CHAPTER 123 Low Back Pain and Pregnancy – Examination and Diagnostic Work-up in the Pregnant Patient
INTRODUCTION
Nearly any medical condition that can occur in the nonpregnant state can occur during pregnancy. In fact, because of the pregnant state, women can potentially be at higher risk of misdiagnosis due to the overall general concept that all back pain in pregnancy is somewhat ‘normal’.1 Back pain in pregnancy is common, but when it becomes disabling it demands further diagnostic evaluation. Estimates of incidence are 50–70%.2 One prospective study of back pain in pregnancy showed a prevalence rate of 60%, with 30% of those patients reporting severe limitations in their daily activities.3
The physiologic changes of pregnancy may predispose women to back pain. The increased lumbar lordosis combined with the effects of the hormone relaxin on the joints of the lumbar spine and pelvis with the added weight of the gravid uterus result in a shift of the center of gravity anteriorly and an increased mechanical burden on the low back.2,4 The abdominal wall musculature of the abdominal cavity stretches as the gravid uterus grows. The force–tension curve of the lengthened abdominal muscles restrict their contractile strength while the muscles of the low back work harder to maintain upright posture. The muscles of the pelvic floor will bear the weight of the growing uterus and will eventually allow passage of the fetus. Relaxin is a polypeptide hormone secreted by the corpus lutea and has been identified as the major contributor to joint laxity during pregnancy.4 It is dramatically elevated during the first trimester, declines early in the second trimester to a level that remains stable throughout the pregnancy,4 and then declines sharply after delivery. Widening of the symphysis pubis and increased mobility of the sacroiliac synchondroses begins in the tenth to twelfth week of pregnancy as a result of relaxin.5 The strong sacroiliac ligament which normally resists forward flexion of the ala will become lax with the effects of relaxin.5 Weight gain, maternal obesity, and fetal weight at term have not been found to be related to pregnancy-related back pain.6 Other studies have shown that low back pain prior to or during a previous pregnancy, nulliparity with increased body mass index (BMI), lower socioeconomic status, and placenta with a posterior fundal location were found to be risk factors for back pain in pregnancy.35 A spectrum of clinical symptoms may be produced by the physiologic changes of pregnancy. However, the differential diagnosis of back pain in pregnancy should not be limited to pregnancy-related changes in the musculoskeletal system.
Clinical entities implicated as causes of back pain in pregnancy in one review article include: pelvic insufficiency (pain), sacroiliac joint (SIJ) subluxation, sciatica, lumbosacral disc pathology, spondylolisthesis, postural back pain and lumbar lordosis, thoracic back pain and coccydynia.6 Other studies have also included hip pathology, such as osteonecrosis of the femoral head and transient osteoporosis of pregnancy, as a potential cause of referred back pain.5 Other known causes of back pain include neurologic etiologies such as radiculopathy or plexopathy, vertebral segmental dysfunction, tumor, or fracture of the sacrum or pelvis. There is also growing evidence that the pelvic floor musculature is a pain generator, especially in relation to coccydynia and dyspareunia (Table 123.1).
| GENITOURINARY | |
|---|---|
| Urinary tract infection | |
| Kidney stones | |
| Pyelonephritis | |
| Cystitis | |
| Urethritis | |
| GYNECOLOGIC | |
| Ovarian cyst or torsion | |
| Uterine dysfunction or placental abnormality | |
| Pelvic inflammatory disease | |
| GASTROINTESTINAL | |
| Constipation | |
| Hemorrhoids | |
| Irritable bowel syndrome | |
| Hernia |
PELVIC OBLIQUITY
The pelvis is a ring comprised of two innominate bones that are connected anteriorly by the pubic symphysis and posteriorly to either side of the sacrum by the SIJ. The pelvis is dynamic or more mobile in the pregnant state as a result of the influence of relaxin on the ligamentous structures. Laxity itself is widespread and does not necessarily result in pain. Asymmetry of any part of the ring will cause dysfunction on the opposite side, i.e. dysfunction of the posterior pelvis will result in asymmetry and dysfunction of the anterior pelvis. They do not occur in isolation. However, there is a clear relation between asymmetric laxity of the SI joints and pregnancy-related pelvic pain (PRPP).8
There is an array of nomenclature to describe a given obliquity. By convention, dysfunction of pelvic ring is named on the hypomobile side. However, anecdotally, in the pregnant state the hypermobile side on physical examination can correlate with the side of pain. Damen et al. studied the prognostic value of laxity in assessing pain postpartum. Asymmetric laxity of the SI joints in pregnancy was believed to increase the presence of pelvic pain postpartum by as much as threefold.9,10 This speaks to treatment of asymmetry of the SI joint and its associated pain during pregnancy to prevent future back pain.
