Chapter 20 Lumbar Plexus and Sacral Plexus
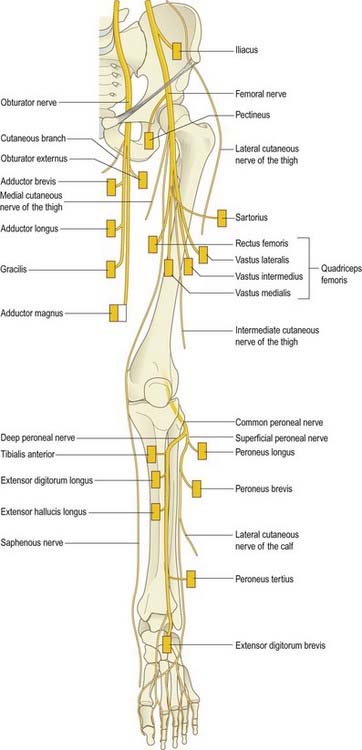
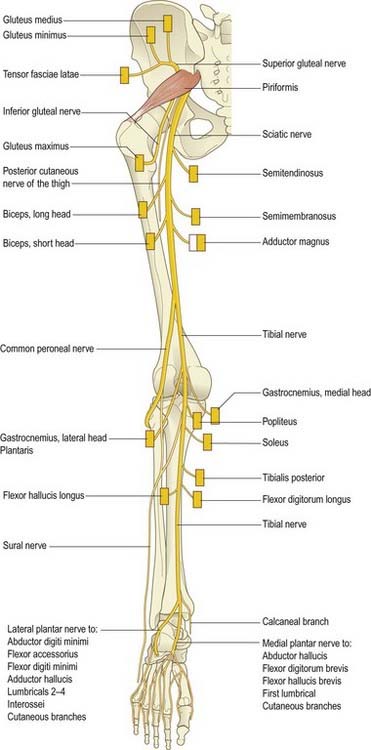
Overview of the Principal Nerves of the Lower Limb (Figs 20.1, 20.2)
Femoral Nerve (L2–4)
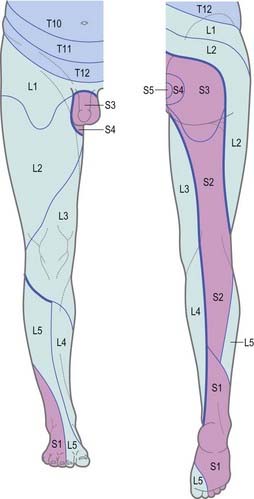
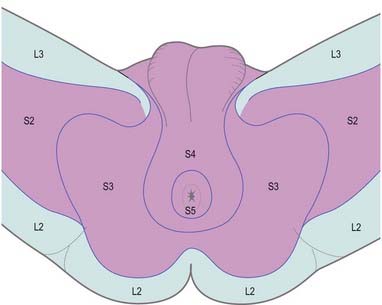
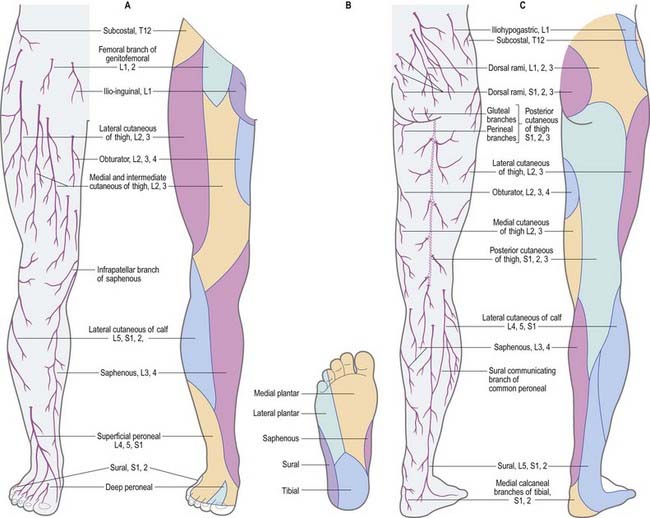
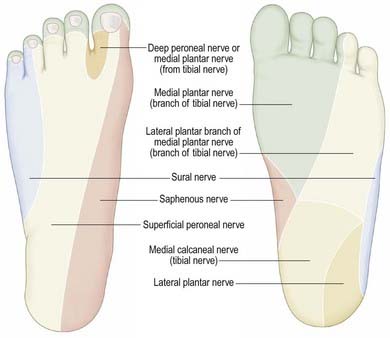
Dermatomes
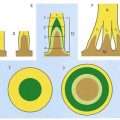
Our knowledge of the extent of individual dermatomes, especially in the limbs, is based largely on clinical evidence. The dermatomes of the lower limb arise from spinal nerves T12 to S3 (Figs 20.3–20.5).
