Chapter 15 Lower Limb Orthotic Devices
An orthosis is defined as a device attached or applied to the external surface of the body to improve function, restrict or enforce motion, or support a body segment.38 Lower limb orthoses are indicated to assist gait, reduce pain, decrease weight-bearing, control movement, and minimize progression of a deformity. Lower limb orthoses assist nonambulatory patients with transfer and mobility skills and assist ambulatory patients in becoming safe walkers. Ambulation aids can be used in combination with lower limb orthoses to help patients ambulate more safely. Ambulation aids represent extensions of the upper limb but are discussed in this chapter because of their importance in gait.
Principles of Lower Limb Orthoses
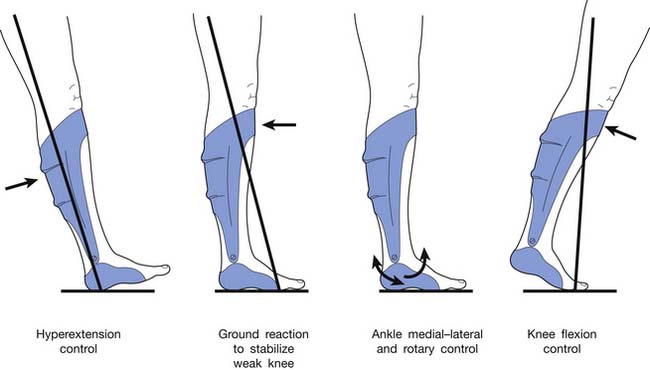
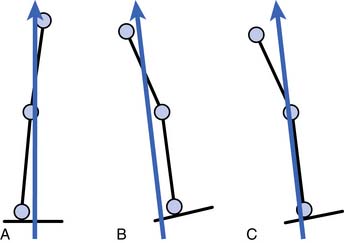
Orthoses should be used for the specific management of selected disorders. As in all fields of medicine, specific treatment should be based on a specific medical diagnosis, with an established goal of treatment.56 Placement of orthotic joints should approximate anatomic joints. Box 15-1 outlines this principle as well as other common lower limb orthotic principles. Most orthoses use a three-point system to ensure proper positioning of the limb within the orthosis.27 For example, a knee that has a tendency to hyperextend, or “back knee,” can be treated with a knee orthosis that applies force posterior to the knee but also applies forces anteriorly along the leg and the thigh. Such an orthosis ensures adequate control of the knee by exerting these forces proximal to, distal to, and at the knee joint.
Shoes
The purpose of wearing shoes is to protect the feet. The normal foot does not require support from shoes. The sole should be pliable so as not to interfere with the normal biomechanics of the foot. A practical way of ensuring that a shoe is of adequate length is to determine whether the index finger can be placed between the tip of the great toe and the toe box.58 The presence of calluses indicates areas of friction from poorly fitting (loose) shoes. The presence of corns indicates areas of friction over bony prominences, most often caused by tight-fitting shoes. Leather shoes are good choices for all types of activity. They are durable, allow ventilation, and mold to the feet with time. A good pair of shoes can often eliminate the need for foot orthoses and should be considered before orthotic prescription.
Shoe Parts
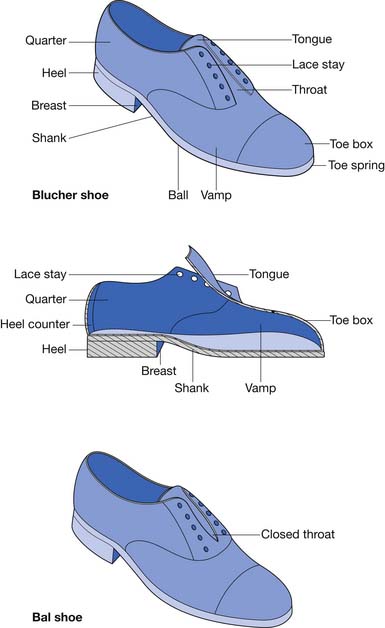
Two types of dress shoes are commonly worn: the Blucher and the Bal (Figure 15-1). The tongue is part of the vamp in the Blucher shoe. The quarters overlap the vamp. A Blucher shoe is recommended for patients requiring an orthosis because there is more room to don and doff the shoe and the orthosis because of the open throat.63 In the Bal shoe style the quarters meet at the throat. The vamp is stitched over the quarters at the throat, thereby limiting the ability of the shoe to open and accommodate an orthosis.
Foot Orthoses
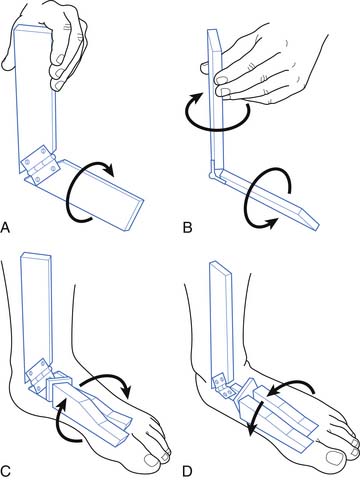
Foot orthoses range from arch supports found at a local pharmacy or athletic store to customized orthoses fabricated by an orthotist. The effectiveness of an orthosis depends on proper diagnosis of the foot condition, the appropriate selection of orthotic material, and proper molding. Foot orthoses affect the ground reactive forces acting on the joints of the lower limb. They also have an effect on rotational components of gait (Figure 15-2).
Mild conditions can be treated with over-the-counter orthoses. More severe problems and chronic medical conditions require customized orthoses.61 These are available in three types. A soft type is most commonly used in over-the-counter orthoses. Orthotists usually provide semirigid orthoses, which provide more support than the soft type but are still shock absorbing. A rigid orthosis is indicated only for a problem that requires aggressive bracing to control a deformity.
To make a custom foot orthosis, the subtalar joint should be placed in a neutral position before casting. This position minimizes abnormalities related to foot and ankle rotation, such as hyperpronation, and it is also the position in which the foot functions best.41 The subtalar neutral position is used to treat conditions associated with hyperpronation including pes planus, patellofemoral pain.9,48 The foot is then covered with a parting agent such as stockinette or a clear plastic wrap. The foot is then wrapped in either plaster of Paris strips or fiberglass tape and allowed to harden. Fiberglass casting is also used for difficult orthotic cases where the fiberglass casting itself can be used as a temporary orthosis to determine whether the mold properly controls the deformity. This negative mold is then removed to allow a positive mold to be made from the negative mold. The positive mold can be modified to increase the effectiveness of the orthosis. The custom orthosis is obtained by heating and form-fitting (often by use of a vacuum) the plastic to the positive mold.
Common Foot Conditions
Pes Planus (Flat Foot)
Symptomatic relief of pain is obtained by controlling excess pronation of the foot. Pronation of the foot can be defined as a rotation of the foot in the longitudinal axis resulting in a lowering of the medial aspect of the foot. Foot pronation is a component of eversion. Eversion involves pronation at the subtalar joint, dorsiflexion at the ankle joint, and abduction of the forefoot at the tarsometatarsal joints. The key to controlling excess pronation is controlling the calcaneus to keep the subtalar joint in a neutral position.
Pes planus can be due to abnormalities such as excessive internal torsion of the tibia (which results in pronation of the foot) or malalignment of the calcaneus. It is the interaction between the tibia and the foot at the subtalar joint that allows pathology outside the foot to cause inrolling of the foot (see Figure 15-2).
The reduction of pronation is accomplished by maintaining the calcaneus and the subtalar joint in correct alignment. The subtalar joint should be in a neutral position during the custom molding process. The subtalar joint neutral position prevents rotational deformities associated with excessive pronation or supination from occurring (see Figure 15-2, C and D). Elevation of the anteromedial calcaneus exerts an upward thrust against the sustentaculum tali to help prevent inrolling.6 The orthosis should extend beyond the metatarsal heads to provide better leverage for control of the deformity. A custom-made foot orthosis designed to prevent hyperpronation is also referred to as a UCBL orthosis (or UCB), denoting the University of California Biomechanics Laboratory, where original work regarding this type of orthosis was performed in the 1940s. There are two common mistakes noted in custom foot orthoses. First, some are not made by orthotists, who represent the profession best capable of making a proper foot orthosis. Second, some custom foot orthoses do not cup the calcaneus but rather merely serve as a platform to stand on. The orthosis must extend proximally enough on the calcaneus to cup and control the subtalar joint during gait.