In pregnancy, the innominate obliquity is commonly named for the side which gives the patient pain in order to best direct the physical therapy prescription. A number of anatomic landmarks are used to determine pelvic obliquity: the iliac crest, the posterior superior iliac spine (PSIS), the anterior superior iliac spine (ASIS), and the pubic tubercles. The inferior lateral angle of the sacrum (ILA) can also be assessed to further delineate asymmetric sacral positioning in relation to ilial positioning. By measuring the side-to-side difference between these landmarks, the type of obliquity can be determined. A problematic hemipelvis can be rotated anteriorly or posteriorly, sheared superiorly (upslip) or inferiorly (downslip), inflared or outflared. Sacral positioning can be described similarly.11
SACROILIAC JOINT DYSFUNCTION
The sacroiliac joint is a true joint consisting of a synovial component inferiorly. It is auricular-shaped with the thinner sacral side lined with hyaline cartilage and the thicker ilial side with fibrocartilage. Primary innervation to this joint is thought to be from S1. Sturesson, in 1989, described true movement of the SIJ measuring approximately 1–3° of rotation.12 The sacroiliac joint has also been shown to be a potential generator of low back pain.13 In the pregnant patient, the potential for dysfunction is increased secondary to pregnancy-related hormone-induced ligamentous laxity and resultant asymmetry. It is thought that the laxity prepares for and facilitates delivery of the baby at term.14 Ostgaard, in a prospective study of back pain in 855 pregnant women, found an incidence of 19% with sacroiliac pain in week 30 of gestation.15 Additionally, Damen showed that in pregnant patients who were evaluated by Doppler imaging of vibrations there was found to be a definite relationship between asymmetric laxity of the sacroiliac joints and pregnancy-related pelvic pain.8 Patients typically report pain over the sacrum or the sacral sulcus. Transitional motions, particularly while turning in bed and arising from the seated to the standing position frequently triggers or exacerbates the presenting symptoms. Physical examination maneuvers will be discussed later, but posterior pelvic pain provocation test and active straight leg raise testing are well-documented, reliable diagnostic tests to assess pregnancy-related sacroiliac joint pain.
PELVIC FLOOR MYOFASCIAL PAIN
When a pelvic obliquity is present, the resulting asymmetry affects the pelvic floor muscles that originate from and that are attached to the pelvic bones. With a pelvic obliquity, the attaching muscles will be either abnormally shortened or lengthened. A force–tension curve of these muscles will be shifted, thereby demonstrating their disadvantageous biomechanical state. As well, it is known that muscle injury and soreness are more selectively associated with eccentric contraction.15a-c An inherently lengthened muscle must also work harder to function properly, and if the external force on the muscular floor is greater than the force the muscles can generate, weakness may eventually develop in addition to or in conjunction with pain.
COCCYDYNIA
There is a blatant absence of literature guiding the evaluation of the coccyx in pregnancy; however, it can be easily done via rectal examination. A study by Maigne16 found that body mass index determines the manner by which a subject sits down and that pathologies were different in obese, normal weight, and thin patients. For a detailed description of the analyses in the nonpregnant patient the reader is referred to Chapter 120 by Yves Maigne. Hypermobility of the coccyx defined as coccygeal flexion exceeding 25° when the patient is in the sitting position as evaluated on plain radiograph was also a cause of coccydynia. The pregnant state lends itself to the potential of coccygeal dysfunction and pain with the acute increase of BMI over 9 months as well as ligamentous laxity that accompanies pregnancy as a result of relaxin and estrogen.
STRESS FRACTURE
Stress fracture is defined as fracture due to repetitive cyclic loading on normal bone, whereas insufficiency fracture occurs when normal forces are applied to abnormal bone. Stress insufficiency fracture occurs when repetitive cyclic loading occurs in the setting of abnormal bone. Any of these fractures at the level of the sacrum, pelvis, or hip may be the cause of back pain in the pregnant patient, similar to the nonpregnant patient. Fractures should be considered in a patient diagnosed with sacroiliac dysfunction which is not improving with medical rehabilitation and interventional spine techniques; in the case of known trauma; or in a patient with a prepartum history of amenorrhea, eating disorder, or known osteopenia (female athletic triad).17
Risk factors specific to pregnancy that predispose for sacral fatigue fractures include rapid or excessive weight gain in the third trimester, increased lumbar lordosis, pelvic instability due to relaxin effect, rapid vaginal delivery, and prolactin-induced transient osteopenia. These injuries should also be considered immediately postpartum in the breastfeeding patient. Polatti showed evidence of a progressive decline in bone mineral density (BMD) in lactating women over the first 6 months with increase in BMD following a 1-month weaning period.17a Calcium supplementation during lactation had only a transient effect in minimizing bone loss.