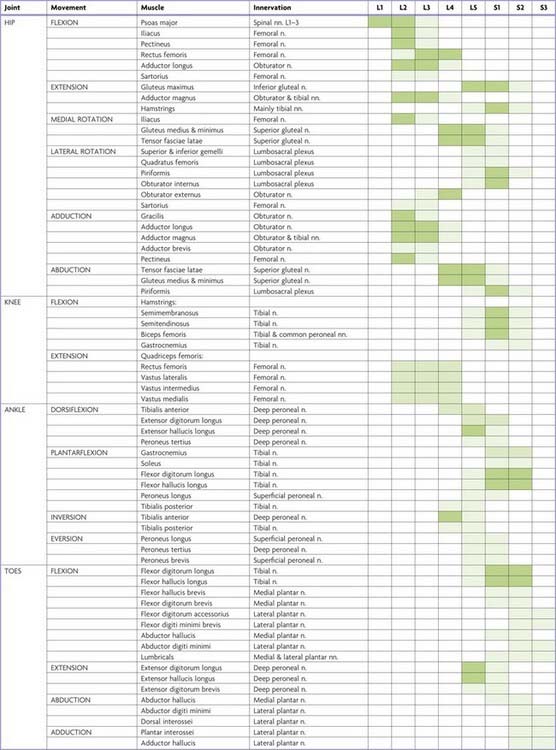
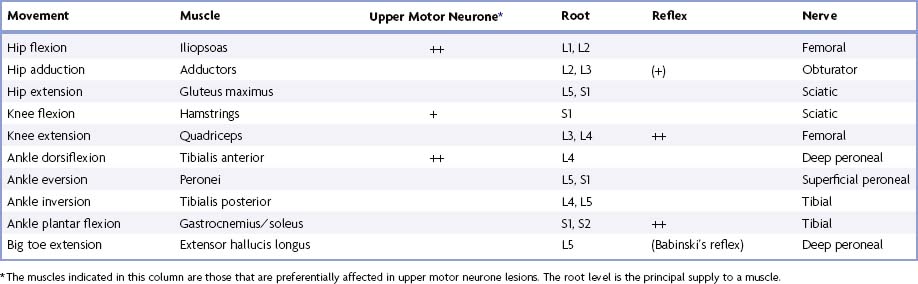
Myotomes
Tables 20.1 to 20.4 summarize the predominant segmental origin of the nerve supply for each of the lower limb muscles and for movements that take place at the joints of the lower limb. Damage to these segments or to their motor roots results in maximal paralysis.