Some cases of pes planus are due to ligamentous laxity within the foot. For these cases a medial longitudinal arch support can be helpful for alleviating pain. Initial use of an arch that is too high can cause discomfort. The height of the arch can be increased as necessary as the foot develops a tolerance for the inlay. A Thomas heel extension (term for increased medial length to heel) can also offer medial support, particularly for heavier individuals. A most practical piece of advice for runners who have hyperpronation or pes planus is to purchase a pair of running shoes with a firm medial heel counter as well as shoes with a wide last at the shank (see Figure 15-1). Each of these applications helps prevent pronation at the subtalar joint.
Pes Cavus (High-Arched Foot)
A typical complication of pes cavus is excess pressure along the heel and metatarsal head areas, which can lead to pain. This can be prevented by making the height of the longitudinal support just high enough to fill in the space between the shank of the shoe and the arch of the foot to distribute weight more effectively. Weight should also be evenly distributed over the metatarsal heads. The lift is extended just to the metatarsal head area to help distribute and alleviate pressure over the metatarsal weight-bearing area. The high point of the arch is located at the talonavicular joint because there is no tendency to pronate as in pes planus. If the tibia is externally rotated (see Figure 15-2), this can give the appearance of an elevated arch as the foot supinates and the lateral aspect of the foot assumes additional weight-bearing responsibility. In these cases a foot orthosis is custom molded with the subtalar joint in a neutral position to prevent excess supination from occurring.
Forefoot Pain (Metatarsalgia)
Relief of pain in the forefoot is accomplished by distributing the weight-bearing forces to an area proximal to the metatarsal heads. This can be done by either internal or external modification. A metatarsal pad (also referred to as a “cookie”) can be placed inside the shoe just proximal to the second, third, and fourth metatarsal heads. It should also be just proximal to the lateral aspect of the first metatarsal head and medial to the fifth metatarsal head (Figure 15-3). A metatarsal bar is recommended for cases in which the foot is too sensitive to tolerate a pad inside the shoe. The metatarsal bar is typically ¼-inch thick and tapers distally. The distal edge should be proximal to the metatarsal heads. It is often applied to a leather or neoprene sole.35 The metatarsal bar can also be used for forefoot pain associated with pes cavus. A rocker bottom (Figure 15-4) can also be used for metatarsalgia to decrease the force on the metatarsal pad region at push off.
Prevention of forefoot pain should also be emphasized to patients. Patients should avoid shoes with high heels or pointed toes, which place excess stress on the metatarsal heads.4
Heel Pain
The painful area can be alleviated by using an orthosis to help distribute weight. Rubber heel pads can be applied inside the shoe to offer relief in cases of minor discomfort. A calcaneal bar is recommended for cases in which the foot is too sensitive to tolerate a pad inside the shoe and the heel pain is associated with a chronic condition. The calcaneal bar is placed distal to the painful area to prevent the calcaneus from assuming full weight-bearing status. The same can be accomplished with a shoe that has a spring for the heel set on the anterior calcaneus (see Figure 15-4, A). The application of a rocker bottom shoe can also be used to help initiate heel strike anterior and the ground reaction force anterior to the painful calcaneus (see Figure 15-4, B). Both of these shoe types are now commercially available.
A common cause of heel pain along the anteromedial calcaneus is plantar fasciitis. Pain occurs at the attachment site of the fascia along the medial aspect of the heel.39 Point tenderness is located over the anteromedial calcaneus. It is common in people who hyperpronate their feet, thereby placing excess stress on the medial longitudinal arch. A custom-made orthosis with the subtalar joint in a neutral position (such as that described for pes planus) helps prevent excessive inrolling from occurring and reduces the stress placed along the proximal arch. A custom-made UCB orthosis is indicated for cases in which conservative treatment has failed. From an orthotic standpoint, conservative treatment should include the use of a pair of shoes with a firm medial heel counter and a wide shank (see Figure 15-1).
An additional orthotic intervention for plantar fasciitis is the application of a plantar fascia night splint, which is a prefabricated AFO placed in a few degrees of dorsiflexion.16,42 This helps provide the plantar fascia and plantar flexors a therapeutic stretch during sleep hours, assuring the patient several hours of passive stretching daily. Such a device is recommended for as long as is necessary until the patient is asymptomatic (Figure 15-5).
Heel spurs are frequently mistaken as the source of heel pain. Heel spurs related to plantar fasciitis are the result of mechanical stress acting through the plantar fascia onto its origin at the calcaneus and are not the source of the pain.34 Inferior heel spurs are related to advancing age and are not painful in nature.
Osteoarthritis of the Knee
Although osteoarthritis of the knee is not a foot condition, it is mentioned here because pain related to it can be alleviated with foot orthoses. Foot orthoses alter the ground reaction forces affecting the more proximal joints, such as the knee, and this relationship should be considered when prescribing a foot orthosis. Lateral heel wedges can be used for conservative treatment of osteoarthritis when medial compartment narrowing is present. The heel wedges used are ¼-inch thick along the lateral border and taper medially. Relief was obtained with heel wedges in 74 of 121 knees from 85 patients in one study.15 Relief of pain was most frequently obtained in patients with mild osteoarthritis, but it was also documented in some patients with complete obliteration of the medial joint space. Wedge use widened the gait pattern. This orthosis has not been studied in patients with medial meniscus injuries, but it might afford some pain relief with medial compartment unloading.
Pediatric Shoes
It is a common misconception that all flat feet need to be treated in children. Flat feet are usual in infants, common in children, and occur occasionally in adults.50 Flat feet improve over time, in part because of the loss of subcutaneous fat and the reduction of laxity of the joints that occur with growth50 and the maturation of the gait pattern. Intensive treatment with corrective shoes or inserts for a 3-year period did not alter the natural history of flat feet in 129 children who were 1 to 6 years of age.58 One cannot make the asymptomatic person feel any better. Frequent shoe size change is necessary in the first few years of life.59
Ankle-Foot Orthoses
AFOs are the most commonly prescribed lower limb orthoses. They were formerly known decades ago as short leg braces. Metal or plastic AFOs can be used effectively to control ankle motion. Metal AFOs are relatively contraindicated in children because the weight of the brace can cause external tibial rotation. Plastic AFOs are now most common in all age-groups.
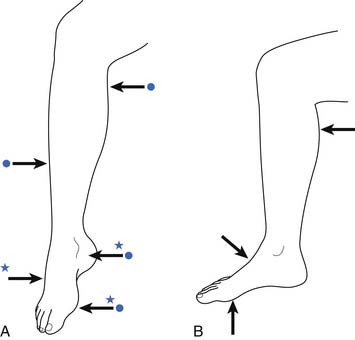
AFOs should provide mediolateral stability as a safety feature.17 Although much emphasis with AFOs is placed on controlling the amount of dorsiflexion and plantar flexion, movements at the subtalar joint also significantly influence the biomechanics of gait. Inversion includes supination at the subtalar joint, adduction at the tarsometatarsal joints, and plantar flexion at the ankle joint, which results in the foot being in an equinovarus position. Eversion includes pronation at the subtalar joint, abduction of the forefoot at the tarsometatarsal joints, and dorsiflexion at the ankle joint, resulting in the foot being in a valgus position. Rotation at the subtalar joint is also accompanied by rotation of the tibia (see Figure 15-2).
AFOs can also stabilize the knee during gait.23 They are prescribed for conditions affecting knee stability, such as genu recurvatum. An AFO should be considered for conditions affecting the knee, particularly when a concurrent problem exists at the ankle or subtalar joints. A proper AFO prescription considers the biomechanical influence of the orthosis at the foot, ankle, and knee in all planes of movement. It is very important to remember that plantar flexion creates a knee extension moment and dorsiflexion creates a knee flexion moment.
Metal Ankle-Foot Orthoses
Recent research has offered support that metal AFOs provide better stabilization of the ankle during the gait cycle.8
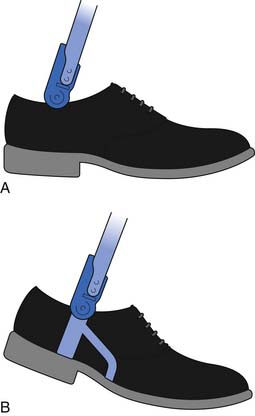
The metal AFO consists of a proximal calf band, two uprights, ankle joints, and an attachment to the shoe to anchor the AFO (Figure 15-6). The posterior metal portion of the calf band should be 1.5 to 3 inches wide to adequately distribute pressure.11 The calf band should be 1 inch below the fibular neck to prevent a compressive common peroneal nerve palsy. A leather strap with Velcro is used to close the calf band, because it provides ease of closure for patients with only one functional upper limb.