The imaging study of choice in pregnancy after the first trimester when there is a high suspicion of stress fracture is magnetic resonance imaging. A comprehensive literature review revealed several reported sacral fractures associated with pregnancy.18,19,19a
PUBIC SYMPHYSIS
Symphysitis and symphyseal separation
Pubic symphysis motion and asymmetry is seen during pregnancy. Anterior pain can be associated with this increased motion and simultaneously precipitate posterior pelvic or low back pain. Maximum widening of the pubic symphysis during pregnancy is considered to be 10 mm. By definition, pubic symphysis separation is a width greater than 10 mm and is usually seen after a traumatic labor and delivery. Bjorklund et al., in 2000, studied the association between symphyseal distention and pelvic pain and circulating relaxin levels in the pregnant patient.20 They found that severe pelvic pain during pregnancy was strongly associated with an increased symphyseal distention; however, relaxin levels were not associated with the degree of distention or with pelvic pain in pregnancy. Another study showed that the majority of pregnant women with symphyseal pain had an average pubic symphysis width of 9.5 mm or more via sonographic measurement. In comparison, the asymptomatic pregnant patient had an average width of 6.3 mm.21
Osteitis pubis
Acute pubic symphysis inflammation, which can begin in pregnancy in association with a pelvic obliquity, can often lead to a chronic, painful, noninfectious inflammatory condition known as osteitis pubis. Osteitis pubis has been described as a complication of various obstetrical and gynecological procedures, including vaginal deliveries.22 Periosteal trauma seems to be part of the initiating event, although there is controversy regarding the true pathophysiological nature of the disorder. One of the first cases cited in the obstetrical literature was a report of a patient with osteitis pubis after a traumatic forceps vaginal delivery. Wiltse and Frantz reported 10 cases associated with the pregnant state.23 As the pubic symphysis becomes more lax to allow passage of the fetus, there is potential for excess movement and trauma. Plain films are the imaging method of choice; however, radiographic findings often lag behind clinical symptoms. Typically, X-ray changes can be seen 4 weeks after the traumatic event, and include loss of smooth cortical bone and reactive sclerosis. Treatment needs to be initiated based on physical examination in the peripartum period to prevent chronic postpartum pain.
LUMBAR DISC HERNIATION
Although early studies by LaBan et al. in 198324 suggested that pregnancy was an independent risk factor for the development of a herniated disc, it has been proven in subsequent studies that the actual incidence of lumbar herniated disc is no greater for pregnant women than for the general population.2,4 It is an uncommon etiology of low back pain in pregnancy with an incidence of 1:10 000.24 Risk factors include prior history of low back pain, increased body mass index, and lower socioeconomic status. Advanced maternal age, birth weight, and primiparity are controversial risk factors. In the last 20 years, the incidence of women aged 30 years and older at delivery has increased from 17.7% to 30.2%.24a Since the inexorable alterations that occur as the degenerative disc cascade proceeds25 will be more prominent as a female ages, it is expected that the probability of pain emanating from degenerative disc disease will be higher in this group. Pain from lumbar degenerative disc disease should be considered in the pregnant and nonpregnant patient alike who complains of back pain, numbness and tingling, or with neurologic findings on examination. A thorough examination is critical to differentiate the symptoms of degenerative disc disease from the radicular pain of a herniated disc from SIJ dysfunction. It is important to note that patients can have SIJ dysfunction concurrently with an S1 radiculopathy. If there is progressive weakness or bowel or bladder incontinence in pregnancy associated with back pain, cauda equina syndrome must be ruled out. Immediate imaging with MRI and surgical referral, even in pregnancy, is warranted.
NEUROLOGIC CAUSES OF BACK PAIN IN PREGNANCY
Neurologic sequelae in pregnancy may or may not be related to lumbar pathology. Nerve disorders that occur in the nonpregnant state can occur in pregnancy though they are not well described in the literature. Patients may experience direct nerve trauma or peripheral neuropathy from other disease states such as diabetes. Lateral femoral cutaneous neuropathy, or meralgia parasthetica, is a sensory abnormality of the anterolateral thigh and is the most common nerve injury seen in pregnancy.26 This lesion can be seen in association with a pelvic obliquity (often a left innominate posterior rotation) and consequently in those with concomitant SIJ pain. Hence, early treatment of the pelvic obliquity may influence outcome and improve numbness. Although Wong et al. also described this as the most common immediate postpartum nerve injury, they found low incidences of nerve injuries in general (0.92%) after labor and delivery.27
True sciatic nerve pathology is only seen in 1% of the pregnant population, despite its overuse as a catchall diagnosis for back pain or radiating pain in pregnancy.3 More comprehensive neurologic studies, such as needle electromyography and nerve conduction studies, may need to be done to diagnose a true sciatic nerve lesion versus an S1 radiculopathy or sacroiliac joint pain referred in a neurologic distribution.
CONCOMITANT CONDITIONS
Musculoskeletal conditions in pregnancy
Hip pathology
Osteonecrosis of the hip and transient osteoporosis of pregnancy are two hip conditions that occur in the pregnant state and should be considered in the differential diagnosis. These are relevant to our discussion on back and pelvic pain because they may present with non-specific groin pain, pelvic pain, or low back pain. Osteonecrosis of the hip in pregnancy has not been completely elucidated.5 Cheng postulated that higher adrenocortical activity during pregnancy combined with increased stresses may predispose the pregnant patient to this condition.28 Transient osteoporosis of pregnancy is a rare disorder that occurs typically during the third trimester of pregnancy. Patients typically have hip pain with weight bearing, limited hip range of motion (ROM), and MRI evidence of osteoporosis of the femoral head with preservation of the joint space.29 Early diagnostic imaging is important because persistent weight bearing can lead to stress or occult fracture of the hip or pelvis.
