CHAPTER 65 LOWER EXTREMITY VASCULAR INJURIES: FEMORAL, POPLITEAL, AND SHANK VESSEL INJURY
Lower extremity vascular injuries can be devastating and life threatening. The morbidity and mortality associated with these injuries are dependent on a multitude of factors, including the extent of injury, overall condition of the patient, and duration of ischemia. Deciding whether limb salvage is the optimal management for the injured patient requires good judgment. The initial decision to salvage the injured extremity depends on the ability of the patient to tolerate the procedure required to successfully repair the injury. It also depends on the likelihood of limb salvage as well as a satisfactory functional limb outcome. In the past, ligation of vascular injuries was often the approach taken to “save a life,” and was favored because of a high amputation rate (up to 40%) reported when a surgical approach to repair the injuries was used.1 Currently, the amputation rate in civilian trauma undergoing vascular repair is below 10% and this is not the preferred approach to manage extremity vascular injury. This reduction in the amputation rate over the past few decades has been attributed to a multitude of factors, including rapid transport time, improved prehospital care, soft tissue coverage, decreasing warm ischemia time (using the damage control approach and vascular shunt), low-velocity weapons, antibiotic utilization, and the early and aggressive use of fasciotomy.
INCIDENCE AND MECHANISM OF INJURY
Lower extremity vascular injuries occur most frequently in young men. In both the urban and rural setting, penetrating injuries to the extremity are the most common cause of peripheral vascular trauma. Penetrating injuries occur more commonly in the urban setting because of high levels of interpersonal violence and mostly result from gunshot wounds or stab wounds.1 Blunt injuries occur more commonly in the rural setting because of a higher incidence of farming and industrial-type injuries. In part caused by a rise in urban violence and high-speed motor vehicles, the incidence of peripheral vascular trauma is increasing. Compared with other arterial injury, such as in the neck and chest, which may be rapidly fatal, most isolated peripheral vascular injuries are not immediately fatal and patients usually survive transportation to a medical center.2 Extremity vascular injury accounts for up to 50% of all arterial injuries seen at civilian trauma centers. Although the exact incidence of peripheral vascular injuries is variable, upper and lower extremity vascular trauma has a similar incidence in an urban setting. Within the lower extremity, femoral arterial injuries are more common than popliteal injuries and account for up to 70% of all lower vascular injuries treated in urban trauma centers.4–15
DIAGNOSIS
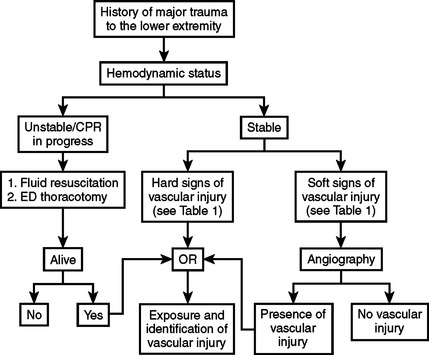
The diagnosis of peripheral vascular trauma can usually be made based on a quick history and physical examination of the extremity, including a systematic and thorough neurovascular evaluation (Figure 1). There are a multitude of signs of vascular injury on examination. They are divided into hard and soft signs and reflect the likelihood that a significant vascular injury is present. Hard signs (Table 1) indicate a high likelihood that a significant vascular injury is present. Thus, patients with hard signs should be taken directly to the operating room to undergo immediate operative management.2 Patients with soft signs of vascular injury (see Table 1) are less likely to have a significant vascular injury. This, however, must be confirmed using more invasive diagnostic modalities. Arteriography is currently the best available modality for the diagnosis of vascular injury in stable patients with soft signs of vascular injury but without evidence of peripheral ischemia. It can also be used in selected cases where the exact location of the injury is difficult to determine (e.g., pellet wounds or multiple gunshot wounds) and where the optimal incision and approach cannot be determined a priori. Arteriography can be performed in the angiography suite by an interventional radiologist or intraoperatively by the surgeon. It can be time consuming, but it is both sensitive and specific in the diagnosis of extremity vascular injury. Spiral computed tomographic angiography (CT-A) with the newest generation of high-speed scanner is an alternative diagnostic modality that has not yet been fully evaluated or widely accepted. It is rapid and does not require arterial catheterization. It does require contrast infusion, has no therapeutic potential, and can be limited by the artifacts generated if foreign bodies are present in the extremity.2
| Hard Signs |
The types of arterial trauma that have been described include laceration, transaction (complete or partial), contusion (with or without thrombosis), aneurysm (true or false), arteriovenous (AV) fistula, intimal disruption, and external compression by a hematoma. Lacerations and transections account for the great majority of arterial trauma.1
OPERATIVE MANAGEMENT FOR ALL PERIPHERAL VASCULAR INJURY
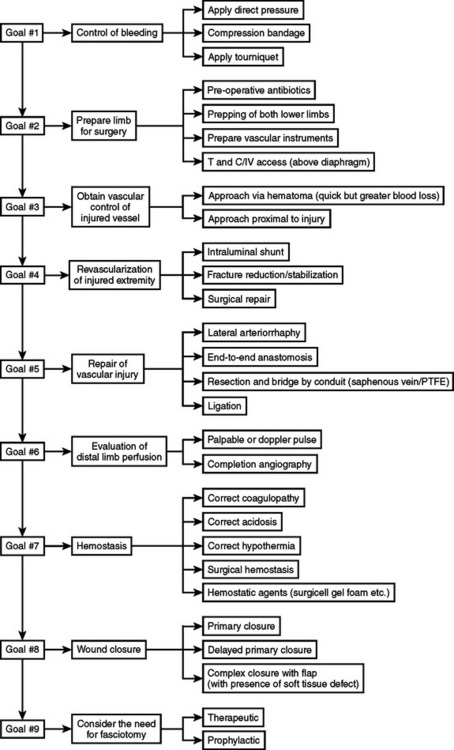
Preoperative Management
The initial objective in the management of peripheral vascular injury is to control bleeding to avoid exsanguination. This can immediately be accomplished using digital pressure, compressive bandages, or a tourniquet. Simultaneously, adequate fluid resuscitation is essential to limit the duration and extent of shock. Broad-spectrum antibiotics should also be administered in a timely fashion. Both groins, the lower abdomen, and both lower extremities should be prepped and draped. Prepping and draping the entire injured extremity including the distal aspect is important to assess for distal perfusion, assess the development of compartment syndrome, and perform fasciotomies if required. Prepping and draping the uninjured extremity allows for the harvesting of the greater saphenous vein if required to provide for a suitable replacement conduit. Vascular clamps, vessel loops, and fine monofilament sutures must be available before surgery begins.