Table 20.1 Movements, muscles and segmental innervation in the lower limb
Table 20.2 Segmental innervation of muscles of the lower limb
| L1 | Psoas major, psoas minor |
| L2 | Psoas major, iliacus, sartorius, gracilis, pectineus, adductor longus, adductor brevis |
| L3 | Quadriceps, adductors (magnus, longus, brevis) |
| L4 | Quadriceps, tensor fasciae latae, adductor magnus, obturator externus, tibialis anterior, tibialis posterior |
| L5 | Gluteus medius, gluteus minimus, obturator internus, semimembranosus, semitendinosus, extensor hallucis longus, extensor digitorum longus, peroneus tertius, popliteus |
| S1 | Gluteus maximus, obturator internus, piriformis, biceps femoris, semitendinosus, popliteus, gastrocnemius, soleus, peronei (longus and brevis), extensor digitorum brevis |
| S2 | Piriformis, biceps femoris, gastrocnemius, soleus, flexor digitorum longus, flexor hallucis longus, some intrinsic foot muscles |
| S3 | Some intrinsic foot muscles (except abductor hallucis, flexor hallucis brevis, flexor digitorum brevis, extensor digitorum brevis) |
Table 20.3 Segmental innervation of joint movements of the lower limb
| Hip | Flexors, adductors, medial rotators | L1–3 |
| Extensors, abductors, lateral rotators | L5, S1 | |
| Knee | Extensors | L3, L4 |
| Flexors | L5, S1 | |
| Ankle | Dorsiflexors | L4, L5 |
| Plantar flexors | S1, S2 | |
| Foot | Inverters | L4, L5 |
| Everters | L5, S1 | |
| Intrinsic muscles | S2, S3 |
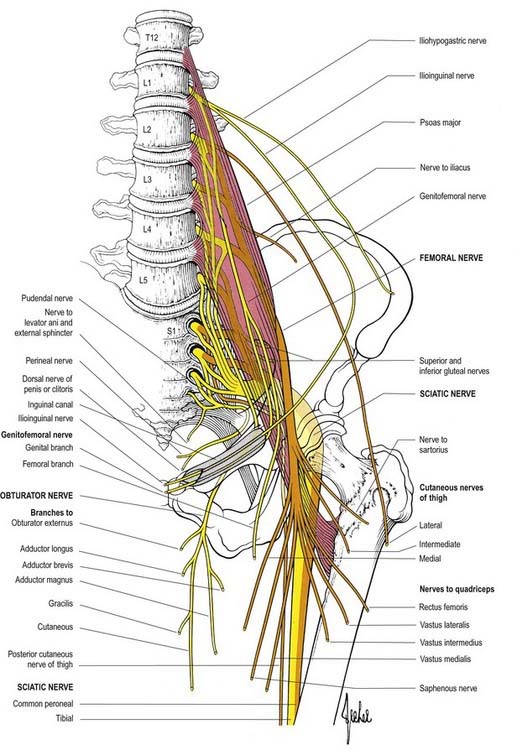
Lumbar Plexus
The posterior abdominal wall contains the origin of the lumbar plexus (Fig. 20.6) and numerous autonomic plexuses and ganglia that lie close to the abdominal aorta and its branches.
Lumbar ventral rami increase in size from first to last and are joined, near their origins, by grey rami communicantes from the four lumbar sympathetic ganglia. These rami, long and slender, accompany the lumbar arteries around the sides of the vertebral bodies, behind psoas major. Their arrangement is irregular: one ganglion may give rami to two lumbar nerves, or one lumbar nerve may receive rami from two ganglia. Rami often leave the sympathetic trunk between ganglia. The first, second and sometimes third lumbar ventral rami are each connected with the lumbar sympathetic trunk by a white ramus communicans. The lumbar ventral rami descend laterally into psoas major. The first three and most of the fourth form the lumbar plexus; the smaller moiety of the fourth joins the fifth as a lumbosacral trunk, which joins the sacral plexus. The fourth is often termed the nervus furcalis, being divided between the two plexuses; however, the third is occasionally the nervus furcalis. Alternatively, both the third and fourth may be furcal nerves, in which case the plexus is termed ‘prefixed.’ More frequently, the fifth nerve is furcal, and the plexus is then termed ‘postfixed.’ These variations modify the sacral plexus.
| Muscular | T12, L1–4 |
| Iliohypogastric | L1 |
| Ilioinguinal | L1 |
| Genitofemoral | L1, L2 |
| Lateral femoral cutaneous | L2, L3 |
| Femoral | L2–4 dorsal divisions |
| Obturator | L2–4 ventral divisions |
| Accessory obturator | L2, L3 |
Division of constituent ventral rami into ventral and dorsal branches is not as clear in the lumbar and lumbosacral plexuses as it is in the brachial plexus. Anatomically, the obturator and tibial nerves (via the sciatic) arise from ventral divisions, and the femoral and peroneal nerves (via the sciatic) arise from dorsal divisions. Lateral branches of the twelfth thoracic and first lumbar ventral rami are drawn into the gluteal skin, but otherwise, these nerves are typical. The second lumbar ramus is difficult to interpret. It not only contributes substantially to the femoral and obturator nerves but also has an anterior terminal branch (genital branch of the genitofemoral) and a lateral cutaneous branch (lateral femoral cutaneous nerve and femoral branch of the genitofemoral). Anterior terminal branches of the third to fifth lumbar and first sacral rami are suppressed, but the corresponding parts of the second and third sacral rami supply the skin of the perineum.
