CHAPTER 21 Long-Term Patellofemoral Progression
 The natural history of the patellofemoral articulation after unicompartmental arthroplasty is poorly understood, and the majority of unicompartmental literature fails to adequately address and describe patellofemoral progression.
The natural history of the patellofemoral articulation after unicompartmental arthroplasty is poorly understood, and the majority of unicompartmental literature fails to adequately address and describe patellofemoral progression. The preoperative status of the patellofemoral articulation does not appear to affect the early to midterm results of Oxford mobile-bearing unicompartmental arthroplasty.
The preoperative status of the patellofemoral articulation does not appear to affect the early to midterm results of Oxford mobile-bearing unicompartmental arthroplasty. The rate of long-term radiographic progression of patellofemoral degeneration is as high as 65%, but the majority of progression is low grade and rarely requires revision.
The rate of long-term radiographic progression of patellofemoral degeneration is as high as 65%, but the majority of progression is low grade and rarely requires revision.Introduction
Long-term survivorship of unicompartmental knee arthroplasty (UKA) is predicated on preoperative patient selection, obtaining proper limb alignment while avoiding overcorrection, and appropriate component position and sizing. An aspect of implant survivorship that is poorly understood is the natural history of arthritis progression in the adjacent tibiofemoral and/or patellofemoral compartments. However, one of the most common reasons cited for UKA failure is pain in one or more of the un-resurfaced compartments.1 The incidence and sequelae of patellofemoral compartment degeneration following UKA has been incompletely delineated. The purpose of this chapter is to summarize the natural history of patellofemoral compartment degeneration, and to describe the contribution of this degeneration to the long-term survival of UKA.
Preexisting Patellofemoral Arthrosis
The contribution of preexisting radiographic patellofemoral arthrosis and/or anterior knee pain to the survivorship of UKA has been described, yet remains a source of debate. Intuitively, preexisting patellofemoral arthritis and/or anterior knee pain should compromise the results of UKA, and many authors consider either of these findings to be contraindications to UKA.2,3 However, several studies have contradicted this assumption. In one short-term study, Beard et al.4 performed an intraoperative evaluation of the patellofemoral articulation in 824 medial UKAs using the Oxford (Biomet; Bridgend, United Kingdom) prosthesis. They noted full-thickness trochlear or patellar cartilage loss in 128 knees (13%). With minimum 1-year follow-up, the knees with cartilage loss did not have significantly worse Oxford scores or Knee Society scores, although patients with full-thickness patellar loss did have significantly worse Knee Society Functional Scores. Additionally, increasing severity of patellofemoral degeneration did not worsen the outcome. In another prospective study, Beard et al.5 evaluated the outcomes of 100 UKAs (Oxford, Biomet). Although 54% of knees had preoperative anterior knee pain and 54% had preoperative radiographic patellofemoral degeneration (including 10% with joint space obliteration), these knees had outcomes similar to the 46% without preoperative pain or degeneration. Knees with lateral patellofemoral degeneration faired slightly worse than knees with medial patellofemoral degeneration, but each of these groups still had good overall outcomes. The authors concluded that neither medial patellofemoral joint degeneration nor anterior knee pain should be considered a contraindication to Oxford UKA. Kuipers et al.6 also assessed the effect of preoperative patellofemoral joint involvement and reported on 437 Oxford UKAs evaluated at a mean of 2.6 years (range, 0.1–7.9 years). The authors found that preoperative patellofemoral osteoarthritis was not associated with decreased implant survival. In fact, they noted a paradoxical 70% reduction in revision risk for patients with preoperative patellofemoral osteoarthritis.
The longer term results of preexisting patellofemoral degeneration on the outcomes of UKA are less clear. There are several longer term outcome studies in which patellofemoral degeneration was not considered to be an absolute contraindication to UKA.7–15 Most of these failed to demonstrate significant differences in failure rates among those patients with and without preexisting patellofemoral arthrosis. However, Argenson et al.8 studied 160 UKAs (Miller-Galante; Zimmer, Warsaw, IN) for a mean of 5.5 years (range, 3–9.3 years) and found that two of their five revisions were secondary to patellofemoral arthritis. These authors noted that both of the revisions for patellofemoral arthritis also had preexisting patellofemoral degeneration. As a result of their findings, the authors now consider extensive loss of cartilage in the patellofemoral joint found on preoperative radiograph or intraoperative inspection to be a contraindication to UKA.