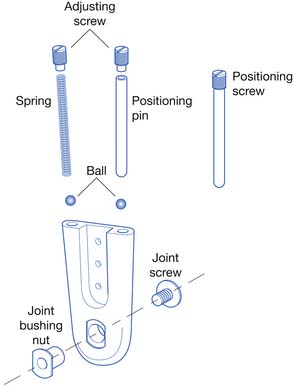
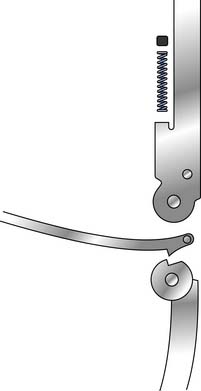
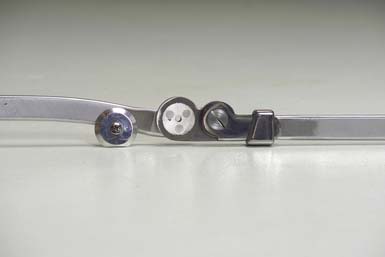
Ankle joint motion is controlled by pins or springs inserted into channels (Figures 15-7 through 15-10). The pins are adjusted with a screwdriver to set the desired amount of plantar flexion and dorsiflexion. The spring is also adjusted with a screwdriver to provide the proper amount of tension necessary to aid motion at the ankle joint (used to assist dorsiflexion). Longer channels help prevent the spring mechanism from ″bottoming out” and provide for more precise control of ankle motion.

FIGURE 15-8 Double-action stirrup (left) and dorsiflexion assist stirrup (right), used with the ankle joints shown in Figures 15-7 and 15-6, respectively.
(Courtesy USMC, Pasadena, CA.)
A solid stirrup is a U-shaped metal piece permanently attached to the shoe. Its two ends are bent upward to articulate with the medial and lateral ankle joints (see Figure 15-7). The proximal stirrup attachment sites are shaped to enforce the desired movements at the ankle joint (see Figure 15-8). The sole plate can be extended beyond the metatarsal head area for conditions requiring a longer lever arm for better control of plantar flexion (e.g., plantar spasticity).
A split stirrup can be used instead of a solid stirrup (see Figures 15-6 and 15-9). The split stirrup has a sole plate with two flat channels for insertion of the uprights. The two uprights are now called calipers, as they can open and close distally to allow donning and doffing of the AFO. A split stirrup allows removal of the uprights from the shoes so that the AFO can be worn with other shoes (see Figure 15-6). Other pairs of shoes should also have the sole plate with channels for calipers incorporated into the heel area. The split stirrup is not as stable as the solid stirrup, and the metal uprights can pop out, which is the main reason a split stirrup is infrequently used.
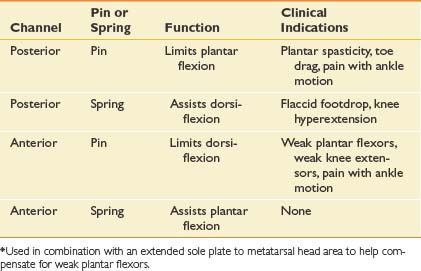
Ankle Stops and Assists
The ankle joint can be positioned so that it is in a neutral, dorsiflexed, or plantar-flexed position, depending on the gait disturbance. It can be set to permit a partial range of motion or to eliminate a certain motion. An understanding of the effect on the placement of pins and screws into the two channels of an ankle joint (see Figure 15-10) facilitates the proper orthotic prescription for the patient. This section reviews the common uses of the posterior stop (via pin), anterior stop (via pin), and the posterior dorsiflexion assist (via spring) of the orthotic metal ankle joint (Table 15-1). A spring in the anterior channel has not been demonstrated to be of clinical value.
Plantar Stop (Posterior Stop)
The plantar stop is used to control plantar spasticity or help incrementally stretch plantar contractures. The plantar stop is most commonly set at 90 degrees. A pin is inserted into the posterior channel of an ankle joint, such as that in Figure 15-10, to limit plantar flexion. An AFO with a plantar stop at 90 degrees produces a flexion moment at the knee during heel strike. Because the dorsiflexors cannot eccentrically activate to permit the foot to make contact with the ground, the ground reactive force remains posterior to the knee after heel strike, which creates a flexion moment at the knee (and possibly an unstable gait via buckling). The proximal portion of the AFO also has an effect on knee stability. The posterior portion of the proximal AFO exerts a forward push on the proximal leg to increase the knee flexion moment after heel strike (Figure 15-11). The opposite occurs at toe-off, with an extension moment created at the knee. This concept has been used to develop what has been referred to as a plastic ground reaction AFO, with a solid proximal anterior tibial closing that provides a greater influence on the knee. This device will be discussed in more detail later. The greater the plantar flexion resistance, the greater the flexion moment at the knee at heel strike, and the greater the need for active hip extensors to prevent the body from collapsing forward on a buckling knee.
The posterior stop should be set at the minimal amount of plantar flexion required to clear the foot during swing-through.18 Remember, plantar flexion creates a knee extension moment at the knee from midstance to toe-off. This provides a more stable knee during gait than when the ankle plantar stops are set in any degree of dorsiflexion.
A balanced decision should be made between providing resistance to plantar flexion to clear the foot during the swing phase of gait and the amount of instability at the knee during the stance phase of gait. No AFO is effective in reducing the amount of knee flexion to “normal” levels during the stance phase of gait.20
Dorsiflexion Stop (Anterior Stop)
An anterior stop is used to substitute for the function of the gastrocnemius-soleus complex (Figure 15-12). It is used in conditions with weak calf muscles or weak quadriceps (because of its effect on the knee). Weak calf musculature allows the ankle to enter dorsiflexion, and dorsiflexion creates a knee flexion moment after heel strike. The anterior stop set at 5 degrees of dorsiflexion best substitutes for gastrocnemius-soleus function.18,20 Three muscle groups help stabilize the knee during the gait cycle: the quadriceps, hamstrings, and gastrocnemius-soleus complex. All three of these muscle groups cross the knee joint and should be clinically evaluated and considered when prescribing a lower limb orthosis.
The earlier the dorsiflexion stop occurs during the stance phase, the greater the extension moment at the knee. This is useful in clinical situations where quadriceps weakness is also present. If the extension moment at the knee is too great for too long, genu recurvatum (“back knee”) can occur. A balance should be obtained such that the extension at the knee is sufficient to stabilize the knee in extension yet prevent genu recurvatum. If too much dorsiflexion is permitted by the anterior stop, there will be too much knee flexion during gait from midstance to toe-off.
Dorsiflexion Assist (Posterior Spring)
The posterior spring (see Figure 15-6) serves two purposes. It substitutes for concentric contraction of dorsiflexors to prevent flaccid foot drop after toe-off. It also substitutes (inadequately) for the eccentric activation of the dorsiflexors after heel strike.
A summary of some of the common indications for the various channel components is found in Table 15-1.
Metal Ankle-Foot Orthoses Varus-Valgus Control
Varus and valgus deformities are associated with rotation at the subtalar joint. A T strap is attached along the side of the shoe distal to the subtalar joint to help minimize the deformity (see Figure 15-6). T straps are also used to help prevent worsening of the deformity. T straps also help distribute pressure properly along the foot during weight-bearing.
T straps are referred to as being either medial or lateral. A lateral T strap is sewn to the lateral aspect of the shoe, and the belt is cinched around the medial upright of the AFO (see Figure 15-6). A lateral T strap is used to control a varus deformity. The belt is secured with a buckle around the medial upright. This helps create a force directing the subtalar joint outward, which counteracts the supination and adduction tendency that would result in excess varus. The opposite is true for a valgus deformity with the T strap being medially located. A pressure ulcer can develop over the malleolus if the T strap is buckled too tightly.
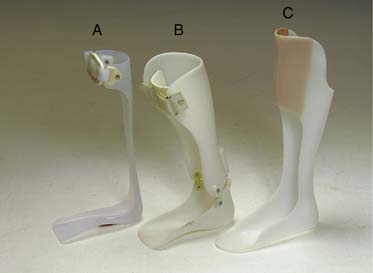
Plastic Ankle-Foot Orthoses
Plastic AFOs are the most commonly used AFOs because of their cost, cosmesis, light weight, interchangeability with shoes, ability to control varus and valgus deformities, provision of better foot support with the customized foot portion, and ability to achieve what is offered by the metal AFO (Figure 15-13). Energy consumption is equal with a plastic solid AFO or a metal double-upright AFO.3 Although a plastic orthosis weighs less than its metal counterpart, the weight of the orthosis is not as important as the influence of the ground reactive force created by the presence of the orthosis. The same orthotic principles apply to orthoses made of plastic or metal. The effect of the plastic AFO on knee stability should be recognized. The plastic AFO prescribed for toe clearance should be just rigid enough to provide resistance for toe clearance. Excessive resistance to plantar flexion can make the knee unstable (create a flexion moment) after heel strike.21
Some practical advice should be offered to the patient regarding the use of a plastic AFO. If changing shoes, it is best to have another pair with a similar heel height, to prevent altering the biomechanical effects at the foot, ankle, and knee. Tennis shoes are most accommodating for donning and doffing of the AFO. However, if dress shoes are to be worn, patients should also be told that their shoe size might need to be one-half size greater and the next width larger to accommodate the orthosis. A Blucher-style dress shoe with its open tongue helps accommodate the orthosis (see Figure 15-1).