Muscular Branches
Small branches are derived from all five lumbar roots.
Iliohypogastric Nerve
Distribution
The iliohypogastric nerve originates from the L1 ventral ramus. It emerges from the upper lateral border of psoas major and crosses obliquely behind the lower renal pole and in front of quadratus lumborum. Above the iliac crest it enters the posterior part of transversus abdominis. Between transversus abdominis and internal oblique, it divides into lateral and anterior cutaneous branches and also supplies both muscles. The lateral cutaneous branch runs through the internal and external oblique above the iliac crest, a little behind the iliac branch of the twelfth thoracic nerve, and is distributed to the posterolateral gluteal skin. The anterior cutaneous branch runs between and supplies the internal oblique and transversus abdominis. It runs through the internal oblique approximately 2 cm medial to the anterior superior iliac spine and through the external oblique aponeurosis approximately 3 cm above the superficial inguinal ring; it is then distributed to the suprapubic skin. The iliohypogastric nerve connects with the subcostal and ilioinguinal nerves (see Fig. 19.3). It is occasionally injured during an oblique surgical approach to the appendix. However, because the suprapubic skin is innervated from several sources, there is rarely any detectable sensory loss. Division of the iliohypogastric nerve above the anterior superior iliac spine may weaken the posterior wall of the inguinal canal and predispose to the formation of a direct hernia.
Lateral Femoral Cutaneous Nerve of the Thigh
The lateral (femoral) cutaneous nerve of the thigh arises from the dorsal branches of the second and third lumbar ventral rami and emerges from the lateral border of psoas major, crossing the iliacus obliquely toward the anterior superior iliac spine. It supplies the parietal peritoneum in the iliac fossa. The right nerve passes posterolateral to the caecum, separated from it by the fascia iliaca and peritoneum; the left passes behind the lower part of the descending colon. Both pass behind or through the inguinal ligament, variably medial to the anterior superior iliac spine (commonly about 1 cm) and anterior to or through sartorius into the thigh, where they divide into anterior and posterior branches. The anterior branch becomes superficial approximately 10 cm distal to the anterior superior iliac spine and supplies the skin of the anterior and lateral thigh as far as the knee. It connects terminally with the cutaneous branches of the anterior division of the femoral nerve and the infrapatellar branch of the saphenous nerve, forming the peripatellar plexus. The posterior branch pierces the fascia lata higher than the anterior, and it divides to supply the skin on the lateral surface from the greater trochanter to about mid thigh. It may also supply the gluteal skin (see Case 2).
Femoral Nerve
The femoral nerve (Fig. 20.7), the largest branch of the lumbar plexus, arises from the dorsal branches (posterior divisions) of the second to fourth lumbar ventral rami. It descends through psoas major, emerging low on its lateral border, and then passes between psoas and iliacus, deep to the iliac fascia. Passing behind the inguinal ligament into the thigh, it splits into anterior and posterior divisions. Behind the inguinal ligament it is separated from the femoral artery by part of psoas major. In the abdomen the nerve supplies small branches to iliacus and pectineus and a branch to the proximal part of the femoral artery; the latter branch sometimes arises in the thigh.