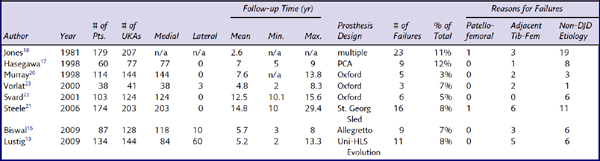
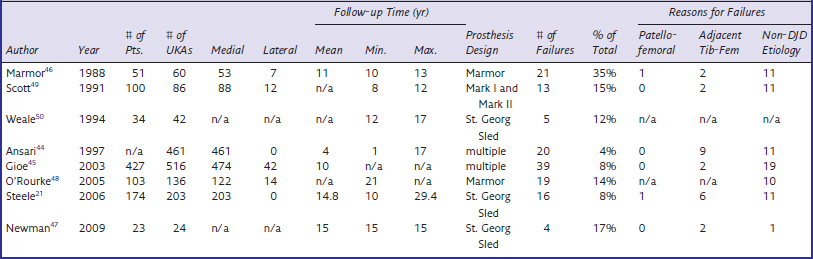
A substantial number of studies include patients with patellofemoral arthrosis as part of the inclusion criteria for UKA, but fail to mention the status of the patellofemoral joint clinically or radiographically at follow-up.16–23 These are shown in Table 21–1. Svard and Price,22 for example, reported the long-term results of 124 medial UKAs using the Oxford mobile-bearing prosthesis. In their cohort, “the state of the patellofemoral compartment was not used as a criterion for selection and no patient was rejected because of patellofemoral degeneration.” Six knees (4.8%) were revised for reasons unrelated to the patellofemoral compartment. However, there was no mention that the patellofemoral compartment was included as part of the follow-up evaluation. In the majority of these studies (see Table 21–1), there were no failures that were secondary to patellofemoral arthritis, and in two studies, only one failure was due to patellofemoral complications. It is therefore tempting to conclude that the inclusion of preoperative patellofemoral degeneration does not negatively affect outcomes. However, in each of these studies, there is no clear indication that the clinical or radiographic status of the patellofemoral joint was evaluated as one of the outcome measures. It may be that there truly were no complications attributable to the patellofemoral joint. Alternatively, it is possible that the authors were not looking for patellofemoral complications, given a bias that the patellofemoral joint is not a relevant source of pain in these patients. Therefore, we are guarded with respect to our interpretation of these reports and believe that meaningful conclusions regarding the extent to which preoperative patellofemoral involvement affects UKA longevity cannot be drawn based on these studies.
Long-Term Patellofemoral Arthritic Progression
We reviewed the literature for UKA outcome studies, with a specific emphasis on reports with long-term follow-up. Although there were several studies that specifically address patellofemoral complications following UKA, a surprising number of studies did not specifically include the status of the patellofemoral joint as part of their clinical and/or radiographic follow-up criteria.11,17,22–43 In these studies, it is difficult to conclude whether patellofemoral degeneration was simply not a source of clinical complication, or whether the patellofemoral joint actually impacted the results of UKA but was overlooked in the study design. As such, meaningful conclusions regarding the natural history of the patellofemoral articulation following UKA cannot be drawn from these studies.