Plastic Ankle-Foot Orthosis Components
Plastic AFOs can also be hinged at the ankle. Ankle hinges allow full or partial ankle motion, which can permit a more natural gait. They should be considered when complete restriction of ankle motion is not required. Plastic ankle joints are light and are a good choice for children. Metal ankle joints are preferred for adults, particularly heavy adults. Newer designs have a single midline posterior pin or spring mechanism (Figure 15-14). This midline spring functions like the more traditional medial and lateral dual posterior spring assist mechanism (see Figures 15-8 and 15-9). This makes the AFO narrower in the mediolateral direction and slightly longer in the anterior-posterior direction, which better conforms to the design of most pants. Hinging an AFO adds mediolateral stability. Consider prescribing a hinged AFO for a patient with spasticity with a tendency toward inversion, or for a patient with multiplanar ankle and subtalar flaccidity accompanying a foot drop with a history of twisting the ankle.
The leg component should encompass three quarters of the leg and should be padded along its internal surface.11 The proximal extent should end 1 inch below the fibular neck to prevent a compressive common peroneal nerve palsy.
The Solid Plastic Ankle-Foot Orthosis
The solid plastic AFO is the most commonly prescribed plastic AFO (see Figure 15-13). It can be made to serve several purposes. The term solid refers to an AFO that is made of a single piece of plastic. It does not have ankle joints. A solid AFO can still be flexible enough to allow some ankle motion, and it should be flexible with a posterior trim line for the treatment of foot drop without mediolateral instability. A solid AFO should be truly solid (not flexible) for the treatment of some cases of plantar spasticity.
Solid AFOs set at 90 degrees are commonly used for foot drop. Less obvious but equally important is the ability of the solid AFO to treat conditions affecting the knee. Again, it should be remembered that plantar flexion creates knee extension, and dorsiflexion creates knee flexion at heel strike. The AFO can be fixed in a few degrees of plantar flexion to provide stability at the knee during the stance phase of gait. Genu recurvatum can also be treated with a solid AFO. The more rigid the AFO, the greater the flexion moment at the knee at heel strike, which helps reverse the extension moment at the knee associated with genu recurvatum. The flexion moment at the knee also becomes even greater during midstance if the ankle is placed in a few degrees of dorsiflexion. Table 15-2 summarizes the important orthotic factors involved in creating knee extension and flexion moments throughout the gait cycle.
Table 15-2 Orthotic Componentry With Knee Flexion and Extension Moments
| Knee Extension Moment/Stability | Knee Flexion Moment/Instability |
|---|---|
| Cushioned heel | Solid heel |
| AFO fixed in plantar flexion | AFO fixed in dorsiflexion |
| Posterior trim line on AFO (flexible) | Anterior trim line on AFO |
| Posterior offset knee joint | — |
AFO, Ankle-foot orthosis.
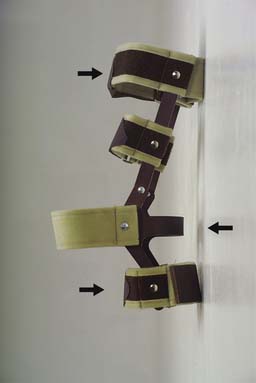
Plastic Ankle-Foot Orthosis Varus-Valgus Control
The goal of orthotic intervention is to alter the ground reactive forces with custom molding to help maintain proper alignment of the lower limb by “building up” selected portions of the AFO. A three-point system is used to provide the counter forces necessary to oppose the forces of the deformity (Figure 15-15).27,30 Some orthotists think that an orthosis should be firm (“not conforming”) to control a deformity. Pressure points should be present in expected areas at follow-up visits if the orthosis is serving its purpose. A custom ground reaction orthosis provides appropriate foot support that influences the rotation of more proximal joints (Figure 15-16). The anterior tibial shell closing helps stabilize the knee during gait (see Figure 15-11).

FIGURE 15-16 Oregon Orthotic System rotational control ankle-foot orthosis. Note the corrugations that add strength to the orthosis. Also note the metal ankle joint that is similar to those in Figure 15-10.
(Courtesy Oregon Orthotic System, Albany, OR.)
An equinovarus (or inversion) deformity is controlled by applying forces medially at the metatarsal head area and calcaneus. The next force is applied more proximally along the lateral aspect of the fibula. This helps prevent inversion at the subtalar and ankle joints. A more proximal medial tibial force is applied to provide stabilization of the leg portion of the plastic AFO by providing an opposing force to the fibular area (see Figure 15-15). A three-point system also exists at the foot level to help prevent supination of the foot related to the equinovarus deformity (see Figure 15-15). A three-point system is again applied to control the plantar flexion deformity associated with equinovarus (see Figure 15-15).
Patellar Tendon–Bearing Ankle-Foot Orthoses
A patellar tendon–bearing (PTB) AFO uses the patellar tendon and the tibial condyles to partially relieve weight-bearing stress on skeletal structures distally, with more weight-bearing distributed along the medial tibial condyle.25 PTB is a misnomer for this orthosis because only about 10% of the weight is distributed along the patellar tendon and the medial tibial condyle. Most of the weight-bearing is distributed throughout the soft tissues of the leg that are compressed by an appropriately fitted orthosis. Compression of the soft tissues of the leg is also responsible for maintaining alignment and length of the tibia after a fracture.45,46
PTB AFOs are often prescribed for diabetic ulcerations of the foot, tibial fractures, and relief of the weight-bearing surface in painful heel conditions such as calcaneal fractures, postoperative ankle fusions, and avascular necrosis of the foot or ankle. The orthoses are made of plastic and are bivalved. They fit snugly with the use of Velcro straps (Figure 15-17) or buckles similar to those of ski boots. A custom-molded PTB AFO can reduce weight-bearing in the affected foot by up to 50%.
Pressure Relief Ankle-Foot Orthoses
A pressure relief AFO is also known by its acronym, PRAFO (Figure 15-18). This type of AFO has different brand names depending on the company that furnished it, including PRAFO, Multi-podus AFO, and Lennard AFO. This orthosis serves two purposes: pressure relief and contracture prevention. Pressure relief is achieved at the heel by completely eliminating weight-bearing with the heel cut out, and also by using a hinged lever arm posteriorly that can be adjusted medially or laterally to prevent medial or lateral malleolar pressure sore development. This should be applied on the immobilized or motionless affected lower limb at all times while in bed. A PRAFO is frequently used in demented patients with hip fractures who do not have much lower limb mobility, as well as in patients with a stroke who have dense hemiplegia. Plantar flexion contracture prevention occurs by keeping the ankle joint in a neutral position while the AFO is donned.
Common Ankle-Foot Orthosis Prescriptions
The three most common physiatric AFO prescriptions are those for foot drop, plantar spasticity, and lumbar spinal cord injury (Figure 15-19). The most common AFO prescription for foot drop is a custom nonhinged plastic AFO set in a few degrees of dorsiflexion with a posterior trim line. This is also referred to as a posterior leaf spring AFO. The few degrees of dorsiflexion ensures foot clearance during the swing phase of gait. It also helps the ankle “spring” into dorsiflexion after the foot is lifted off the ground in a plantar-flexed position from push-off. The minimal weight and bulk of this AFO are highly desired by the patient with foot drop. The avoidance of hinging not only minimizes bulk, but from a practical standpoint it keeps the mediolateral dimension of the AFO narrow to best accommodate a variety of shoes and pants. If there is significant subtalar joint instability (e.g., a patient with a history of inversion injuries and falling), a hinged plastic AFO with metal double-action ankle joints (see Figure 15-10) with springs in the posterior channels (dorsi-assist) would provide mediolateral stability yet also permit plantar flexion. Alternatively, a hinged midline posterior stop AFO that is spring-loaded (see Figure 15-14) can also provide mediolateral stability for the patient with foot drop.