Posterior Division of the Femoral Nerve
The saphenous nerve (see Fig. 20.7) is the largest cutaneous branch of the femoral nerve. It descends lateral to the femoral artery into the adductor canal, where it crosses anteriorly to become medial to the artery. At the distal end of the canal it leaves the artery and emerges through the aponeurotic covering with the saphenous branch of the descending genicular artery. As it leaves the adductor canal it gives off an infrapatellar branch that contributes to the peripatellar plexus and then pierces the fascia lata between the tendons of sartorius and gracilis, becoming subcutaneous to supply the prepatellar skin. It descends along the medial tibial border with the long saphenous vein and divides distally into one branch that continues along the tibia to the ankle and another branch that passes anterior to the ankle to supply the skin on the medial side of the foot, often as far as the first metatarsophalangeal joint. The saphenous nerve connects with the medial branch of the superficial peroneal nerve. Near mid thigh, it gives a branch to the subsartorial plexus (see below). The nerve may be subject to an entrapment neuropathy as it leaves the adductor canal.
Vascular branches of the femoral nerve supply the femoral artery and its branches.
CASE 3 Femoral Neuropathy
Originating in the upper lumbosacral plexus, the femoral nerve travels through psoas major, passing low and deep between psoas and iliacus, then behind the inguinal ligament, separated from the femoral artery by a part of the psoas major. Involvement of the femoral nerve may result from a retroperitoneal haemorrhage or, as in this case, may reflect a diabetic mononeuropathy (compare with Case 4, Proximal Diabetic Amyotrophy). Compression at the inguinal ligament by external or internal pressure can also result in femoral neuropathy.
Obturator Nerve
Anterior Branch
The anterior branch (see Fig. 20.7) leaves the pelvis anterior to obturator externus, descending in front of adductor brevis and behind pectineus and adductor longus. At the lower border of adductor longus it communicates with the medial cutaneous and saphenous branches of the femoral nerve, forming a subsartorial plexus that supplies the skin on the medial side of the thigh. It descends on the femoral artery, which its termination supplies. Near the obturator foramen, the anterior branch supplies the hip joint. Behind the pectineus, it supplies adductor longus, gracilis, usually adductor brevis and often pectineus, and it connects with the accessory obturator nerve when it is present. Occasionally the communicating branch to the femoral medial cutaneous and saphenous branches continues as a cutaneous branch to the thigh and leg, emerging from behind the distal border of adductor longus to descend along the posterior margin of sartorius to the knee, where it pierces the deep fascia, connects with the saphenous nerve and supplies the skin halfway down the medial side of the leg.
Posterior Branch
The posterior branch pierces obturator externus anteriorly, supplies it and passes behind adductor brevis to the front of adductor magnus, dividing into branches to this and adductor brevis when the latter is not supplied by the anterior division. It usually sends an articular filament to the knee joint, which perforates adductor magnus distally or traverses its opening with the femoral artery to enter the popliteal fossa. There it descends on the popliteal artery to the back of the knee, pierces its oblique posterior ligament and supplies the articular capsule. It gives filaments to the popliteal artery.
Sacral Plexus
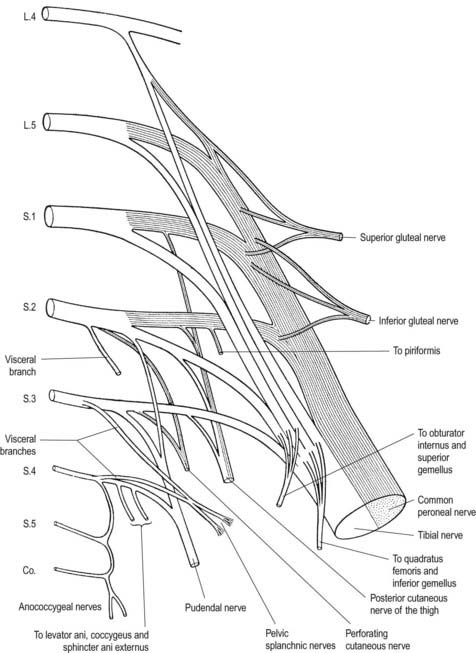
The sacral plexus provides the nerve supply to the pelvis and lower limb in addition to part of the autonomic supply to the pelvic viscera. It gives origin to the sciatic, inferior gluteal, superior gluteal and pudendal nerves, in addition to the nerves to quadratus femoris, obturator internus and the posterior cutaneous nerve of the thigh (Fig. 20.8).
