CHAPTER 62 LOW CEREBROSPINAL FLUID HEADACHE
BACKGROUND AND TERMINOLOGY
In 1938, Schaltenbrand used the term aliquorrhea to describe the spontaneous occurrence of an entity manifested by very low cerebrospinal fluid (CSF) opening pressures and orthostatic headaches, among other features.1,2 Sometimes referred to as Schaltenbrand’s headaches, this later came to be known as spontaneous intracranial hypotension.3 It is now realized that practically all cases of spontaneous intracranial hypotension result from spontaneous CSF leaks,4 often at the level of the spine (particularly the thoracic spine5) and only rarely at the skull base. CSF leak leads to CSF volume depletion. Terms such as spontaneous CSF leak, CSF hypovolemia, and CSF volume depletion have been used interchangeably with spontaneous intracranial hypotension, because some patients with this disorder have consistently normal CSF opening pressures.5,6 True hypovolemic state (reduced total body water), CSF shunt overdrainage, dural holes or tears as the result of lumbar puncture, epidural catheterization, surgery, and trauma all may lead to loss of CSF volume. In this chapter, we focus on spontaneous CSF leaks.
ETIOLOGY OF SPONTANEOUS CEREBROSPINAL FLUID LEAKS
Some patients report a history of trivial trauma, such as coughing, pushing, trivial falls, lifting, and sports activities. Evidence for weakness of the dural sac is accumulating. Meningeal diverticula are seen more frequently in patients with spontaneous CSF leaks. Increased frequency of meningeal diverticula and also CSF leaks have been reported in Marfan’s syndrome.7–9 Some patients with spontaneous CSF leaks show stigmata of the disorders of a connective tissue matrix (e.g., marfanoid features, hyperflexible joints, hyperextensible skin).5,10
In uncommon instances, a dural tear from a spondylotic spur or disc herniation11,12 may cause dural defect and CSF leak.
CLINICAL MANIFESTATIONS
Headache is the most common manifestation. It is “classically” orthostatic (present in upright position, relieved by recumbency).3,5 It is often not throbbing, but it may be throbbing; it is often bilateral, but it may be unilateral; and it is often aggravated or sometimes even triggered by Valsalva-type maneuvers. The headache may be frontal, fronto-occipital, holocephalic, or occipital. Not all headaches in CSF leaks are orthostatic, and variability is substantial (Table 62-1).5,13–17 Furthermore, not all orthostatic headaches result from CSF leaks. For example, they can be the dominant clinical manifestation in some patients with postural tachycardia syndrome.18
TABLE 62-1 Headache Variations in Cerebrospinal Fluid (CSF) Leaks
MRI, magnetic resonance imaging.
CLINICAL MANIFESTATIONS OTHER THAN HEADACHES
Many of the patients with spontaneous CSF leaks have one or, often, more symptoms in addition to the headaches (Table 62-2).3,5,19–32
|
Rare manifestations: facial numbness or weakness, diplopia due to third or fourth cranial nerve palsy,20–23 galactorrhea,24 Menière’s disease–like manifestations,25 upper limb radiculopathy,26 encephalopathy,27 stupor,28 coma,29 parkinsonism,30 ataxia, incontinence, gait unsteadiness,31 frontotemporal dementia32
|
Proposed mechanisms of clinical manifestations in CSF leaks and intracranial hypotension are listed in Table 62-3.3,5,19–34