The most common AFO prescription for plantar spasticity is either a hinged custom plastic AFO with a single midline posterior stop or a hinged custom plastic AFO with pins in the posterior channels to provide plantar stop at 90 degrees. The former is more likely to be considered in milder cases of spasticity without a significant inversion deformity. The latter is more likely to be considered if a significant inversion deformity is still present after all other medical treatment measures to manage the spasticity have been exhausted. Metal ankle joints with posterior pins in this case would provide better mediolateral support yet still permit some dorsiflexion with the anterior channels left open. Permitting dorsiflexion allows a more normalized gait and provides a therapeutic stretch to the plantar flexors from midstance to toe-off during gait. Recent research studies support the use of hinged AFOs with plantar stops at neutral (90 degrees) as a preferred AFO for an active pediatric population with lower limb spasticity.37,40,49,53,54
Knee-Ankle-Foot Orthoses
The use of KAFOs often complements the use of a wheelchair for ambulation. The proprioceptive level is a reliable indicator of which spinal cord–injured patients can achieve ambulation status.57 It is helpful to have sensation and proprioception in the lower limbs to ambulate safely with KAFOs. The level of the spinal cord injury is also important in predicting the ability to ambulate. Adult spinal cord–injured patients with lesions at or above T12 generally are not functional ambulators because of the metabolic cost involved.33 Children have a higher center of gravity and can have a functional gait with a higher spinal cord lesion. Muscle function is a predictor of the quality of ambulation. Good trunk control and upper body strength are needed to ambulate with KAFOs because these devices are used in combination with ambulation aids, such as walkers and Lofstrand forearm orthoses.
Some patients with paraplegia, such as those with lower lumbar lesions with some knee extensor strength, are able to ambulate without KAFOs. Ambulation in these patients can often be accomplished with the use of bilateral plastic ground reaction AFOs (see Figures 15-11 and 15-16) with the ankles fixed in 10 to 15 degrees of plantar flexion. The plantar flexion provides an extension moment at the knee during gait for stability with ambulation. The proximal anterior tibial shell closing provides further stability at the knee from midstance to toe-off (see Figure 15-11, part 4). A walker or two Lofstrand forearm orthoses can be used for additional support and balance.
Knee Joints
There are three basic types of knee joints. The straight-set knee joint provides rotation about a single axis (Figure 15-20). It allows free flexion but prevents hyperextension. It is often used in combination with a drop lock, which keeps the knee in extension throughout all phases of gait for further stability.
The polycentric knee joint uses a double-axis system to simulate the flexion-extension movements of the femur and tibia at the knee joint (Figure 15-21). Although this concept is theoretically sound, the polycentric knee joint has not proved to be advantageous over the straight-set knee joint, and it is less commonly used. It also adds bulk to the orthosis. It is most frequently used in sport knee orthoses.
The third type of knee joint is the posterior offset knee joint (Figures 15-22 and 15-23; see Table 15-2). It is prescribed for patients with weak knee extensors and some hip extensor strength. It allows free flexion and extension of the knee during the swing phase of gait and helps keep the orthotic ground reactive force in front of the knee axis for stability during stance. The center of gravity is normally posterior to the knee at heel strike, creating a flexion moment at the knee, which requires quadriceps and hamstring muscle contraction to counteract this force. The posterior offset knee joint component of the KAFO helps place the ground reactive force anterior to the orthotic knee joint, creating an extension moment at the knee during stance to compensate for the weak knee extensors. The posterior offset knee joint should have a hyperextension stop to help prevent genu recurvatum.
Occasionally the offset knee joint does not provide adequate stability at the knee. The ankle component of the KAFO can then be set in 10 to 15 degrees of plantar flexion to further help create an extension moment at the knee for stability. Lastly, if these measures are insufficient at providing knee stability, the posterior offset knee joints can be locked in extension with drop locks (see Figure 15-20).
Knee Locks
The ratchet lock has recently become the most commonly prescribed knee lock (Figure 15-24). The ratchet lock has a catching mechanism that operates in 12-degree increments. As the user rises from a seated to a standing position, if there is a tendency for the knee to become unstable and flex, the ratchet lock prevents that movement and keeps the gains made toward extension. Once the patient is standing with the knees extended, knee flexion is achieved by pressing down on either a release lever or by sliding the locking mechanism.
Before the development of the ratchet lock, the drop lock (ring lock) was used most commonly in both the medial and lateral uprights of the KAFO (see Figure 15-20). Its advantage is simplicity of design without bulk. However, fine motor coordination skills are needed to lock the knee in complete extension. In addition, there are two locks per side yet only two hands. The drop lock also can “settle” after ambulation and might be difficult to pull up to unlock the knee. The disadvantage of the drop lock in comparison with the ratchet lock is that there is no locking mechanism until full knee extension is obtained. Consequently a patient’s knee can collapse into flexion when it is not sufficiently extended to activate the drop lock. A collapse into flexion does not occur with the ratchet lock, and so the patient is less likely to fall. A drop lock can be used unilaterally along the lateral upright if the patient is relatively lightweight and has a low activity level.
The bail lock (also known as the Swiss, French, Schweitzer, or pawl lock) provides the easiest method of simultaneously unlocking the medial and lateral knee joints of a KAFO (Figures 15-25 and 15-26). Two hands can be used for two bail locks, whereas there are a total of four ratchet locks or four drop locks with other bilateral KAFOs. Lifting up the bail posteriorly releases the knee joint to permit flexion, allowing the patient to sit down. The patient can also alternatively catch the bail on the edge of a chair by leaning back to release the lock mechanism to permit sitting. The locking mechanism is spring-loaded to assist locking the knee into extension (see Figure 15-26). The bail is often padded with rubber to protect the clothing from being torn or soiled. The KAFO with a bail lock can be worn over or under clothes, depending on the size of the bail lock and the size of the clothing. On its downside, child cruelty can lead to one child kneeing the handicapped child’s knee from behind and, with this type of lock, causing the child to fall—not a good practical joke.
The dial lock (formerly known as a turn buckle) is used to stabilize the knee in varying amounts of flexion (Figure 15-27). It can be adjusted in 6-degree increments and is more precise for the management of a knee with a flexion contracture than a KAFO with ratchet locks. Its uses include helping prevent progression of a flexion contracture or assisting with the gradual reduction of a flexion contracture.
Scott-Craig Orthosis
The Scott-Craig orthosis (Figure 15-28) was designed to provide the patient with paraplegia who has a complete lesion at L1 or higher, with a more functional and comfortable gait.47 It was also designed to reduce unnecessary hardware, to be a KAFO of lighter weight, and to be easy to don and doff. This orthosis was named after an orthotist, Bruce Scott, who worked at Craig Hospital in Englewood, Colorado.
The orthotic design consists of an ankle joint with anterior (permits 5 degrees of dorsiflexion to simulate plantar flexion) and posterior (set at 90 degrees to prevent toe drag) pin stops, a sole plate extending to the metatarsal heads, a crossbar added to the metatarsal head area for mediolateral stabilization, and an offset knee joint with a bail lock.47 A rigid anterior tibial band is positioned directly below the tibial tubercle. A rigid proximal thigh band is positioned posteriorly and is closed anteriorly with a soft strap secured with Velcro. These two bands should be shallow enough to hold the knee in extension. A three-point system helps keep the knee in extension by applying pressure at the proximal thigh posteriorly, the proximal tibia anteriorly, and at the calcaneus posteriorly.22 The ankle joint functions with a dorsiflexion stop used to simulate the triceps surae function as previously described, and with a posterior stop set at 90 degrees to prevent toe drag.
A group headed by Lehmann24 analyzed the Scott-Craig orthosis and found that it was the easiest of the KAFOs tested to don and doff. The original design of this orthosis is still being prescribed for patients with paraplegia.
Knee Orthoses
Swedish Knee Cage
The knee orthosis (KO) known as a Swedish knee cage (Figure 15-29) is used to control minor to moderate genu recurvatum caused by ligamentous or capsular laxity. This articulated KO permits full knee flexion and prevents hyperextension. The Swedish knee cage uses a classic three-point orthotic system with two bands placed anterior to the knee axis (one above and one below the knee) and a third band posterior to the knee joint in the popliteal area. It also has an additional thigh band with longer uprights to obtain better leverage at the knee joint. Severe genu recurvatum might need to be controlled with longer lever arms, such as that offered by a KAFO.