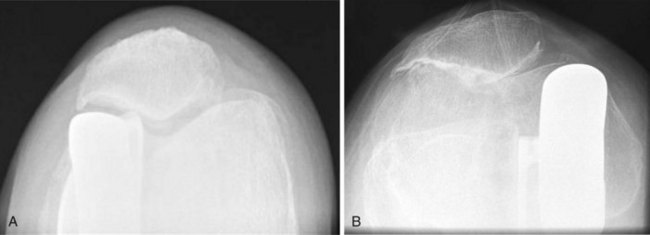
Table 21–2 lists another large subset of studies in which it is difficult to draw conclusions regarding the fate of the patellofemoral joint following UKA.21,44–50 In each of these outcome studies, the authors indicated that failures occurred secondary to “progression of disease” but, unfortunately, failed to differentiate if that progression occurred in the un-resurfaced tibiofemoral compartment or in the patellofemoral compartment (Fig. 21–1). Steele et al.21 reported on 203 medial UKAs (St. Georg Sled; Waldemar-Link, Hamburg, Germany) with a mean follow-up of 14.8 years (range, 10–29.4 years). The most common reason for failure in this cohort was “progression in another compartment.” Seven of 16 failures were secondary to progression. At least one revision was required because of progression of disease in both the lateral and patellofemoral compartments, but the authors did not specify the location of progression of the other six failures. O’Rourke et al.48 described the minimum 21-year results of 136 UKAs (Marmor; Richards Orthopaedics, Memphis, TN). In this series, the overall revision rate was 14.9% (19 knees) and the majority of revisions (9 knees) were secondary to “disease progression.” Again, the location of progression was not explicitly stated. The authors did, however, report that 75 knees (59%) had radiographic patellofemoral arthritis and 66 knees (52%) had contralateral tibiofemoral progression. Although progression occurred in both compartments, it is unclear if the progressions that lead to failure occurred in the tibiofemoral compartment, patellofemoral compartment, or both. Similarly, Gioe et al.45 reported on the 5- and 10-year survivorship of 516 UKAs (474 medial, 42 lateral) using prostheses from multiple manufacturers. A total of 39 failures were identified. The most common reason for revision was “progression of arthritis in the uninvolved compartments,” which accounted for 51.3% of the failures. Again, the location of the progression was not delineated. Thus, once again, the fate of the patellofemoral compartment is inconclusive based on these reports.
Table 21–2 Long-Term Studies Demonstrating Radiographic Evidence of Adjacent Compartment Degeneration, but without Delineation of Tibiofemoral or Patellofemoral Compartment Progression
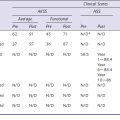
Fortunately, a subset of studies have evaluated the clinical and radiographic progression of disease specifically in the patellofemoral compartment7-15,51-66 (Table 21–3). These studies had follow-up ranging from an average of 2 years to 14.9 years and included both medial and lateral UKAs using a variety of implants. Although the all-cause failure rate ranged from 0% to 30%, in general very few failures were secondary to patellofemoral progression. In fact, in nearly two thirds of these studies the majority of failures were related to causes other than progression of disease (in either compartment). Price et al.14 followed 114 medial UKAs (Oxford) for a minimum of 10 years and found that 16 of 23 failures were unrelated to disease progression and the other 7 failures were due to progression in the lateral compartment. Hernigou and Deschamps55 reported 22 total failures out of 99 UKAs (Lotus; Howmedica, Benoist Girard, Herouville Saint Clair, France), of which 18 failed secondary to etiologies unrelated to progression, 3 failed from progression in the adjacent tibiofemoral compartment, and 1 failed from progression in the patellofemoral compartment. Overall, when failure was due to disease progression, it most commonly occurred in the un-resurfaced tibiofemoral compartment.
Table 21–3 All Studies That Specifically Evaluate the Status of the Patellofemoral Joint at Follow-up (List Includes Studies That Did Not Grade the Severity of Disease Progression)
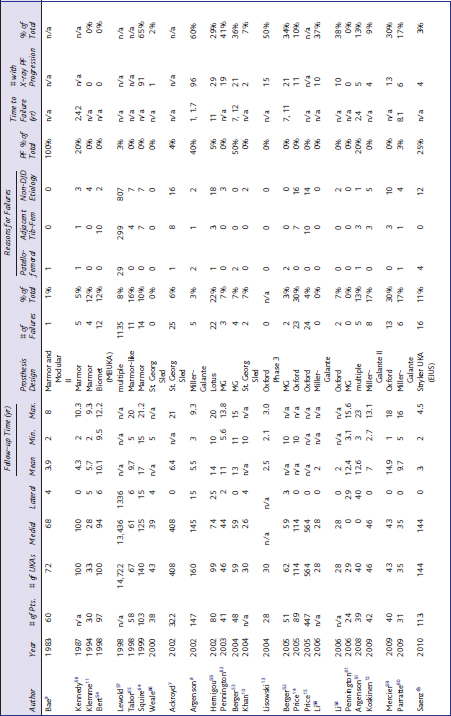