TABLE 62-3 Mechanisms of Clinical Manifestations or Cerebrospinal Fluid Volume Depletion
| Clinical Manifestation | Proposed Mechanism |
|---|---|
| Headache | Descent of the brain, stretch and distortion of pain-sensitive suspending structures of the brain3,5,33,34,34a |
| Cranial nerve palsies | Stretching or compression of related cranial nerves19–23 |
| Dizziness, change in hearing | Stretching of eighth cranial nerve or pressure changes in perilymphatic fluid of the inner ear5,25 |
| Galactorrhea and increased prolactin | Distortion of pituitary stalk24 |
| Radicular upper limb symptoms | Stretching of cervical nerve roots or irritation by dilated epidural venous plexus5,26 |
| Encephalopathy, stupor, coma | Diencephalic compression27–29 |
| Cerebellar ataxia, parkinsonism | Compression of posterior fossa and deep midline structures30 |
| Frontotemporal dementia | Compression of frontotemporal lobes32 |
| Gait disorder | Spinal cord venous congestion31 |
DIAGNOSIS
Cerebrospinal Fluid Examination
Analysis reveals the following characteristics:
 Protein concentration: normal or elevated (protein concentrations up to 100 mg/dL are common, and a concentration up to 1000 mg/dL has been reported).15
Protein concentration: normal or elevated (protein concentrations up to 100 mg/dL are common, and a concentration up to 1000 mg/dL has been reported).15 Leukocyte count: normal or elevated (pleocytosis with counts up to 50 cells/mm3 is common, and a count up to 222 cells/mm3 has been reported).5
Leukocyte count: normal or elevated (pleocytosis with counts up to 50 cells/mm3 is common, and a count up to 222 cells/mm3 has been reported).5Radioisotope Cisternography
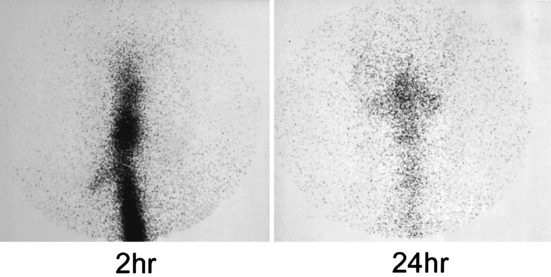
Indium 111 is the radioisotope of choice. This is introduced intrathecally, typically through a lumbar puncture, and its movement is monitored by sequential scanning at various intervals, up to 24 or even 48 hours. Normally, by 24 hours (but often earlier), substantial radioactivity can be detected over the cerebral convexities. When a spinal CSF leak exists, the activity typically does not extend much beyond the basal cisterns. Therefore, images at 24 or even 48 hours reveal either absence or paucity of activity over the cerebral convexities.35–37 This finding is the most common cisternographic abnormality in CSF leaks. Detection of parathecal activity that may point to the level or approximate site of the leak, although more desirable, is noted much less commonly (Fig. 62-1). Furthermore, meningeal diverticula, if large enough, may appear as foci of parathecal activity. Another cisternographic observation in CSF leaks is the early appearance of radioactivity in the kidneys and urinary bladder (<4 hours versus 6 to 24 hours), indicative of early entrance of extravasated isotope into the venous system and its early renal clearance and early appearance in the urinary bladder.
Magnetic Resonance Imaging
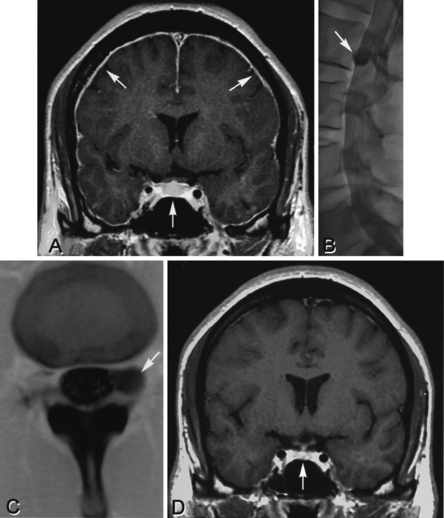
Magnetic resonance imaging (MRI) has truly revolutionized the diagnosis of spontaneous CSF leaks and has been instrumental in recognizing its broad clinical spectrum. Head and spine MRI abnormalities are listed in Table 62-4.
MRI, magnetic resonance imaging.