Spondylolisthesis
Spondylolisthesis is a condition where there is sagittal plane translation or ‘slipping’ of one vertebra on the vertebra below it. This typically occurs when there are bilateral defects in the pars interarticularis, which allows this increase of movement of one vertebra on another. It most commonly occurs with L5 slipping forward on S1. Another form of spondylolisthesis is degenerative in nature and more commonly occurs in women. This form is more likely to occur with the L4 vertebra slipping forward on L5. Saraste, in 1986, found that there was no increase in slippage in women during pregnancy.30 However, Sanderson and Fraser, in 1996, found that women who had children had a higher incidence of spondylolisthesis than women who had never had children.31 In patients with a higher grade of spondylolisthesis, grade III or IV, extra caution should be taken to monitor changes in neurologic examination and increasing back pain in pregnancy.
EXAMINATION TECHNIQUES
Hip examination
Hip range of motion is examined with the patient in supine. The examiner assesses side-to-side differences in range of motion and the patient’s willingness to permit the movement. Pain on any movement is significant. The examiner passively takes the patient’s hip through each movement including flexion (normal 110–120°), hip extension (10–15°), internal (30–40°) and external rotation (40–60°) in neutral and with hip flexion, abduction (30–50°) and adduction (30°) and any restrictions are noted.32
Lumbar spine examination
Lumbar spine range of motion is examined with the patient in standing and the examiner sitting behind the patient. The examiner is looking for abnormalities in active range of motion and the patient’s willingness to perform the movement. Pain on any movement is significant. The patient is instructed go through each lumbar range of motion including forward flexion (normal is 40–60°), extension (20–35°), left and right rotation while in extension to elicit any pain, followed by side bending, left and right (15–20°).32
Core stability examination
Testing of core strength is instrumental to overall proper body mechanics. In Akuthota and Nadler’s review of core strengthening in 2004,33 the core is comprised of the diaphragm serving as the roof of the core, the pelvic floor and hip girdle musculature as the floor, the anterior and lateral abdominal musculature including the transversus abdominus and oblique muscles, and the posterior spine stabilizers including the erector spinae and multifidus and gluteals forming the posterior core. The relationship of these muscles is intimate; there is known co-activation of the pelvic floor muscles with transversus abdominus contraction.34 These muscles serve to provide stability to the lumbar spine. In the pregnant state, the growing uterus dictates lengthening of the abdominal musculature, and consequent relative muscle contraction inefficiency. There is an increased demand of the lumbar erector spinae muscles to continually concentrically contract to maintain an erect posture. If the core is weak, this leads to muscle imbalances with compensatory mechanisms which may be contributing to the patient’s pain complaints. Core strength is frequently compromised in the pregnant and postpartum state. Childbirth is directly injurious to the pelvic floor muscles and can create significant transient weakness. Normal pelvic floor muscle strength generally returns within 2 month postpartum.35 Simple tests to evaluation core strength in the pregnant patient include:
ABDOMINAL MUSCULATURE: Assessment of the integrity of the rectus abdominus is important in the pregnant patient. Diastasis is a common physical finding in pregnancy with increasing growth of the gravid uterus. Although this is typically not a pain generator, a defect anteriorly, especially in conjunction with weakness of pelvic floor muscles, can theoretically lead to muscle imbalance and predispose the pregnant patient to lumbar injury (Fig. 123.1).
Pelvis and sacroiliac joint examination
Physical examination focused on detecting aberrant motion of the SIJ is notoriously unreliable. A study by Dreyfuss et al.36 in 1996 evaluated 12 common testing maneuvers for SIJ pain and found that none of the 12 tests was able to reliably detect SIJ dysfunction in 85 patients. However, this study did not include the pregnant population. Another study by Albert et al.37 in 2000 specifically looked at pregnant patients and found that in patients with sacroiliac joint pain three tests had superior sensitivity: the posterior pelvic pain provocation test, Menell’s test, and FABER test, despite reasonable reliability of several other physical examination maneuvers. In 1994, Laslett concluded that five of seven tests were reliable in predicting the sacroiliac joint as a pain source, and that the remaining two tests were potentially reliable.38 In 2003, Young et al. again validated the significant correlation between clinical examination findings with 3 or more pain provocation tests and SIJ pain.39 In 2003, Laslett et al. further showed that the diagnostic accuracy of the physical examination was superior to sacroiliac joint pain provocation test alone for diagnosing symptomatic SIJ.40 Uniform in all of these studies, inter-tester reliability is critical. Practice with these tests and performing them consistently each time will help proper diagnosis of sacroiliac joint dysfunction.
Palpation and mobility testing of the sacroiliac joint
ALIGNMENT: Iliac crest, PSIS, ASIS: With the patient standing, the examiner notes the heights of both iliac crests and each PSIS. The ASIS may be assessed in standing or supine. If the anterior and posterior iliac spines are at the same level, the pelvis is considered to be in proper alignment. If not, the pelvis is misaligned – either anteriorly rotated, posteriorly rotated or sheered superiorly or inferiorly.37
PALPATION OVER THE SIJ: Positive test is if there is sacral sulcus tenderness immediately medial to the posterior superior iliac spine.36 Palpation in this area approximates the sacroiliac joint line.