Osteoarthritis Knee Orthoses
The same orthotic three-point principle that has been applied for years in the Swedish knee cage for genu recurvatum has recently also been applied to osteoarthritis of the knee, most commonly with medial compartment narrowing (Figure 15-30). The three-point system distribution is achieved by a strap that is applied across the knee joint. In one study, 19 of 20 patients with varying degrees of osteoarthritis experienced significant relief of knee pain.27 Radiographic improvement in joint alignment was also noted. The limiting factor regarding this knee orthotic prescription is the patient’s weight. A morbidly obese patient with an abundance of fatty tissue around the knee will not support the KO adequately. In such cases where this KO and surgery are precluded, the foot orthoses with lateral buildup as described earlier in this chapter should be considered. The foot orthosis with a lateral buildup is considered the preferred first-line orthotic treatment for osteoarthritis of the knee. (See Osteoarthritis of the Knee in the Foot Orthoses section.)

FIGURE 15-30 The Generation II knee orthosis for tricompartmental osteoarthritis of the knee. This uses the standard orthotic three-point distribution system in a medial-lateral distribution rather than in an anterior-posterior distribution as was noted with the Swedish knee cage (see Figure 15-29).
Sport Knee Orthoses
There is an increasing abundance of sport orthoses on the market. There is also a lack of definitive research regarding their role in sports. This can lead to much confusion regarding their prescription, unless the KO is reviewed systematically. Sport KOs can be divided into prophylactic, rehabilitative, and functional categories.31
Prophylactic knee bracing attempts to prevent or reduce the severity of knee injuries. There is currently no evidence to support the use or cost benefit of these orthoses. Some studies have found that the use of these orthoses actually increased the number of athletes with knee injuries.44,52 It is theorized that knee-braced players can put themselves in compromising positions because of overreliance on the orthosis and that this can contribute directly to the increasing injury rates observed. The use of prophylactic knee bracing has also been associated with increased energy consumption, which can impair athletic performance.13
Rehabilitative knee bracing is used to allow protected motion within defined limits.36 It is useful for postoperative and conservative management of knee injuries, and is most commonly applied postoperatively for anterior cruciate ligament–reconstructed knees (Figure 15-31) and patellofemoral pain syndrome.∗
Functional knee bracing is designed to assist or provide stability for the unstable knee. Functional knee bracing does not replace the need for rehabilitation of the knee. Knee braces are used most commonly to stabilize a laterally subluxing patella7,28 or an anterior cruciate ligament–deficient knee.2,32,51 Their use has been shown to be effective only at loads much lower than those placed on the knee during athletic participation. In summary, functional knee bracing can possibly play a role in the treatment of pathologic laxity by possibly decreasing the frequency of unstable episodes.36
Pediatric Orthoses
Caster Cart
The disabled child should identify early with motion so that ambulatory skills can progress naturally.1 Without familiarity with motion, disabled children lack the desire to ambulate once placed in a parapodium or reciprocating gait orthosis.
The caster cart (Figure 15-32) is used for children with a developmental delay in ambulatory skills, and it serves as an initial mobility aid. It is most often prescribed for children with spina bifida. Most children are upright and cruising by 10 months.14 Children with paraplegia should be fitted for a caster cart once they have obtained enough upper limb strength and trunk balance to propel themselves. If balance is a problem for the child, a deep seat bucket can be prescribed to help provide balance so that the child can use the upper limbs for propulsion.
Standing Frame
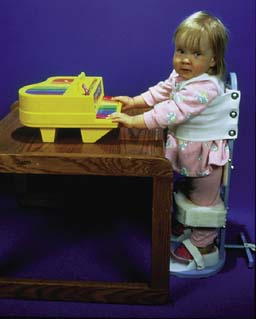
The use of a standing frame (Figure 15-33) typically follows successful use of a caster cart. The age range for initial use is usually 8 to 15 months. Children can continue to use their caster carts during this time. Children who are pulling themselves up along furniture are typically ready for a standing frame. This is the first sign that they are interested in standing and moving.14
Parapodium
The parapodium was also referred to in the past as a swivel orthosis (Figure 15-34). Before children are given a parapodium, they should first demonstrate adequate use of a standing frame and exhibit a desire to ambulate. A child’s standing frame can be evaluated for wear and tear to determine whether it has been used sufficiently so that the child can advance to a parapodium. A frequently used standing frame (or any orthosis) will show evidence of wear and tear that includes soiling and scratches. It is important to note this, because parents frequently set expectations too high for the disabled child. A child who has not used a standing frame will likely be unable or unwilling to ambulate with a parapodium.
A parapodium is an appropriate prescription for children who are unlikely to become functional walkers because of the severity of their impairment. It often complements wheelchair use.26 It is most commonly prescribed for children between 2.5 to 5 years of age.
A parapodium allows crutchless gait. Ambulation occurs by the child pivoting the hips and using “body English” to swivel one side of the oval-based stand forward and then repeating the same event for the other side. Its design is similar to the standing frame, but it has hip and knee joints. The hip and knee joints remain locked in extension to permit ambulation in the upright position but can be unlocked (simultaneously in some models) to permit sitting. The difficulties experienced with the use of this orthosis include donning and doffing and rising from a seated position to a standing position.
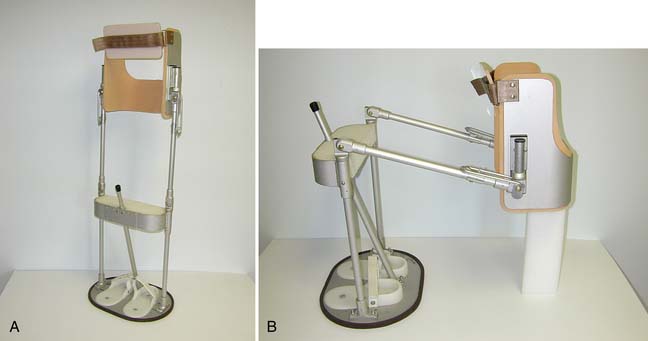
Reciprocating Gait Orthosis
The reciprocating gait orthosis (RGO) was formerly known as a hip-guided orthosis (Figure 15-35). It can also be referred to as a bilateral hip-knee-ankle-foot orthosis (HKAFO). The purpose of the RGO is to provide contralateral hip extension with ipsilateral hip flexion. The RGO is appropriate for children who have used the standing frame, developed good trunk control and coordination, can safely stand, and are mentally prepared for ambulation. Good upper limb strength, trunk balance, and active hip flexion are important positive variables for ambulation.12 Obesity, advanced age, lack of patient or family motivation, scoliosis, spasticity,8 and contractures are significant negative factors in the long-term use of the RGO. This type of orthosis clearly only complements the use of a wheelchair for mobility purposes and serves therapeutic purposes of exercise and upright activities. One newer type of spinal cord injury orthosis is the Walkabout which has a scissoring mechanism in the groin area attaching two KAFOs via a hinge. The trade-off with this device is a lack of contralateral hip extension with ipsilateral hip flexion for a less bulky orthosis to don and doff.34

FIGURE 15-35 Isocentric reciprocating gait orthosis.
(Courtesy Center for Orthotic Design, Redwood City, Calif, and Fillauer Companies, Inc, Chattanooga, TN.)
The RGO is prescribed most commonly for children aged 3 to 6 years. The concept of the RGO was developed by researchers working with a patient who had active hip flexion and no hip extension. Gait is initiated with unilateral hip flexion and can be assisted by swaying the trunk when hip flexion is inadequate. This type of gait pattern can also be considered to be a form of physical therapy, because hip extension occurs passively with each step, helping to reduce flexion contractures. Cables were initially used to provide the necessary hip motion, but newer mechanical methods of reciprocal gait use a “teeter-totter” concept (see Figure 15-35). This type of RGO has been reported to be more energy efficient than an RGO with cables.60
Crutches are used with the RGO to provide a control mechanism, taking advantage of the forward momentum to produce small propulsive forces when needed.29 This also is a disadvantage of this orthosis (compared with the parapodium) because the upper limbs are not free for other activities. The patient with an RGO is able to negotiate a greater variety of surfaces than would be possible with the parapodium.43
Ambulation Aids
The purpose of using ambulation aids (Figures 15-36 and 15-37) is to increase the area of support for patients who have difficulty maintaining their center of gravity safely over their own support area. A variety of aids are available for the individual needs of patients. Ambulation aids improve balance, redistribute and extend the weight-bearing area, reduce lower limb pain, provide small propulsive forces, and provide sensory feedback. They should be considered an extension of the upper limb. Their proper use requires adequate upper limb strength and coordination. An exercise program for the upper limbs is useful and can complement ambulation with the aid by increasing endurance and stability. A supervised period of training is recommended after prescription of an aid.