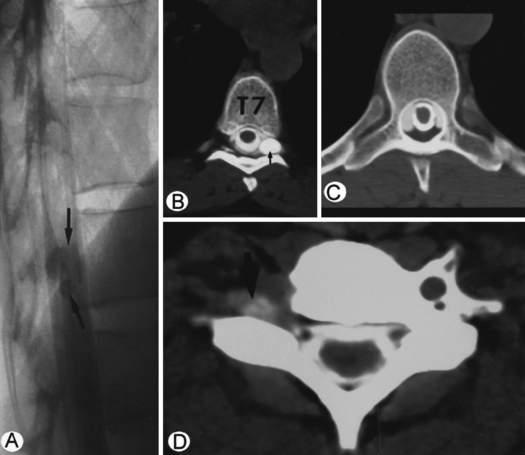
Computed Tomographic Myelography
Computed tomographic myelography (CTM) is myelography with water-soluble contrast material, followed by CT, typically at each spinal level, unless the myelogram itself or a previous cisternography or spine MRI reliably pointed to a more limited area of the spine to be investigated. CTM may show extra-arachnoid and extradural extravasation of contrast material (and therefore, the CSF) and so far is the most reliable test for locating the actual site of CSF leakage. It also shows meningeal diverticula and dilated nerve root sleeves and helps identify whether a noted meningeal diverticulum is the actual site of the CSF leak (Figs. 62-2B,C and 62-5).5 This test, like cisternography, also provides an opportunity to measure CSF opening pressure.
The rate of CSF leakage (fast-flow or slow-flow) may create special diagnostic challenges.
Fast-Flow Cerebrospinal Fluid Leaks
In this situation, after the myelogram and by the time of CT, a substantial amount of contrast has leaked and has spread across several spinal levels, making it virtually impossible to locate the exact site of the leakage. Dynamic CTM38 is often effective in solving this problem. In this technique, CT is performed immediately after intrathecal injection of contrast material, and high-speed multidetector spiral CT (which allows obtaining many cuts in a short period of time) is used. This technique is quite effective in detecting fast-flow CSF leaks as well as leaks from multiple sites.
Slow-Flow Cerebrospinal Fluid Leaks
When the leaks are slow, even after CTM, not enough contrast material has leaked to allow detection. A delayed CT, 3 to 4 hours after the initial one, sometimes reveals the site of the leak. Magnetic resonance myelography (spine MRI after intrathecal introduction of gadolinium), a test that awaits more confirmation and experience, may also prove to be helpful, inasmuch as images delayed as long as 72 or even 96 hours may be obtained.39
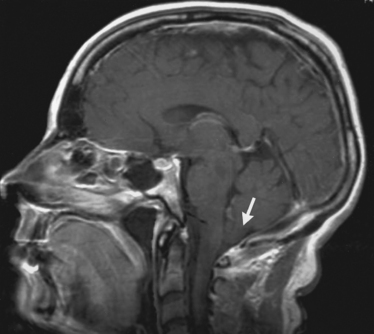
MECHANISMS OF MAGNETIC RESONANCE IMAGING ABNORMALITIES
CSF volume depletion leads to (1) ventricular collapse and decrease in the size of the ventricles and (2) sinking of the brain (and, therefore, descent of the cerebellar tonsils [Fig. 62-3], decrease in the sizes of prepontine and perichiasmatic cisterns, flattening of the optic chiasm, and crowding of the posterior fossa). Furthermore, the loss of CSF volume, according to the Monro-Kellie doctrine,40 mandates replacement of the depleted CSF volume, which is accomplished mainly by an intracranial venous hypervolemia. This results in (1) meningeal venous hyperemia, leading to diffuse pachymeningeal enhancement with gadolinium (leptomeninges have blood-brain barriers, but pachymeninges do not and, therefore, it is only the pachymeninges that enhance)41; (2) enlargement of the pituitary gland as the result of pituitary hyperemia; and (3) engorgement of cerebral venous sinuses. Subdural fluid collections are also volume-compensatory phenomena. At the spine level, CSF volume depletion and relative collapse of the spinal dura lead to engorgement of the epidural venous plexus.15
CONSIDERABLE VARIABILITY
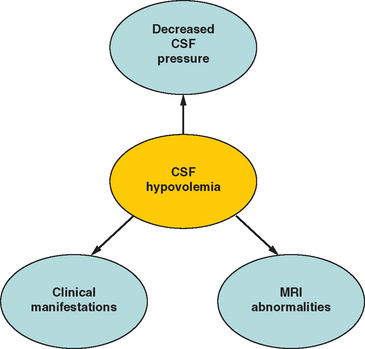
In spontaneous CSF leaks, clinical manifestations (including headaches), imaging findings, and CSF abnormalities (including opening pressures, which may range from unmeasurable to entirely normal) exhibit considerable variability. The core pathogenetic factor in this disorder is loss of CSF volume (CSF hypovolemia), which is the independent variable, whereas CSF pressures, imaging abnormalities, and clinical manifestations are variables dependent on the CSF volume (Fig. 62-6).4