GILLET’S TEST: The examiner has the patient stand with his or her feet 12 inches apart, while the examiner sits behind the patient and palpates the bilateral posterior superior iliac spines. The patient then flexes the knee and hip on the side to be tested (Fig. 123.2). ‘Stand on one leg and bring the other leg to your chest,’ is often the direction given. The test should show movement of the PSIS inferiorly or a ‘drop’ of the PSIS is seen on the ipsilateral side of the lifted leg. If there is no drop, the test is positive for hypomobility on that side, but is not correlated to the side of pain.36
PALPATION OF PUBIC SYMPHYSIS: With the patient lying supine, the pubic symphysis is palpated gently. If palpation causes pain, that is a positive sign for pubic symphysis tenderness.37
Provocative testing of the sacroiliac joint
FABERS TEST: With the patient lying supine, the patient’s hip is Flexed, ABducted and Externally Rotated so that the heel rests on the opposite kneecap. Pain may be experienced in the inguinal region, which suggests hip joint pathology. Pain may also be experienced in the back or SIJ, suggesting SIJ dysfunction.37 This test is also known as the figure-4 test and Patrick’s maneuver.
FORCED FABER’S TEST: This is another maneuver more specific for SIJ pathology. With the patient in the same position as above, anterior to posterior force is placed on both the externally rotated leg at the knee and on the opposite ASIS (Fig. 123.3). This test is positive with production of pain in the SIJ.32
GAENSLEN’S TEST: With the patient lying supine and on the edge of the examination table, one hip and knee are flexed and held by the patient, while the other hip is extended off the side of the table. Overpressure exerted on the extended knee is applied to force the sacroiliac joint to its end range.38 This test can be performed in the side-lying position with the patient holding the lower leg flexed against the chest while the uppermost leg is extended.32
MENELL’S TEST: With the patient lying supine, one hip is moved into 30° abduction and 10° flexion. It is then first pushed into, then pulled out from the pelvis causing sagittal movement. Pain is considered positive for this test.37
POSTERIOR PELVIC PAIN PROVOCATION TEST (OR AP GLIDE): With the patient lying supine, the hip is flexed to be perpendicular with the table at 90° and the knee is flexed at 90°. A gentle force is applied to the femur in the direction of the examination table, from anterior to posterior (Fig. 123.4). The test is positive when the patient experiences pain in the gluteal region of the tested leg.37,41
ACTIVE STRAIGHT LEG RAISE (ASLR) TEST: This test is performed with the patient supine with both legs extended on the table. The patient raises one leg at a time to 30° of hip flexion without flexing the knee. The test is considered positive when the patient has pain in the back with the leg raised, or describes a heaviness or difficulty in performing the task.42,43 In the second part of the maneuver, posterior compression is applied and the patient is then asked to actively perform a straight leg raise (Fig. 123.5). If there is less pain upon compression or greater ease in motion this is considered a positive provocative test.
COMPRESSION TEST: With the patient supine, pressure is placed on both sides of the pelvis at the ASIS with force applied inward by the palms of the examiner’s hands.38
Pelvic floor and coccyx examination
A vaginal manual examination of the pelvic floor musculature is not recommended in the pregnant patient as this may potentially induce contractions or introduce infection in the region of the cervix. However, rectal examination to evaluate the coccyx and pelvic floor is an option.44 The examination can be done using several techniques reviewed in detail in an article by Maigne.45 Most commonly, the examination is performed with the patient in the side-lying position. A finger is inserted into the rectum and the coccyx can be palpated by gradually pushing the finger posteriorly until contact is made with the coccyx. This technique allows for simultaneous palpation of the pelvic floor because the coccyx is the anatomical insertion for most of these muscles, including the iliococcygeus, pubococcygeus, and coccygeus. Palpation of the coccyx can be performed in this manner and any pain elicited with palpation or mobility is noted. Mobilization of the coccyx using Mennell’s technique46 can be performed by grasping the coccyx between the external thumb and the internal index finger while flexion, extension, and rotation are applied to the coccyx. The intrarectal finger can be used to palpate the pelvic floor musculature.
In the nonpregnant patient, pelvic muscle assessment is done using a one-finger technique both vaginally and rectally. This should be considered, especially in the postpartum patient with persistent pain at the sacral sulci. Pelvic floor muscle tone, strength, conditioning, coordination, tender/trigger points, anatomic deficits such as prolapse, and pelvic descent are evaluated. Tightness, tenderness, and the presence of trigger points are evaluated at the 12, 3, 6, and 9 o’clock positions. By convention, the 12 o’clock position is at the underside of the pubic symphysis and 6 o’clock represents the posterior coccyx. General contractile strength is evaluated, including 10-second isometric holds to evaluate endurance slow-twitch muscle fibers and ‘quick flicks’ to evaluate fast-twitch muscle fibers.47 The obturator internus can also be palpated by internal examination and is activated with hip external rotation. As the patient’s knee presses against the examiner’s external hand, the internal hand can appreciate ipsilateral obturator internus muscle contraction.