FIGURE 15-36 Ambulation aids. (Left to right) C cane, Lofstrand forearm orthosis, walker, crutch, and quad cane.

FIGURE 15-37 Wooden forearm orthosis (Kenny stick). The leather band encloses the proximal forearm.
(Courtesy Thomas Fetterman, Inc, Southampton, PA.)
The type of aid needed depends on how much balance and weight-bearing assistance is needed. The body weight transmission for a unilateral cane opposite the affected side is 20% to 25%.4 It is 40% to 50% with the use of a forearm or arm cane.4 Body weight transmission with bilateral crutches is estimated at up to 80%.5
Canes
There are three common types of canes (see Figure 15-36). The C cane is most commonly used. It is also known as a crook top cane or a J cane. A functional grip cane offers the patient a grip that can be more comfortable than with the C cane. A quad cane provides an increased area of support compared with the other canes. Quad canes also come in narrow- and wide-based forms for different degrees of support. The lateral two legs are directed away from the body.
A cane is used on the side opposite the supporting lower limb. It is advanced with the opposite lower limb. It is usually held on the patient’s unaffected side. This can be done to lessen the force exerted on a hip with pathology. The load is increased by four times the body weight on the stance side during gait because of the gravitational forces and the gluteus medius–gluteus minimus force exerted across the weight-bearing hip.5 The cane helps decrease the force generated across the affected hip joint by decreasing the work of the gluteus medius-minimus complex. This occurs when the upper limb exerts force on the cane to help minimize pelvic drop on the side opposite the weight-bearing lower limb.
Walker
Crutches
Nonaxillary Crutches
Nonaxillary crutches are more appropriately called forearm or arm canes, or forearm or arm orthoses. The Loftstrand forearm orthosis, Kenny sticks, the Everett or Warm Spring orthosis, the Canadian crutch, and the platform forearm orthosis will be discussed (see Figures 15-36 and 15-37).
Forearm Orthoses
Lofstrand Forearm Orthosis
Wooden Forearm Orthosis (Kenny Stick)
Another forearm orthosis option is the Kenny stick (see Figure 15-37). It was named after Sister Kenny, who sawed off the top half of wooden crutches and placed a leather band around the proximal portion of the forearm. It was designed for polio patients who had satisfactory proximal upper limb musculature but were weak distally and unable to effectively hold and control the orthosis. Its advantage over the Loftstrand orthosis is the presence of a closed leather band. This assures patients (more so than the Lofstrand forearm orthosis does) that they will not drop the ambulation aid.
Platform Forearm Orthosis
Crutch Tips and Hand Grips
The purpose of crutch tips is to absorb shock and prevent slippage. Crutches are only as safe as the quality of their crutch tips. Special crutch tips are available for rainy and icy conditions (Figure 15-38). At each checkup the physician should make sure that the crutch tips are not worn out. Hand grips are used to reduce pressure on the hands and are also safety features because they help prevent slippage.
Prescription
A medical diagnosis with delineation of the impairment and any resulting disability should be made before an orthotic prescription is written. The orthotic goals should be documented for the orthotist. An AFO prescription should include the type of ankle (rigid, flexible, or jointed) and the position of the ankle (neutral, dorsiflexed, or plantar flexed). If the ankle is jointed, the range of motion should be specified. In the case of a compressive peroneal nerve palsy, for example, the physical impairment would be a flaccid foot drop. The ankle should be flexible and held in a neutral position with a plastic AFO set in a few degrees of dorsiflexion. The goals include toe clearance during swing-through and prevention of foot slap during early stance.19
From an orthotic prescription standpoint, most of this chapter is concisely summarized in Figure 15-39, a full-size prescription pad with convenient check boxes and room at the top of the page to copy this onto a letterhead for clinical use. Adjacent to this sheet is a quick summary reference that can be copied onto the back of the prescription sheets (Box 15-2).
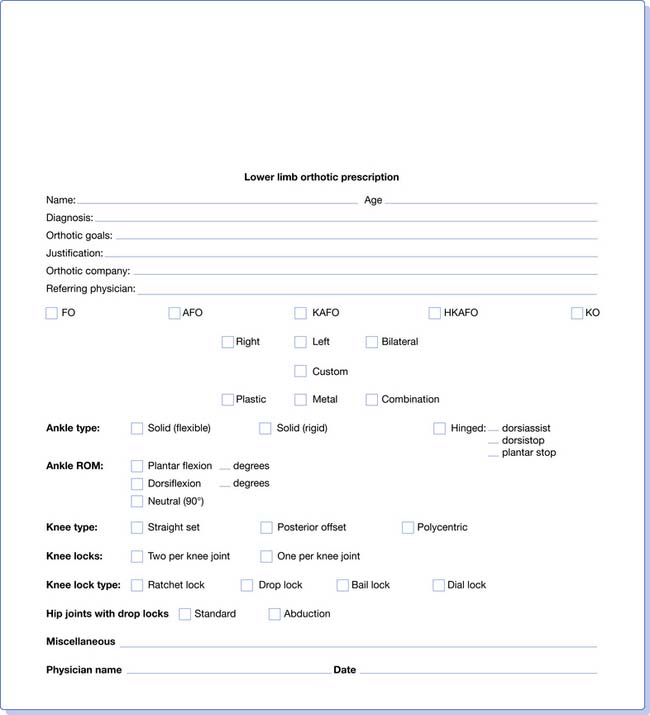
FIGURE 15-39 Lower limb orthotic prescription sheet. (For a printable version of this form, see the Expert Consult website.)
BOX 15-2 Summary Reference for Prescription Pad
Foot Orthosis
Ankle-Foot Orthosis
Hinge Indications
1. Bleck E.E. Developmental orthopaedics. III. Toddlers. Dev Med Child Neurol. 1982;24:533-555.
2. Chew K.Y., Lew H.L., Date E., et al. Current evidence and clinical applications of therapeutic knee braces. Am J Phys Med Rehabil. 2007;86(8):678-686.
3. Corcoran P.J., Jebsen R.H., Brengelmann G.L., et al. Effects of plastic and metal leg braces on speed and energy cost of hemiparetic ambulation. Arch Phys Med Rehabil. 1970;51:69-77.
4. D’Ambrosia R.D. Conservative management of metatarsal and heel pain in the adult foot. Orthopedics. 1987;10:137-142.
5. Deathe A.B., Hayes K.C., Winter D.A. The biomechanics of canes, crutches, and walkers. Crit Rev Phys Rehab Med. 1993;5:15-29.
6. Diveley RL: Foot appliances and alterations. In: American Academy of Orthopaedic Surgeons, eds. Orthopaedic appliances atlas, vol. 1, Ann Arbor, 1952, JW Edwards.
7. Draper C.E., Bsier T.F., Santos J.M., et al. Using real-time MRI to quantify altered joint kinematics in subjects with patellofemoral pain and to evaluate the effects of a patellar brace or sleeve on joint motion. J Orthop Res. 2009;27(5):571-577.
8. Gok H., Kucukdeveci A., Yavuzer G., et al. Effects of ankle-foot orthoses on hemiparetic gait. Clin Rehabil. 2003;17:137-139.
9. Gross M.T., Foxworth J.L. The role of foot orthoses as an intervention for patellofemoral pain. J Orthop Sports Phys Ther. 2003;33:661-670.
10. Guidera K.J., Smith S., Raney E., et al. Use of the reciprocating gait orthosis in myelodysplasia. J Pediatr Orthop. 1993;13:341-348.
11. Halar E., Cardenas D. Ankle-foot orthoses: clinical implications. Phys Med Rehabil State Art Rev. 1987;1:45-66.
12. Harvey L.A., Smith M.B., Davis G.M., et al. Functional outcomes attained by T9-12 paraplegic patients with the Walkabout and the Isocentric reciprocal gait orthoses. Arch Phys Med Rehabil. 1997;78:706-711.
13. Houston M.E., Goemans P.H. Leg muscle performance of athletes with and without knee support braces. Arch Phys Med Rehabil. 1982;63:431-432.
14. Johnson E.W., Spiegel M.H. Ambulation problems in very young children. JAMA. 1961;175:858-863.
15. Keating E.M., Faris P.M., Ritter M.A., et al. Use of lateral heel and sole wedges in the treatment of medial osteoarthritis of the knee. Orthop Rev. 1993;22:921-924.
16. Lee S.Y., McKeon P., Hertel J. Does the use of orthoses improve self-reported pain and function measures in patients with plantar fasciitis? A meta-analysis. Phys Ther Sport. 2009;10(1):8-12.