TREATMENT
A variety of treatment modalities have been advocated in the management of patients with intracranial hypotension or spontaneous CSF leaks (Table 62-5). Some of these are based on previous experience with post–lumbar puncture headaches rather than direct experience with spontaneous CSF leaks.
Fortunately, in some patients, the leak stops or slows spontaneously and the symptoms resolve. Bed rest has been traditionally recommended. Because many such patients have orthostatic symptoms, they tend to remain recumbent much of the time anyway.
Caffeine and theophylline, according to some studies,42 are mildly effective, but this effectiveness is doubtful to be impressive or durable.
Sporadic reports of successful results with epidural saline infusion exist,43 but the experience is limited. This procedure can be tried, but with limited expectations, in patients in whom repeated epidural blood patches (EBPs) have failed. Reports, mostly anecdotal,44 have mentioned the efficacy of epidural dextran injections. Intradural fluid infusions have been effective but typically only for as long as the CSF volume loss is thus compensated. However, in rare cases of rapid deterioration with obtundation or coma, intrathecal fluid injections may prove helpful.45 Overall, the concern is about complications such as infections in sustained epidural and intrathecal infusions.
EBP has emerged as the treatment of choice for patients in whom initial conservative management has failed.46,47 The effect of EBP may be transient or sustained. EBP has an early effect that is simply a volume replacement resulting from the tamponade effect of the volume of the epidurally introduced blood, as well as a latent effect related to complete or partial sealing of the leak. A durable response is noted in approximately one third of patients with each EBP.47 Thus, many patients may require more than one EBP. The efficacy of EBP in spontaneous CSF leaks is much less than what is seen in post–lumbar puncture headaches or even in the leaks that may follow epidural catheterizations. This difference is related mostly to the complex anatomy of the spontaneous CSF leaks (often not a simple rent or hole) but also to the site of the leak (which may not be in the posterior aspect of the dura or may be distant from the site where EBP is delivered).
Sporadic reports on the effectiveness of epidural injection of fibrin glue48 are encouraging. It can be an alternative when EBPs fail.
Surgery in well-selected cases is effective and can be tried when conservative and less invasive approaches, such as EBPs, have failed.49 The surgery, however, may not be entirely straightforward, mostly as the result of the complexity of the anatomy of the leak. Besides, occasional patients have leaks at multiple sites.38 It is essential to determine the site of the CSF leak and perform a thorough preoperative workup before surgery is undertaken.
COMPLICATIONS
The major complication of spontaneous CSF leak is the development of symptomatic unilateral or bilateral subdural hematomas, which may create significant therapeutic challenges.50,51 Cerebral venous sinus thrombosis, an uncommon complication of spontaneous CSF leak, has been occasionally reported.52
After treatment of spontaneous CSF leaks, whether by EBP or by surgery, sometimes a symptomatic rebound syndrome of intracranial hypertension may develop.53 This is typically self-limited. Treatment with acetazolamide has shown encouraging results.