Intraoperative Management
Controlling active bleeding before the start of the operation allows for sufficient time to obtain proximal and distal vascular control without further blood loss and prevents contamination of the surgical field by further bleeding. Approaching the hematoma directly may be useful in selected cases, but good judgment is required, as this can result in significant and potentially needless blood loss, which can further compromise the patient’s hemodynamic and metabolic status, leading to a poor outcome. The cornerstone principle is to obtain proximal and distal control rapidly along with revascularization of the injured extremity. Surgical repair and temporary shunting are the main two options. The use of intraluminal shunt is advisable in patients who cannot tolerate surgical repair because of extreme systemic abnormalities such as acidosis, hypothermia, and coagulopathy. Also, when fracture stabilization may compromise the vascular repair, shunting should be performed before definitive vascular repair (Figure 2).
Approach to Specific Vascular Injuries
Femoral Artery
The common femoral artery (CFA) is exposed via a longitudinal incision approximately 10 cm long placed over its course from the inguinal ligament inferiorly. If proximal control is needed, the external iliac artery must be explored and controlled. Using a similar incision, the profunda FA can be exposed and identified via a posterior lateral approach around the take-off of a superficial FA. Direct repair of the CFA is preferred; however, if a longitudinal injury or defect is identified, a vein patch may be necessary to preserve lumen diameter and avoid stenosis of the repair. An interposition graft is mandated when significant loss of artery has occurred, making it impossible to perform a tension free repair. Options for interposition grafts include the greater saphenous vein or synthetic grafts such as Dacron or PTFE with acceptable long-term patency rates. Profunda FA should be ligated when the patient is unstable or if serious associated injuries are present. It should be repaired if possible, but long-term complications are rare. The superficial FA courses deeper as it moves more distally. Because of their location, vascular injuries related to femur shaft fractures typically involve the superficial FA. The proximal portion is best exposed via a longitudinal groin incision as described previously; the middle and distal portion require an oblique incision in the thigh along the course of the sartorius muscle. Repair of this injury follows the same principles as those of the CFA described previously. However, patency rates using synthetic grafts are significantly lower than those for autologous vein graft, and therefore should be used in limited cases.2
MORBIDITY AND COMPLICATIONS
The most dangerous complications in the postoperative period are bleeding and thrombosis. Bleeding from the vascular repair may result in rapid swelling of the leg or external bleeding. This can be a life-threatening complication and mandates immediate return to the operating room for re-exploration and control of bleeding. At the same time, any coagulopathy should be corrected promptly. Arterial thrombosis at the site of the repair is suspected when the pulses are diminished or lost in the injured leg. Immediate return to the operating room to evaluate the vascular repair and to perform thrombectomy is essential to salvage the limb. The development of edema in the injured limb can result from thrombosis of the venous repair. Other complications include wound infection and deep infection at the site of the vascular repair. Delayed complications include stenosis and late thrombosis, pseudoaneurysm, and AV fistula. The surgical management of these complications is beyond the scope of this chapter. Chronic venous insufficiency has been associated with fourcompartment fasciotomy.1
OUTCOME
There are three main outcomes after peripheral vascular trauma of the lower extremity: mortality rate, amputation rate, and functional outcome. The mortality rate after peripheral vascular injury has reached the lowest levels ever reported (<5%). This is attributable to rapid transport to a trauma center, adequate and prompt resuscitation, rapid diagnosis and treatment, and the use of damage control under the appropriate settings. In addition, the amputation rate has also dramatically improved (<2%), because of the institution of maneuvers resulting in abbreviated warm ischemia time. These include rapid transport from the scene to the operating room, better resuscitation, using intraluminal shunts, early stabilization of fractures, and liberal use of fasciotomy. The reported amputation rate after lower extremity vascular injury is highly variable.1–3,16–19 Amputation rates for femoral artery injuries range from 0%–5%, and are much lower than those reported for popliteal injuries, which range from 0%–42%. Furthermore, any associated vein injury requiring ligation worsens the overall outcome and increases the amputation rate in the injured limb. A recently published study on blunt vascular trauma to the extremity reported that blunt vascular injuries reported an 18% amputation rate, which is considered to be three times the rate resulting from penetrating injuries. Higher amputation rates have been attributed to a delay in diagnosis as well as the presence of more significant injuries that delay the management of the extremity injury. Finally, the long-term functional outcomes of limbs with vascular trauma remain under-reported because of poor follow-up in this patient population, warranting further investigation.1 A recent study20 dealing with lower extremity injury reported that in limbs at high risk for amputation, reconstruction versus amputation results in equivalent functional outcome at 2 years after injuries.