DIAGNOSTIC WORK-UP
In 1997, the National Council on Radiation Protection and Measurements (NCRP) evaluated the effects of all types of radiation on reproduction. Many articles were presented which discussed the effects of irradiation on the developing fetus, including congenital malformation, growth retardation, pregnancy loss, and mental retardation.48,49 Although there is argument over the amount of irradiation that would produce such effects, it is generally thought that avoidance of such exposures for the pregnant patient is the rule. However, the failure to correctly diagnose maternal medical problems may pose a much greater risk to the fetus. One paper proposed guidelines for single radiographic image of the abdomen or pelvis with the fetus in field of view as well as estimated fetal dose for CT of the abdomen or pelvis with the fetus in field of view.50 Despite these guidelines, practitioners generally associate exposure to roentgenograms or abdominal CT with high risks to the developing fetus.51
Ultrasound, on the other hand, has been used clinically as an effective diagnostic tool in pregnancy for many years. To date, there is no documented evidence of fetal harm from ultrasound.51 Technological advances have significantly improved, intra-abdominal, intrapelvic and fetal assessments, but because sonography cannot penetrate bone, intra-osseous, epidural, intrathecal and discogenic disease cannot be adequately evaluated. It is limited in its ability to diagnose more sinister etiologies of back or pelvic pain in pregnancy.
Magnetic resonance imaging does not use any ionizing radiation and therefore is thought to be safe for use in the pregnant patient. Until recently, MRI in the pregnant patient was used in the evaluation of adnexal masses, pelvimetry, hydroureteronephrosis of pregnancy, and placenta accreta and to evaluate fetal anomalies such as arachnoid cysts and ventriculomegaly.53 Fast MRI has essentially done away with the need for sedation of the mother and fetus to prevent fetal movement artifact.54 Fast MRI taken during suspension of maternal breathing removes this artifact and results in excellent images with high resolution.55 Gadolinium is not recommended during pregnancy because of its ability to cross the placental barrier and potentially cause harm to the fetus.55 Although MRI appears safe in pregnancy, the International Radiation Protection Association takes the position that MRI should be postponed until after the first trimester and should be limited to cases where unique diagnostic information can be obtained.55 Fast MRI has expanded its usefulness to evaluate and diagnose nonpregnancy-related conditions in the pregnant patient such as lumbar disc herniations and pelvic stress fractures. It can also be used in patients with both posterior and anterior pelvic pain postpartum. One study demonstrated increased T-weighted signal change consistent with edema of the pelvic joints in those with pain.56
SIJ injections have been used as a diagnostic tool for potential sacroiliac joint-mediated pain. There is literature suggesting a low success rate of blindly placing medications intra-articularly within the sacroiliac joints.57 In contrast, there is evidence that medications can be successfully placed within the SIJ using CT guidance58 or fluoroscopic guidance.59 It has been shown that sacroiliac joint injections are clinically effective for the diagnosis and treatment of SIJ syndrome. Because the pregnant population should not undergo fluoroscopy or CT, Pekkafal, in 2003, studied SIJ injections performed under sonographic guidance.60 Of the 60 sonographically guided SIJ injections they performed, 76% were successfully placed intra-articularly and 23% were missed. More importantly, the last 30 injections that were performed had a success rate of 94%, suggesting a significant training effect. Although these were not performed specifically in the pregnant population, the use of ultrasound during pregnancy is known to be safe and the obvious utility of this intervention is important. Future studies should be aimed at the use of ultrasound guided intra-articular SIJ injections for both the diagnosis and treatment of SIJ dysfunction in the pregnant women.
CONCLUSIONS
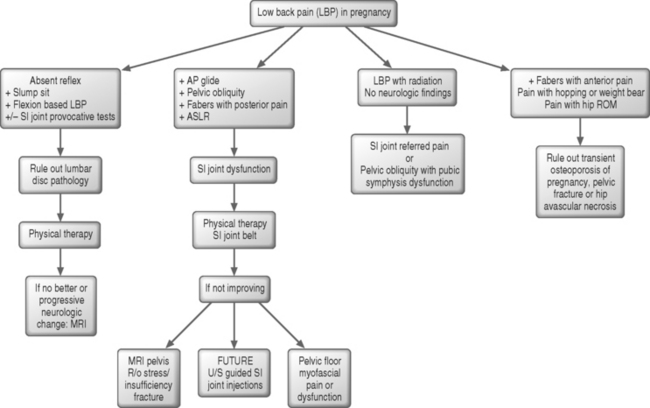
Disabling back pain in the pregnant patient warrants meticulous and detailed physical examination and appropriate diagnostic work-up in light of limited radiographic options. Differential diagnoses include disorders commonly seen in the nonpregnant population with an emphasis on pelvic obliquity and associated SIJ dysfunction. Subsequent therapeutic options are based on comprehensive assessment (Fig. 123.6). Low back pain in pregnancy is manageable and treatable if a proper and timely diagnosis is reached.