1 Schaltenbrand G. Neure anschauungen zur pathophysiologie der liquorzirkulation. Zentrablbl Neurochir. 1938;3:290-300.
2 Schaltenbrand G. Normal and pathological physiology of the cerebrospinal fluid circulation. Lancet. 1953;1:805-808.
3 Chung SJ, Kim JS, Lee MC. Syndrome of cerebrospinal fluid hypovolemia: clinical and imaging features and outcome. Neurology. 2000;55:1321-1327.
4 Mokri B. Spontaneous cerebrospinal fluid leaks: from intracranial hypotension to cerebrospinal fluid hypovolemia—evolution of a concept. Mayo Clin Proc. 1999;74:1113-1123.
5 Mokri B, Piepgras DG, Miller GM. Syndrome of orthostatic headaches and diffuse pachymeningeal gadolinium enhancement. Mayo Clin Proc. 1997;72:400-413.
6 Miyazawa K, Shiga Y, Hasegawa T, et al. CSF hypovolemia vs intracranial hypotension in “spontaneous intracranial hypotension syndrome.”. Neurology. 2003;60:941-947.
7 Davenport RJ, Chataway SJ, Warlow CP. Spontaneous intracranial hypotension from a CSF leak in a patient with Marfan’s syndrome. J. Neurol Neurosurg Psychiatry. 1995;59:516-519.
8 Fukutake T, Sakakibara R, Mori M, et al. Chronic intractable headache in a patient with Marfan’s syndrome. Headache. 1997;37:291-295.
9 Schriver I, Schievink WI, Godfrey M, et al. Spontaneous spinal cerebrospinal fluid leaks and minor skeletal features of Marfan’s syndrome: a microfibrillonopathy. J Neurosurg. 2002;96:483-489.
10 Mokri B, Maher CO, Sencakova D. Spontaneous CSF leaks: underlying disorder of connective tissue. Neurology. 2002;58:814-816.
11 Eros EJ, Dodick DW, Nelson KD. Orthostatic headache syndrome with CSF leak secondary to bony pathology of the cervical spine. Cephalalgia. 2002;22:439-443.
12 Winter SCA, Maartens NF, Anslow P, et al: Spontaneous intracranial hypotension due to thoracic disc herniation. J Neurosurg 96(3, Suppl):343–345.
13 Schievnik WI, Wijdicks EFM, Meyer FB, et al. Spontaneous intracranial hypotension mimicking aneurysmal subarachnoid hemorrhage. Neurosurgery. 2001;48:513-557.
14 Mokri B, Aksamit AJ, Atkinson JLD. Paradoxical postural headache in spontaneous CSF leaks. Cephalalgia. 2004;24:883-886.
15 Mokri B. Low cerebrospinal fluid pressure syndromes. Neurol Clin North Am. 2004;22:55-74.
16 Mokri B. Spontaneous CSF leaks mimicking benign exertional headaches. Cephalalgia. 2002;22:780-783.
17 Mokri B, Atkinson JLD, Piepgras DG. Absent headaches despite CSF volume depletion (intracranial hypotension). Neurology. 2000;55:573-575.
18 Mokri B, Low PA. Orthostatic headaches without CSF leak in postural tachycardia syndrome. Neurology. 2003;61:980-982.
19 Horton JC, Fishman RA. Neurovisual findings in the syndrome of spontaneous intracranial hypotension from dural cerebrospinal fluid leak. Ophthalmology. 1994;101:244-251.
20 Brady-McCreery K, Spiedel S, Hussein MAW, et al. Spontaneous intracranial hypotension with unique strabismus due to third and fourth cranial neuropathies. Binocul Vis Strabismus Q. 2002;17:43-48.