1 Shackford SR, Rich NM. Peripheral vascular injury. Trauma. 4th ed. New York: McGraw-Hill; 2000.
2 Sise MJ, Shackford SR. Extremity vascular trauma. In: Rich N, Mattox KL, Hirshberg A, editors. Vascular Trauma. 2nd ed. Philadelphia: Elsevier Saunders; 2004:353-393.
3 Rich NM. Vascular trauma. Surg Clin North Am. 1973;53(6):1367-1392.
4 DeBakey ME, Simeone F. Battle injuries of the arteries in WWII: an analysis of 2471 cases. Ann Surg. 1946;123(4):534-579.
5 Jahnke EJJr, Seeley SF. Acute vascular injuries in the Korean War: an analysis of 77 consecutive cases. Ann Surg. 1953;138(2):158-177.
6 Hughes CW. Acute vascular trauma in Korean War casualties: an analysis of 180 cases. Surg Gyne Obst. 1954;99(20):91-100.
7 Rich NM, Baugh JH, Hughes CW. Acute arterial injuries Vietnam: 1000 cases. J Trauma. 1970;10(5):359-369.
8 Cargile JS, Hunt JL, Purdue GF. Acute trauma of the femoral artery and vein. J Trauma. 1992;32(3):364-370.
9 Degiannis E, Levy RD, Velmahos GC, Potokar R, Saadia R. Penetrating injuries to the femoral artery. Br J Surg. 1995;82(4):492-493.
10 Feliciano DV, Bitondo CG, Mattox KL. Civilian trauma in the 1980’s: a one year experience with 456 vascular and cardiac injuries. Ann Surg. 1984;199:717-724.
11 Carrillo EH, Spain DA, Miller FB, Richardson JD. Femoral vessel injuries in vascular trauma: complex and challenging injuries. Surg Clin North Am. 2002;82(1):49-65.
12 Richa NM, Hobson RW, Fedde CW, Collins GJ. Acute femoral arterial trauma. J Trauma. 1975;15(8):628-637.
13 Phifer TJ, Gerlock AJ, Vekovius WA, Rich NM, McDonald JC. Amputation risk factors in concomitant superficial femoral artery and vein injuries. Ann Surg. 1984;199(4):241-243.
14 Weaver FA, Rosenthal RE, Waterhouse G, Adkins RB. Combined skeletal and vascular injuries of the lower extremities. Am Surg. 1984;50:189-197.
15 Drost TF, Rosemurgy AS, Proctor D, Kearney RF. Outcome of treatment of combined orthopedic and arterial trauma to the lower extremity. J Trauma. 1989;29(10):1331-1334.
16 Reynolds R, McDowell HA, Diethelm AG. The surgical treatment of blunt and penetrating injuries of the popliteal artery. Am Surg. 1983;49(8):405-410.
17 Ashworth EM, Dalsing MC, Glover JL, Reilly MK. Lower extremity vascular trauma: a comprehensive aggressive approach. J Trauma. 1988;28(3):329-336.
18 Nanbashvili J, Kopadze T, Tvaladze M, Buachidze T, Nazvlishvili G. War injuries of major extremity arteries. World J Surg. 2003;27(2):134-139.
19 Feliciano DV, Herskowitz K, O’Gorman RB, Cruse PA, Brandt ML, Burch JM, Mattox KL. Management of vascular injuries in the lower extremities. J Trauma. 1988;28(3):319-328.
20 Bosse MJ, MacKenzie EJ, Kellam JF, Burgess AR, et al. An analysis of outcomes of reconstruction or amputation of leg-threatening injuries. N Engl J Med. 2002;347(24):1924-1931.
21 Asensio JA, Kuncir EV, Garcia-Nunez LM, Petrone P. Femoral vessel injuries: analysis of factors predictive of outcomes. J Am Coll Surg. 2006;203:512-520.