| Ventral Divisions | Dorsal Divisions | |
|---|---|---|
| To quadratus femoris and gemellus inferior | L4, L5, S1 | |
| To obturator internus and gemellus superior | L5, S1, S2 | |
| To piriformis | (S1), S2 | |
| Superior gluteal | L4, L5, S1 | |
| Inferior gluteal | L5, S1, S2 | |
| Posterior femoral cutaneous | S2, S3 | S1, S2 |
| Tibial (sciatic) | L4, L5, S1, S2, S3 | |
| Common peroneal (sciatic) | L4, L5, S1, S2 | |
| Perforating cutaneous | S2, S3 | |
| Pudendal | S2, S3, S4 | |
| To levator ani, coccygeus and sphincter ani externus | S4 | |
| Pelvic splanchnic | S2, S3, (S4) |
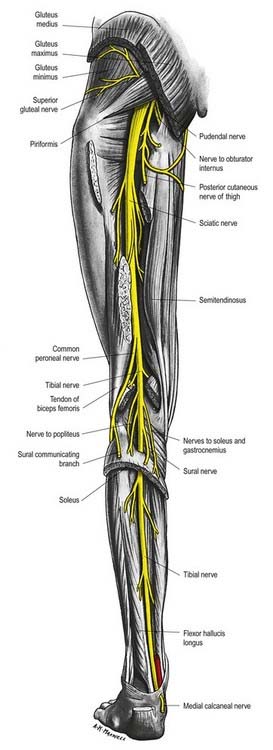
Sciatic Nerve
The sciatic nerve is 2 cm wide at its origin and is the thickest nerve in the body (Fig. 20.9). It leaves the pelvis via the greater sciatic foramen below piriformis and descends between the greater trochanter and the ischial tuberosity and along the back of the thigh, dividing into the tibial and common peroneal (fibular) nerves at a varying level proximal to the knee. Superiorly, it lies deep to gluteus maximus, resting first on the posterior ischial surface with the nerve to quadratus femoris between them. It then crosses posterior to obturator internus, the gemelli and quadratus femoris, separated by the last from obturator externus and the hip joint. It is accompanied medially by the posterior femoral cutaneous nerve and the inferior gluteal artery. More distally, it lies behind adductor magnus and is crossed posteriorly by the long head of biceps femoris. It corresponds to a line drawn from just medial to the midpoint between the ischial tuberosity and the greater trochanter to the apex of the popliteal fossa.
The point of division of the sciatic nerve into its major components (tibial and common peroneal) is very variable. A common site is at the junction of the middle and lower thirds of the thigh, near the apex of the popliteal fossa. The division may occur at any level above this, but rarely below it. It is not uncommon for the major components to leave the sacral plexus separately, in which case the common peroneal component usually passes through piriformis at the greater sciatic notch, while the tibial component passes below the muscle.
Lesions of the Sciatic Nerve
CASE 5 Sciatica
Discussion: Sciatica is a term used to describe pain radiating down the leg, with or without back pain. It is most commonly associated with nerve root compression at L5 or S1. The most frequent cause of acute sciatica is disc herniation. L5 and S1 roots are most commonly compressed; both roots can be involved in dorsolateral or central disc herniation, with the disc compressing the roots in the lateral recess. A large and more lateral herniation may result in only a single root being compressed, usually within the intervertebral foramen. Owing to mixed root innervation to lower extremity muscles, motor and sensory symptoms and signs do not always precisely match the root injured. Sensory loss in the foot (lateral foot and fifth toe involvement) indicates S1 localization (Fig. 20.10), but in some instances, sensation is normal. Straight leg raising increases symptoms by stretching the roots already compromised. Loss of the Achilles reflex with a normal patellar reflex is typical of an S1 root lesion.
Tibial Nerve
Branches
Muscular Branches
Proximal muscular branches arise between the heads of gastrocnemius and supply gastrocnemius, plantaris, soleus and popliteus. The nerve to soleus enters its superficial aspect. The branch to popliteus descends obliquely across the popliteal vessels, curling around the distal border of the muscle to its anterior surface. It also supplies tibialis posterior, the proximal tibiofibular joint and the tibia and gives off an interosseous branch that descends near the fibula to reach the distal tibiofibular joint.