17. Lehmann J.F. The biomechanics of ankle foot orthoses: prescription and design. Arch Phys Med Rehabil. 1979;60:200-207.
18. Lehmann J.F., Condon S.M., de Lateur B.J., et al. Ankle-foot orthoses: effect on gait abnormalities in tibial nerve paralysis. Arch Phys Med Rehabil. 1985;66:212-218.
19. Lehmann J.F., Condon S.M., de Lateur B.J., et al. Gait abnormalities in peroneal nerve paralysis and their correlation by orthoses: a biomechanical study. Arch Phys Med Rehabil. 1986;67:380-386.
20. Lehmann J.F., de Lateur B.J., Warren C.G., et al. Biomechanical evaluation of braces for paraplegics. Arch Phys Med Rehabil. 1969;50:179-188.
21. Lehmann J.F., Esselman P., Ko M.J., et al. Plastic ankle foot orthoses: evaluation of function. Arch Phys Med Rehabil. 1983;64:402-407.
22. Lehmann J.F., Warren C.G. Restraining forces in various designs of knee ankle orthoses: their placement and effect on anatomical knee joint. Arch Phys Med Rehabil. 1976;57:430-437.
23. Lehmann J.F., Warren C.G., de Lateur B.J. A biomechanical evaluation of knee stability in below knee braces. Arch Phys Med Rehabil. 1970;51:687-695.
24. Lehmann J.F., Warren C.G., Hertling D., et al. Craig Scott orthosis: a biomechanical and functional evaluation. Arch Phys Med Rehabil. 1976;57:438-442.
25. Lehmann J.F., Warren C.G., Pemberton D.R., et al. Load bearing function of patellar tendon bearing braces of various designs. Arch Phys Med Rehabil. 1971;52:367-370.
26. Liptak G.S., Shurtleff D.B., Bloss J.W., et al. Mobility aids for children with high-level myelomeningocele: parapodium versus wheelchair. Dev Med Child Neurol. 1992;34:787-796.
27. Loke M. New concepts in lower limb orthotics. Phys Med Rehabil Clin N Am. 2000;11:477-496.
28. Lun V.M., Wiley J.P., Meeuwisse W.H., et al. Effectiveness of patellar bracing for treatment of patellofemoral pain syndrome. Clin J Sport Med. 2005;15(4):235-240.
29. Major R.E., Stallard J., Rose G.K. The dynamics of walking using the hip guidance orthosis (HGO) with crutches. Prosthet Orthot Int. 1981;5:19-22.
30. Marx H.W. Lower limb orthotic designs for the spastic hemiplegic patient. Orthot Prosthet. 1974;28:14-20.
31. Matsuno H., Kadowaki. Tsjui H: Generation II knee bracing for severe medial compartment osteoarthritis of the knee. Arch Phys Med Rehabil. 1997;78:745-749.
32. McDevitt E.R., Taylor D.C., Miller M.D., et al. Functional bracing after anterior cruciate ligament reconstruction: a prospective, randomized, multicenter study. J Bone Joint Surg Am. 2004;32(8):1887-1892.
33. Merritt J.L. Knee-ankle-foot orthotics: long leg braces and their practical applications. Phys Med Rehabil State Art Rev. 1987;1:67-82.
34. Middleton J.W., Yeo J.D., Blanch L., et al. Clinical evaluation of a new orthosis, the ‘Walkabout’, for restoration of functional standing and short distance mobility in spinal paralysed individuals. Spinal Cord. 1997;35:574-579.
35. Milgram J.E., Jacobson M.A. Footgear: therapeutic modifications of sole and heel. Orthop Rev. 1978;7:57-61.
36. Millet C., Drez D.Jr. Knee braces. Orthopedics. 1987;10:1777-1780.
37. Radtka S.A., Skinner S.R., Dixon D.M., et al. A comparison of gait with solid, dynamic and no ankle-foot orthoses in children with spastic cerebral palsy. Phys Ther. 1997;77:395-409.
38. Redford J.B. Orthoses. In: Basmajian J.V., Kirby R.L., editors. Medical rehabilitation. Baltimore: Williams & Wilkins, 1984.
39. Reid D.C. Heel pain and problems of the hindfoot. In: Reid D.C., editor. Sports injury assessment and rehabilitation. New York: Churchill Livingstone, 1992.
40. Rethlefsen S., Kay R., Dennis S., et al. The effects of fixed and articulated ankle-foot orthoses on gait patterns in subjects with cerebral palsy. J Pediatr Orthop. 1999;19:470-474.
41. Riegler H.F. Orthotic devices for the foot. Orthop Rev. 1987;16:293-303.
42. Roos E., Engstrom M., Soderberg B. Foot orthoses for the treatment of plantar fasciitis. Foot Ankle Int. 2006;27(8):606-611.
43. Rose G.K., Stallard J., Sankarankutty M. Clinical evaluation of spina bifida patients using hip guidance orthoses. Dev Med Child Neurol. 1981;23:30-40.
44. Rovere G.D., Haupt H.A., Yates C.S. Prophylactic knee bracing in college football. Am J Sports Med. 1987;15:111-116.
45. Sarmiento A. A functional below the knee brace for tibial fractures: a report of its use in 135 cases. J Bone Joint Surg Am. 1970;52:295-311.
46. Sarmiento A., Gersten L.M., Sobol J.A., et al. Tibial shaft fractures treated with functional braces: experience with 780 fractures. J Bone Joint Surg Br. 1989;71:602-609.
47. Scott B.A. Engineering principles and fabrication techniques for Scott-Craig: long leg brace for paraplegics. Orthot Prosthet. 1974;28:14-19.
48. Shrader J.A., Siegel K.L. Nonoperative management of functional hallux limitus in a patient with rheumatoid arthritis. Phys Ther. 2003;83:831-843.
49. Smiley S.J., Jacobsen F.S., Mielke C., et al. A comparison of the effects of solid, articulated, and posterior leaf-spring ankle-foot orthoses and shoes alone on gait and energy expenditure in children with spastic diplegic cerebral palsy. Orthopedics. 2002;25:411-415.
50. Staheli L.T., Chew D.E., Corbett M. The longitudinal arch. J Bone Joint Surg Am. 1987;69:426-428.
51. Sterett W.I., Briggs K.K., Farley T., et al. Effect of functional bracing on knee injury in skiers with anterior cruciate ligament reconstruction: a prospective cohort study. Am J Sports Med. 2006;34(10):1581-1585.
52. Teitz C.C., Hermanson B., Kronmal R.A., et al. Evaluation of the use of braces to prevent injury to the knee in collegiate football players. J Bone Joint Surg Am. 1987;69:2-9.
53. Thomas S.S., Buckon C.E., Jakobson-Huston S.J., et al. Comparison of three ankle-foot orthosis configurations for children with spastic hemiplegia. Dev Med Child Neurol. 2001;43:371-378.
54. Thomas S.S., Buckon C.E., Jakobson-Huston S.J., et al. Stair locomotion in children with spastic hemiplegia: the impact of three different ankle foot orthosis (AFOs) configurations. Gait Posture. 2002;16:180-187.
55. Crutches Varghese G., canes, walkers. In: Redford J.B., editor. Orthotics etcetera, ed 3, Baltimore: Williams & Wilkins, 1980.
56. Von Werssowetz O.F. Basic principles of lower extremity bracing. Orthot Prosthet Appl J, pp. 1962:325-350.
57. Waters R.L., Miller L. A physiologic rationale for orthotic prescription in paraplegia. Clin Prosthet Orthot. 1987;11:66-73.
58. Wenger D.R., Mauldin D., Morgan D., et al. Foot growth rate in children age one to six years. Foot Ankle. 1983;3:207-210.
59. Wenger D.R., Mauldin D., Speck G., et al. Corrective shoes and inserts as treatment for flexible flatfoot in infants and children. J Bone Joint Surg Am. 1989;71:800-810.
60. Winchester P.K., Carollo J.J., Parekh R.N., et al. A comparison of paraplegic gait performance using two types of reciprocating gait orthoses. Prosthet Orthot Int. 1993;17:101-106.
61. Woodburn J., Barker S., Helliwell P.S. A randomized control trial of foot orthoses in rheumatoid arthritis. J Rheumatol. 2002;29:1377-1383.
62. Wright R.W., Fetzer G.B. Bracing after ACL reconstruction: a systematic review. Clin Orthop Relat Res. 2007;455:162-168.
63. Zamosky I., Redford J.B. Shoes and their modifications. In Redford J.B., editor: Orthotics etcetera, ed 3, Baltimore: Williams & Wilkins, 1980.