When the studies in Table 21–3 are taken in summation, revision for progression in the adjacent tibiofemoral compartment was nearly eight times more common than revision for patellofemoral progression (there were 360 revisions for tibiofemoral progression versus 45 revisions for patellofemoral progression). No revisions were performed for patellofemoral progression in any of the knees that received the Oxford mobile-bearing prosthesis despite the fact that all four of the studies that involved the Oxford UKA reported radiographic patellofemoral progression ranging from 10% to 50% of knees. It is also interesting to note that two of these four studies included patients with preoperative radiographic patellofemoral osteoarthritic changes. In contradistinction, 9 of 20 studies involving fixed-bearing devices (excluding studies that included both fixed- and mobile-bearing designs) reported knees that required revision for patellofemoral progression. All but five of these studies excluded knees with preoperative patellofemoral degeneration. Berger et al.53 followed 59 medial UKAs (Miller-Galante) for a mean of 13 years (range, 11–15 years) and noted that the only two revisions in the cohort had failed secondary to progressive patellofemoral degeneration (7 and 12 years). Two additional patients had moderate or severe patellofemoral symptoms. Interestingly, at 10 years only 1.6% of patients had patellofemoral symptoms, but this increased to 10% at 15 years. Saenz et al.63 followed 144 medial UKAs (EIUS UKA; Stryker, Mahwah, NJ). Although they had a short average follow-up of only 3 years (range, 2–4.5 years), there were four knees with patellofemoral degeneration that required revision. No knees required revision for adjacent tibiofemoral progression, and 12 required revision for reasons unrelated to progression. The reason for early patellofemoral failure in this cohort is unclear, but it is a noticeable outlier. Preoperatively, the authors excluded patients with any anterior knee pain, but did not specifically note if preoperative radiographic degeneration was accepted.
As seen in Table 21–3, although the overall failure rate secondary to patellofemoral progression was low, the incidence of radiographic progression was notably higher, ranging from 0% to 65%. It is notable that five of the studies quantified the percentage of knees with radiographic patellofemoral progression, but did not grade the severity of the progression. Three of these five studies report progression greater than or equal to 50% (50%, 60%, and 65%), which represents the highest incidences reported. Because progression can range from simple osteophytes to full-thickness changes, the clinical significance of these ungraded changes is uncertain (Fig. 21–2). Furthermore, despite the high rate of radiographic progression, revision for patellofemoral progression was reported in only one of these studies (two knees).8
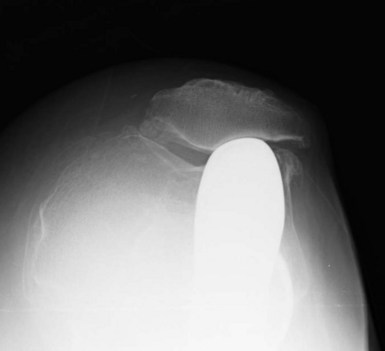
In the studies that did grade the radiographic patellofemoral progression, the grade was typically low. For example, although Pennington et al.62 reported progression in 19 of 46 knees (41%), all were classified as Berger grade I (osteophytes only). Similarly, Argenson et al.51 reported progression in 5 of 40 knees (13%) and all of these were Ahlbäck grade I changes (joint space narrowing < 3 mm). Hernigou and Deschamps55 performed a thorough radiographic analysis on 99 UKAs with a mean follow-up of 14 years (range, 10–20 years). In addition to the 29 knees (29%) that developed patellofemoral osteoarthritis, 28 knees had impingement of the femoral component on the patella. They found that impingement occurred with an oversized or anteriorly placed femoral component. Impingement led to patellar notching and erosion, and was associated with a higher incidence of patellofemoral symptoms than knees with patellofemoral osteoarthritis without impingement (Fig. 21–3). One knee (1%) required revision because of patellar impingement. In the series by Berger et al.,52 all four knees with grade 4 patellofemoral changes had associated patellar impingement.
1 Borus T, Thornhill T. Unicompartmental knee arthroplasty. J Am Acad Orthop Surg. 2008;16:9-18.
2 Kozinn SC, Scott R. Unicondylar knee arthroplasty. J Bone Joint Surg [Am]. 1989;71:145-150.
3 Stern SH, Becker MW, Insall JN. Unicondylar knee arthroplasty: an evaluation of selection criteria. Clin Orthop Relat Res. 1993;286:143-148.
4 Beard DJ, Pandit H, Gill HS, et al. The influence of the presence and severity of pre-existing patellofemoral degenerative changes on the outcome of the Oxford medial unicompartmental knee replacement. J Bone Joint Surg [Br]. 2007;89:1597-1601.
