS TEST
PROCEDURE
NERI SIGN
PROCEDURE
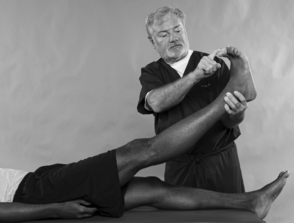
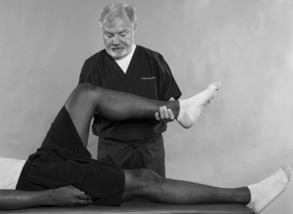
PRONE KNEE-BENDING TEST
Assessment for L2 or L3 Nerve Root Lesion, Femoral Nerve Inflammation, or Quadriceps Muscular Strain
ORTHOPEDIC GAMUT 8-41 FRANK DEGENERATION OF THE FACETS
QUICK TEST
Assessment for Lower Back or Lower Extremity Screening
ORTHOPEDIC GAMUT 8-43 LOW BACK PAIN
Considering low back pain under three headings is helpful:
PROCEDURE
PROCEDURE
SICARD SIGN
Assessment for Sciatic Radiculopathy
Comment
ORTHOPEDIC GAMUT 8-45 DISC FRAGMENT MIGRATION
PROCEDURE
SIGN OF THE BUTTOCK
PROCEDURE
SKIN PINCH TEST
Assessment for Fibrositic Infiltration
ORTHOPEDIC GAMUT 8-47 CAUDA EQUINA SYNDROME
The clinical characteristics of cauda equina syndrome (CES triad of signs) include the following:
PROCEDURE
SPINAL PERCUSSION TEST
Assessment for Osseous or Soft-Tissue Injury in the Lumbar Spine
ORTHOPEDIC GAMUT 8-50 OSTEOPOROTIC COMPRESSION FRACTURE CLASSIFICATION
ORTHOPEDIC GAMUT 8-51 ANTERIOR VERTEBRAL COMPRESSION FRACTURES
Roentgenographic findings in anterior vertebral compression fractures:
PROCEDURE
STRAIGHT-LEG-RAISING TEST
Assessment for Space-Occupying Mass in the Path of a Nerve Root, Sacroiliac Inflammation, and Lumbosacral Involvement
ORTHOPEDIC GAMUT 8-54 UNILATERAL STRAIGHT LEG RAISING
The following are dynamics of unilateral straight leg raising:
PROCEDURE
TURYN SIGN
Assessment for Sciatic Radiculopathy
ORTHOPEDIC GAMUT 8-55 LUMBAR DISC DISEASE CLASSIFICATION
Variation of the lumbar disc disease classification model is as follows:
ORTHOPEDIC GAMUT 8-56 CATEGORIES OF LOW BACK PAIN
ORTHOPEDIC GAMUT 8-59 SCIATICA
PROCEDURE
VANZETTI SIGN
Assessment for Sciatic Scoliosis
ORTHOPEDIC GAMUT 8-60 DEGENERATIVE LUMBAR SCOLIOSIS CLASSIFICATION