Muscular branches in the leg, either independently or by a common trunk, supply soleus (on its deep surface), tibialis posterior, flexor digitorum longus and flexor hallucis longus. The branch to flexor hallucis longus accompanies the peroneal vessels.
Common Peroneal Nerve
Deep Peroneal Nerve
The deep peroneal nerve (deep fibular nerve) begins at the common peroneal bifurcation, between the fibula and the proximal part of peroneus longus. It passes obliquely forward, deep to extensor digitorum longus, to the front of the interosseous membrane and reaches the anterior tibial artery in the proximal third of the leg. It descends with the artery to the ankle, dividing there into lateral and medial terminal branches. It is first lateral to the artery, then anterior and again lateral at the ankle.
Sural Nerve
The sural nerve arises from the tibial nerve and descends between the heads of gastrocnemius, pierces the deep fascia proximally in the leg and is joined at a variable level by the sural communicating branch of the common peroneal nerve (Fig. 20.2). Some authors term this branch the lateral sural cutaneous nerve, and they call the main trunk (from the tibial nerve) the medial sural cutaneous nerve. The sural nerve descends lateral to the calcaneal tendon, near the short saphenous vein, to the region between the lateral malleolus and the calcaneus and supplies the posterior and lateral skin of the distal third of the leg. It then passes distal to the lateral malleolus along the lateral side of the foot and little toe, supplying the overlying skin. It connects with the posterior femoral cutaneous nerve in the leg and with the superficial peroneal nerve on the dorsum of the foot. The surface marking at the ankle is a line parallel to the calcaneal tendon halfway between the tendon and the lateral malleolus. However, its position is variable, and it is at risk from any surgery in this region. Rather like the radial nerve at the wrist, the sural nerve has a tendency to form painful neuromas. The nerve is harvested for grafting on occasion because it is sensory only, superficial, and easily identified.
Posterior Cutaneous Nerve of the Thigh
The posterior cutaneous nerve of the thigh arises from the dorsal branches of the first and second sacral rami and the ventral branches of the second and third sacral rami. It leaves the pelvis via the greater sciatic foramen below piriformis and descends under gluteus maximus with the inferior gluteal vessels, lying posterior or medial to the sciatic nerve. It descends in the back of the thigh superficial to the long head of biceps femoris, deep to the fascia lata. Behind the knee it pierces the deep fascia and accompanies the short saphenous vein to midcalf, its terminal twigs connecting with the sural nerve. Its branches are all cutaneous and are distributed to the gluteal region, perineum and flexor aspect of the thigh and leg. Three or four gluteal branches curl around the lower border of gluteus maximus to supply the skin over its inferolateral area. The perineal branch supplies the superomedial skin in the thigh, curves forward across the hamstrings below the ischial tuberosity, pierces the fascia lata and runs in the superficial perineal fascia to the scrotal or labial skin, communicating with the inferior rectal and posterior scrotal branches of the perineal nerve. It gives numerous branches to the skin of the back and medial side of the thigh, the popliteal fossa and the proximal part of the back of the leg.
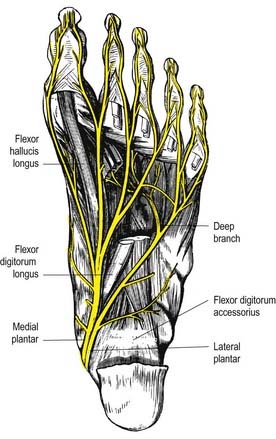
Innervation of the Foot
Tibial Nerve
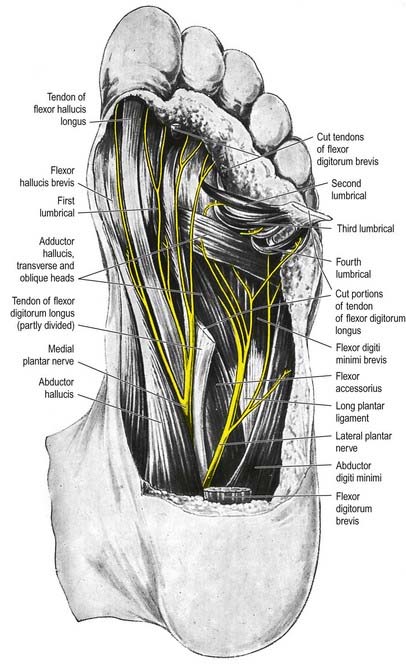
Medial Plantar Nerve
The medial plantar nerve (Fig 20.11) is the larger terminal division of the tibial nerve, and it lies lateral to the medial plantar artery. From its origin under the flexor retinaculum, it passes deep to abductor hallucis, then appears between it and flexor digitorum brevis, gives off a medial proper digital nerve to the hallux and divides near the metatarsal bases into three common plantar digital nerves.