1 Johnson D, Coley S. Back pain in pregnancy. J R Soc Med. 1998;91(6):344.
2 Ireland ML, Ott SM. The effects of pregnancy on the musculoskeletal system. Clin Orthop. 2000;372:169-179.
3 Kristiansson P, Svardsudd K, et al. Back pain during pregnancy: a prospective study. Spine. 1996;21(6):702-709.
4 Heckman JD, Sassard R. Musculoskeletal considerations in pregnancy. J Bone Joint Surg [Am]. 1994;76(11):1720-1730.
5 Ritchie JR. Orthopedic considerations during pregnancy. Clin Obstet Gynecol. 2003;46(2):456-466.
6 MacEvilly M, Buggy D. Back pain and pregnancy: a review. Pain. 1996;64(3):405-414.
7 Orvieto R, Achiron A, et al. Low-back pain of pregnancy. Acta Obstet Gynecol Scand. 1994;73(3):209-214.
8 Damen L, Buyruk HM, et al. Pelvic pain during pregnancy is associated with asymmetric laxity of the sacroiliac joints. Acta Obstet Gynecol Scand. 2001;80(11):1019-1024.
9 Damen L, Buyruk HM, et al. The prognostic value of asymmetric laxity of the sacroiliac joints in pregnancy-related pelvic pain. Spine. 2002;27(24):2820-2824.
10 Damen L, Stijnen T, et al. Reliability of sacroiliac joint laxity measurement with Doppler imaging of vibrations. Ultrasound Med Biol. 2002;28(4):407-414.
11 Isascs E, Mark B. Bourdillon’s spinal manipulation, 6th edn. Boston: Butterworth Heinemann, 2002.
12 Sturesson B, Selvik G, et al. Movements of the sacroiliac joints. A roentgen stereophotogrammetric analysis. Spine. 1989;14(2):162-165.
13 Schwarzer AC, Aprill CN, et al. The sacroiliac joint in chronic low back pain. Spine. 1995;20(1):31-37.
14 MacLennan AH. The role of the hormone relaxin in human reproduction and pelvic girdle relaxation. Scand J Rheumatol Suppl. 1991;88:7-15.
15 Ostgaard HC, Andersson GB, et al. Prevalence of back pain in pregnancy. Spine. 1991;16(5):549-552.
15a Friden J. Muscular pain after physical training [Swedish]. Lakartidningen. 1984;81(18):1825-1826.
15b Friden J. Changes in human skeletal muscle induced by long-term eccentric exercise. Cell & Tissue Research. 1984;236(2):365-372.
15c Friden J, Lieber RL. Structural and mechanical basis of exercise-induced muscle injury. Medicine & Science in Sports and Exercise. 1992;24(5):521-530.
16 Maigne JY, Doursounian L, et al. Causes and mechanisms of common coccydynia: role of body mass index and coccygeal trauma. Spine. 2000;25(23):3072-3079.
17 Nattiv A. Stress fractures and bone health in track and field athletes. J Sci Med Sport. 2000;3(3):268-279.
17a Polatti F, Capuzzo E, Viazzo F, et al. Bone mineral changes during and after lactation. Obstet Gynecol. 1999;94(1):52-56.
18 Thienpont E, Simon JP, et al. Sacral stress fracture during pregnancy – a case report. Acta Orthop Scand. 1999;70(5):525-526.
19 Rousiere M, Kahan A, et al. Postpartal sacral fracture without osteoporosis. Joint Bone Spine. 2001;68(1):71-73.
19a Parrish KM, Holt VL, Easterling TR, et al. Effect of changes in maternal age, parity, and birth weight distribution on primary cesarean delivery rates. JAMA. 1994;271(6):443-447.
20 Bjorklund K, Bergstrom S, et al. Symphyseal distention in relation to serum relaxin levels and pelvic pain in pregnancy. Acta Obstet Gynecol Scand. 2000;79(4):269-275.
21 Schoellner C, Szoke N, et al. [Pregnancy-associated symphysis damage from the orthopedic viewpoint – studies of changes of the pubic symphysis in pregnancy, labor and post partum]. Z Orthop Ihre Grenzgeb. 2001;139(5):458-462.
22 Lentz SS. Osteitis pubis: a review. Obstet Gynecol Surv. 1995;50(4):310-315.
23 Wiltse LL, Frantz CH. Non-suppurative osteitis pubis in the female. J Bone Joint Surg [Am]. 1956;38A(3):500-516.
24 LaBan MM, Perrin JC, et al. Pregnancy and the herniated lumbar disc. Arch Phys Med Rehabil. 1983;64(7):319-321.
24a Schmid L, Pfirrman C, Hess T, et al. Bilateral fracture of the sacrum associated with pregnancy: a case report Osteoporosis International. 1999;101(1):91-93.
25 Kirkaldy-Willis WH, Wedge JH, et al. Pathology and pathogenesis of lumbar spondylosis and stenosis. Spine. 1978;3(4):319-328.
26 Aminoff MJ. Neurological disorders and pregnancy. Am J Obstet Gynecol. 1978;132(3):325-335.
27 Wong CA, Scavone BM, et al. Incidence of postpartum lumbosacral spine and lower extremity nerve injuries. Obstet Gynecol. 2003;101(2):279-288.
28 Cheng N, Burssens A, et al. Pregnancy and post-pregnancy avascular necrosis of the femoral head. Arch Orthop Trauma Surg. 1982;100(3):199-210.