21 Follens I, Evans PA, Tassignon MJ. Combined fourth and sixth cranial nerve palsy after lumbar puncture: a rare complication. Bull Soc Belge Ophthalmol. 2001;281:29-33.
22 Warner GT. Spontaneous intracranial hypotension causing a partial third cranial nerve palsy: a novel observation. Cephalalgia. 2002;22:822-823.
23 Ferrante E, Svaino A, Briuschia A, et al. Transient oculomotor cranial nerve palsy in spontaneous intracranial hypotension. J Neurosurg Sci. 1998;42:177-179.
24 Yamamoto M, Suehiro T, Nakata H, et al. Primary low cerebrospinal fluid pressure syndrome associated with galactorrhea. Intern Med. 1993;32:228-321.
25 Portier F, de Minteguiaga C, Racy E, et al. Spontaneous intracranial hypotension: a rare cause of labyrinthine hydrops. Ann Otol Rhinol Laryngol. 2002;111:817-820.
26 Albayram S, Wasserman BA, Yousem DM, et al. Intracranial hypotension as a cause of radiculopathy from cervical epidural venous engorgement: case report. AJNR Am J Neuroradiol. 2002;23:618-621.
27 Beck CE, Rzk NW, Kiger LT, et al. Intracranial hypotension presenting with severe encephalopathy: case report. J Neurosurg. 1998;89:470-473.
28 Pleasure SJ, Abosch A, Friedman J, et al. Spontaneous intracranial hypotension resulting in stupor caused by diencephalic compression. Neurology. 1998;50:1854-1857.
29 Evans RW, Mokri B. Spontaneous intracranial hypotension resulting in coma. Headache. 2002;24:159-160.
30 Pakiam AS, Lee C, Lang AE. Intracranial hypotension with parkinsonism, ataxia, and bulbar weakness. Arch Neurol. 1999;56:869-872.
31 Nowak DA, Radiek SO, Zinner J, et al. Broadening of the clinical spectrum: unusual presentation of spontaneous cerebrospinal fluid hypovolemia: case report. J Neurosurg. 2003;98:903-907.
32 Hong M, Shah GV, Adams KM, et al. Spontaneous intracranial hypotension causing reversible frontotemporal dementia. Neurology. 2002;58:1285-1287.
33 Fay T. Mechanism of headache. Arch Neurol Psychiatry. 1937;37:471-474.
34 Mokri B: Cerebrospinal fluid volume depletion and its emerging clinical/imaging syndromes. Neurosurg Focus 2000; 9(1, article 6).
34a Fishman RA. Cerebrospinal Fluid in Diseases of the Nervous System, 2nd ed., Philadelphia: WB Saunders; 1992:84-87. 152–155.
35 Benamer M, Tainturier C, Graveleau P, et al. Radionuclide cisternography in spontaneous intracranial hypotension. Clin Nucl Med. 1998;23:150-151.
36 Bai J, Yokoyama K, Kinuya S, et al. Radionuclide cisternography in intracranial hypotension syndrome. Ann Nucl Med. 2002;16:75-78.
37 Spell L, Boulin A, Tainturier C, et al. Neuroimaging features of spontaneous intracranial hypotension. Neuroradiology. 2001;43:622-627.
38 Leutmer PH, Mokri B. Dynamic CT myelography: a technique for localizing high-flow spinal cerebrospinal fluid leaks. AJNR Am J Neuroradiol. 2003;24:1711-1714.
39 Tali ET, Ercan N, Krumina G, et al. Intrathecal gadolinium (gadopentetate dimeglumine). Enhanced magnetic resonance myelography and cisternography. Results of a multicenter study. Invest Radiol. 2002;37:152-159.
40 Mokri B. The Monro-Kellie hypothesis: applications in CSF volume depletion. Neurology. 2001;56:1746-1748.
41 Fishman RA, Dillon WP. Dural enhancement and cerebral displacement secondary to intracranial hypotension. Neurology. 1993;43:609-611.