5 Beard DJ, Pandit H, Ostlere S, et al. Pre-operative clinical and radiological assessment of the patellofemoral joint in unicompartmental knee replacement and its influence on outcome. J Bone Joint Surg [Br]. 2007;89:1602-1607.
6 Kuipers BM, Kollen BJ, Bots PC, et al. Factors associated with reduced early survival in the Oxford phase III medial unicompartment knee replacement. Knee. 2010;17:48-52.
7 Ackroyd CE, Whitehouse SL, Newman JH, Joslin CC. A comparative study of the medial St Georg sled and kinematic total knee arthroplasties: ten-year survivorship. J Bone Joint Surg [Br]. 2002;84:667-672.
8 Argenson JN, Chevrol-Benkeddache Y, Aubaniac JM. Modern unicompartmental knee arthroplasty with cement: a three to ten-year follow-up study. J Bone Joint Surg [Am]. 2002;84:2235-2239.
9 Bae DK, Guhl JF, Keane SP. Unicompartmental knee arthroplasty for single compartment disease: clinical experience with an average four-year follow-up study. Clin Orthop Relat Res. 1983;176:233-238.
10 Khan OH, Davies H, Newman JH, Weale AE. Radiological changes ten years after St. Georg Sled unicompartmental knee replacement. Knee. 2004;11:403-407.
11 Klemme WR, Galvin EG, Petersen SA. Unicompartmental knee arthroplasty: sequential radiographic and scintigraphic imaging with an average five-year follow-up. Clin Orthop Relat Res. 1994;301:233-238.
12 Koskinen E, Paavolainen P, Eskelinen A, et al. Medial unicompartmental knee arthroplasty with Miller-Galante II prosthesis: mid-term clinical and radiographic results. Arch Orthop Trauma Surg. 2009;129:617-624.
13 Lisowski LA, Verheijen PM, Lisowski AE. Oxford Phase 3 unicompartmental knee arthroplasty (UKA): clinical and radiological results of minimum follow-up of 2 years. Orthop Traumatol Rehabil. 2004;6:773-776.
14 Price AJ, Dodd CA, Svard UG, Murray DW. Oxford medial unicompartmental knee arthroplasty in patients younger and older than 60 years of age. J Bone Joint Surg [Br]. 2005;87:1488-1492.
15 Price AJ, Waite JC, Svard U. Long-term clinical results of the medial Oxford unicompartmental knee arthroplasty. Clin Orthop Relat Res. 2005;435:171-180.
16 Biswal S, Brighton RW. Results of unicompartmental knee arthroplasty with cemented, fixed-bearing prosthesis using minimally invasive surgery. J Arthroplasty. 2010;25:721-727.
17 Hasegawa Y, Ooishi Y, Shimizu T, et al. Unicompartmental knee arthroplasty for medial gonarthrosis: 5 to 9 years follow-up evaluation of 77 knees. Arch Orthop Trauma Surg. 1998;117:183-187.
18 Jones WT, Bryan RS, Peterson LF, Ilstrup DM. Unicompartmental knee arthroplasty using polycentric and geometric hemicomponents. J Bone Joint Surg [Am]. 1981;63:946-954.
19 Lustig S, Paillot JL, Servien E, et al. [Cemented all polyethylene tibial insert unicompartimental knee arthroplasty: a long term follow-up study]. Orthop Traumatol Surg Res. 2009;95:12-21.
20 Murray DW, Goodfellow JW, O’Connor JJ. The Oxford medial unicompartmental arthroplasty: a ten-year survival study. J Bone Joint Surg [Br]. 1998;80:983-989.
21 Steele RG, Hutabarat S, Evans RL, et al. Survivorship of the St Georg Sled medial unicompartmental knee replacement beyond ten years. J Bone Joint Surg [Br]. 2006;88:1164-1168.
22 Svard UC, Price AJ. Oxford medial unicompartmental knee arthroplasty: a survival analysis of an independent series. J Bone Joint Surg [Br]. 2001;83:191-194.
23 Vorlat P, Verdonk R, Schauvlieghe H. The Oxford unicompartmental knee prosthesis: a 5-year follow-up. Knee Surg Sports Traumatol Arthrosc. 2000;8:154-158.