29 Beaulieu JG, Razzano CD, et al. Transient osteoporosis of the hip in pregnancy. Clin Orthop. 1976;115:165-168.
30 Saraste H. Spondylolysis and pregnancy – a risk analysis. Acta Obstet Gynecol Scand. 1986;65(7):727-729.
31 Sanderson PL, Fraser RD. The influence of pregnancy on the development of degenerative spondylolisthesis. J Bone Joint Surg [Br]. 1996;78(6):951-954.
32 Magee D. Orthopedic physical assessment. Philadelphia, PE: WB Saunders, 2002.
33 Akuthota V, Nadler SF. Core strengthening. Arch Phys Med Rehabil. 2004;85(3 Suppl 1):S86-S92.
34 Sapsford RR, Hodges PW, et al. Co-activation of the abdominal and pelvic floor muscles during voluntary exercises. Neurourol Urodyn. 2001;20(1):31-42.
35 Peschers UM, Schaer GN, et al. Levator ani function before and after childbirth. Br J Obstet Gynaecol. 1997;104(9):1004-1008.
36 Dreyfuss P, Michaelsen M, et al. The value of medical history and physical examination in diagnosing sacroiliac joint pain. Spine. 1996;21(22):2594-2602.
37 Albert H, Godskesen M, et al. Evaluation of clinical tests used in classification procedures in pregnancy-related pelvic joint pain. Eur Spine J. 2000;9(2):161-166.
38 Laslett M, Williams M. The reliability of selected pain provocation tests for sacroiliac joint pathology. Spine. 1994;19(11):1243-1249.
39 Young S, Aprill C, et al. Correlation of clinical examination characteristics with three sources of chronic low back pain. Spine J. 2003;3(6):460-465.
40 Laslett M, Young SB, et al. Diagnosing painful sacroiliac joints: A validity study of a McKenzie evaluation and sacroiliac provocation tests. Aust J Physiother. 2003;49(2):89-97.
41 Ostgaard HC, Zetherstrom G, et al. The posterior pelvic pain provocation test in pregnant women. Eur Spine J. 1994;3(5):258-260.
42 Mens JM, Vleeming A, et al. The active straight leg raising test and mobility of the pelvic joints. Eur Spine J. 1999;8(6):468-473.
43 Mens JM, Vleeming A, et al. Validity of the active straight leg raise test for measuring disease severity in patients with posterior pelvic pain after pregnancy. Spine. 2002;27(2):196-200.
44 Thiele G. Coccydynia and pain in the superior gluteal region. JAMA. 1937;109:1271-1275.
45 Maigne JY, Chatellier G. Comparison of three manual coccydynia treatments: a pilot study. Spine. 2001;26(20):E479-E483. discussion E484
46 Mennell J. The science and art of joint manipulation. London: Churchill, 1952.
47 Theofrastous JP, Swift SE. The clinical evaluation of pelvic floor dysfunction. Obstet Gynecol Clin North Am. 1998;25(4):783-804.
48 Brent RL. Utilization of developmental basic science principles in the evaluation of reproductive risks from pre- and postconception environmental radiation exposures. Teratology. 1999;59(4):182-204.
49 Schull WJ, Otake M. Cognitive function and prenatal exposure to ionizing radiation. Teratology. 1999;59(4):222-226.
50 El-Khoury GY, Madsen MT, et al. A new pregnancy policy for a new era. Am J Roentgenol. 2003;181(2):335-340.
51 Ratnapalan S, Bona N, et al. Physicians’ perceptions of teratogenic risk associated with radiography and CT during early pregnancy. Am J Roentgenol. 2004;182(5):1107-1109.
52 Ziskin MC. Intrauterine effects of ultrasound: human epidemiology. Teratology. 1999;59(4):252-260.
53 Levine D, Barnes PD, et al. Obstetric MR imaging. Radiology. 1999;211(3):609-617.
54 Nagayama M, Watanabe Y, et al. Fast MR imaging in obstetrics. Radiographics. 2002;22(3):563-580. discussion 580–582
55 Amin RS, Nikolaidis P, et al. Normal anatomy of the fetus at MR imaging. Radiographics. 1999;19(Spec No):S201-S214.
56 Wurdinger S, Humbsch K, et al. MRI of the pelvic ring joints postpartum: normal and pathological findings. J Magn Reson Imaging. 2002;15(3):324-329.
57 Rosenberg JM, Quint TJ, et al. Computerized tomographic localization of clinically guided sacroiliac joint injections. Clin J Pain. 2000;16(1):18-21.
58 Pulisetti D, Ebraheim NA. CT-guided sacroiliac joint injections. J Spinal Disord. 1999;12(4):310-312.
59 Slipman CW, Lipetz JS, et al. Fluoroscopically guided therapeutic sacroiliac joint injections for sacroiliac joint syndrome. Am J Phys Med Rehabil. 2001;80(6):425-432.
60 Pekkafahli MZ, Kiralp MZ, et al. Sacroiliac joint injections performed with sonographic guidance. J Ultrasound Med. 2003;22(6):553-559.