42 Vilmig ST, Titus F. Low cerebrospinal fluid pressure. In: Olesem J, Tfelt-Hansen P, Welch KMA, editors. The Headache. New York: Raven Press; 1993:687-695.
43 Gibson BE, Wedel DJ, Faust RJ, et al. Continuous epidural saline infusion for the treatment of low CSF pressure headache. Anesthesiology. 1988;48:789-791.
44 Aldrete JA. Persistent post-dural–puncture headache treated with epidural infusion of dextran. Headache. 1994;34:265-267.
45 Binder DK, Dillon WP, Fishman RA. Intrathecal saline infusion in the treatment of obtundation associated with spontaneous intracranial hypotension. Technical case report. Neurosurgery. 2002;51:830-837.
46 Duffy PJ, Crosby ET. The epidural blood patch. Resolving the controversies. Can J Anaesth. 1999;46:878-886.
47 Sencakova D, Mokri B, McClelland RL. The efficacy of epidural blood patch in spontaneous CSF leaks. Neurology. 2001;57:1921-1923.
48 Cru JBP, Gerritse BM, Van Dongen RTM, et al. Epidural fibrin glue injection stops persistent postdural puncture headache. Anesthesiology. 1999;91:576-577.
49 Scheivink WI, Morreale VM, Atkinson JLD, et al. Surgical treatment of spontaneous spinal cerebrospinal fluid leaks. J Neurosurg. 1998;88:243-246.
50 De Noronha RJ, Sharrack B, Hadjivassiliou M, et al. Subdural hematoma: a potentially serious consequence of spontaneous intracranial hypotension. J Neurol Neurosurg Psychiatry. 2003;74:752-755.
51 Augustin J, Proust F, Verdure L, et al. [Bilateral chronic subdural hematoma: spontaneous intracranial hypotension?]. Neurochirurgie. 2003;49:47-50.
52 Berroir S, Grabli D, Heran F, et al. Cerebral venous sinus thrombosis in two patients with spontaneous intracranial hypotension. Cerebrovasc Dis. 2004;17:9-12.
53 Mokri B. Intracranial hypertension after treatment of spontaneous cerebrospinal fluid leaks. Mayo Clin Proc. 2002;77:1241-1246.
54 Pannullo SC, Reich JB, Krol G, et al. MRI changes in intracranial hypotension. Neurology. 1993;43:919-926.
55 Atkinson JLD, Weinshenker BG, Miller GM, et al. Acquired Chiari I malformation secondary to spontaneous spinal cerebrospinal fluid leakage and chronic intracranial hypotension syndrome in seven cases. J Neurosurg. 1988;88:237-242.
56 Mokri B, Atkinson JLD. False pituitary tumor in CSF leaks. Neurology. 2000;55:573-575.
57 Alvarez-Linera J, Escribano J, Benito-Leon J, et al. Pituitary enlargement in patients with intracranial hypotension syndrome. Neurology. 2000;55:1895-1897.
58 Bakshi R, Mechtler LL, Kamran S, et al. MRI findings in lumbar puncture headache syndrome: abnormal duralmeningeal and dural venous sinus enhancement. Clin Imaging. 1999;23:73-76.
59 Rabin BM, Roychowdhury S, Meyer JR, et al. Spontaneous intracranial hypotension: spinal MRI findings. AJNR Am J Neuroradiol. 1998;19:1034-1039.
60 Chiapparini L, Farina L, D’Incerti L, et al. Spinal radiological findings in nine patients with spontaneous intracranial hypotension. Neuroradiology. 2002;44:143-150.
61 Moayeri NN, Henson JW, Schaefer PW, et al. Spinal dural enhancement on magnetic resonance imaging associated with spontaneous intracranial hypotension. J Neurosurg. 1998;88:912-918.
62 Mokri B. Headaches caused by decreased intracranial pressure: diagnosis and management. Curr Opin Neurol. 2003;16:319-326.