Lateral Plantar Nerve
The lateral plantar nerve (see Fig. 20.11) supplies the skin of the fifth toe, the lateral half of the fourth toe and most of the deep muscles of the foot. Its distribution therefore closely resembles that of the ulnar nerve in the hand. It passes laterally forward, medial to the lateral plantar artery, toward the tubercle of the fifth metatarsal. It next passes between flexor digitorum brevis and accessorius and ends between brevis and abductor digiti minimi by dividing into superficial and deep branches. Before division, it supplies flexor digitorum accessorius and abductor digiti minimi and gives rise to small branches that pierce the plantar fascia to supply the skin of the lateral part of the sole (Fig. 20.12). The superficial branch splits into two common plantar digital nerves: the lateral supplies the lateral side of the fifth toe, flexor digiti minimi brevis and the two interossei in the fourth intermetatarsal space; the medial connects with the third common plantar digital branch of the medial plantar nerve and divides into two to supply the adjoining sides of the fourth and fifth toes. The deep branch accompanies the lateral plantar artery deep to the flexor tendons and adductor hallucis and supplies the second to fourth lumbricals, adductor hallucis and all interossei (except those of the fourth intermetatarsal space). Branches to the second and third lumbricals pass distally, deep to the transverse head of adductor hallucis, and curl around its distal border to reach them (Fig. 20.13).
Nerve Entrapment Syndromes in the Foot
Any nerve of the foot can be affected by entrapment, classically leading to a burning sensation in the distribution of that nerve. Tarsal tunnel syndrome (see Case 6) is much less common than carpal tunnel syndrome. The flexor retinaculum can compress the tibial nerve or either of its branches (medial and lateral plantar nerves), but it is most commonly compressed by a space-occupying lesion (e.g. ganglion), a leash of vessels or the deep fascia associated with abductor hallucis. Compression of the first branch of the lateral plantar nerve by the deep fascia of abductor hallucis can lead to heel pain. The medial plantar nerve can be irritated at the master knot of Henry; this is usually related to jogging. The superficial peroneal nerve can be damaged in severe inversion injuries of the ankle, and the deep peroneal nerve is sometimes compressed by osteophytes in the region of the second tarsometatarsal joint. Sural nerve entrapment does not occur from compression by fascial elements; rather, it follows trauma and subsequent scar formation around the nerve. Entrapment of the common digital nerve as it passes under the intermetatarsal ligament of the third (or, less commonly, second) web space can result in Morton’s neuroma, which is probably the most common form of nerve entrapment in the foot.
Innervation of the Pelvis
Innervation of the Perineum
Inferior Rectal Nerve
The inferior rectal nerve runs through the medial wall of the pudendal canal with the inferior rectal vessels. It crosses the ischioanal fossa to supply the external anal sphincter, the lining of the lower part of the anal canal and the circumanal skin. It frequently breaks into terminal branches just before reaching the lateral border of the sphincter. Its cutaneous branches distributed around the anus overlap the perineal branch of the posterior femoral cutaneous nerve and the scrotal or labial nerves. The inferior rectal nerve occasionally arises directly from the sacral plexus and crosses the sacrospinous ligament or reconnects with the pudendal nerve. In females the inferior rectal nerve may supply sensory branches to the lower part of the vagina.