24 Aleto TJ, Berend ME, Ritter MA, et al. Early failure of unicompartmental knee arthroplasty leading to revision. J Arthroplasty. 2008;23:159-163.
25 Ashraf T, Newman JH, Evans RL, Ackroyd CE. Lateral unicompartmental knee replacement survivorship and clinical experience over 21 years. J Bone Joint Surg [Br]. 2002;84:1126-1130.
26 Bergenudd H. Porous-coated anatomic unicompartmental knee arthroplasty in osteoarthritis: a 3- to 9-year follow-up study. J Arthroplasty. 1995;10(Suppl):S8-S13.
27 Carr A, Keyes G, Miller R, et al. Medial unicompartmental arthroplasty: a survival study of the Oxford meniscal knee. Clin Orthop Relat Res. 1993;295:205-213.
28 Cartier P, Sanouiller JL, Grelsamer RP. Unicompartmental knee arthroplasty surgery: 10-year minimum follow-up period. J Arthroplasty. 1996;11:782-788.
29 Christensen NO. Unicompartmental prosthesis for gonarthrosis: a nine-year series of 575 knees from a Swedish hospital. Clin Orthop Relat Res. 1991;273:165-169.
30 Fehring TK, Odum SM, Masonis JL, Springer BD. Early failures in unicondylar arthroplasty. Orthopedics. 2010;33:11.
31 Gulati A, Chau R, Simpson DJ, et al. Influence of component alignment on outcome for unicompartmental knee replacement. Knee. 2009;16:196-199.
32 Hamilton WG, Collier MB, Tarabee E, et al. Incidence and reasons for reoperation after minimally invasive unicompartmental knee arthroplasty. J Arthroplasty. 2006;21(6 Suppl 2):98-107.
33 Heck DA, Marmor L, Gibson A, Rougraff BT. Unicompartmental knee arthroplasty. A multicenter investigation with long-term follow-up evaluation. Clin Orthop Relat Res. 1993;286:154-159.
34 Hernigou P, Deschamps G. Alignment influences wear in the knee after medial unicompartmental arthroplasty. Clin Orthop Relat Res. 2004;423:161-165.
35 Jeer PJ, Keene GC, Gill P. Unicompartmental knee arthroplasty: an intermediate report of survivorship after the introduction of a new system with analysis of failures. Knee. 2004;11:369-374.
36 Kort NP, van Raay JJ, Cheung J, et al. Analysis of Oxford medial unicompartmental knee replacement using the minimally invasive technique in patients aged 60 and above: an independent prospective series. Knee Surg Sports Traumatol Arthrosc. 2007;15:1331-1334.
37 Koskinen E, Paavolainen P, Eskelinen A, et al. Unicondylar knee replacement for primary osteoarthritis: a prospective follow-up study of 1,819 patients from the Finnish Arthroplasty Register. Acta Orthop. 2007;78:128-135.
38 Newman JH, Ackroyd CE, Shah NA. Unicompartmental or total knee replacement? Five-year results of a prospective, randomised trial of 102 osteoarthritic knees with unicompartmental arthritis. J Bone Joint Surg [Br]. 1998;80:862-865.
39 Robertsson O, Lidgren L. The short-term results of 3 common UKA implants during different periods in Sweden. J Arthroplasty. 2008;23:801-807.
40 Schai PA, Suh JT, Thornhill TS, Scott RD. Unicompartmental knee arthroplasty in middle-aged patients: a 2- to 6-year follow-up evaluation. J Arthroplasty. 1998;13:365-372.
41 Swank M, Stulberg SD, Jiganti J, Machairas S. The natural history of unicompartmental arthroplasty: an eight-year follow-up study with survivorship analysis. Clin Orthop Relat Res. 1993;286:130-142.
42 Walton MJ, Weale AE, Newman JH. The progression of arthritis following lateral unicompartmental knee replacement. Knee. 2006;13:374-377.
43 Whittaker JP, Naudie DD, McAuley JP, et al. Does bearing design influence midterm survivorship of unicompartmental arthroplasty? Clin Orthop Relat Res. 2010;468:73-81.
44 Ansari S, Newman JH, Ackroyd CE.St. Georg sledge for medial compartment knee replacement: 461 arthroplasties followed for 4 (1–17) years. Acta Orthop Scand. 1997;68:430-434.
45 Gioe TJ, Killeen KK, Hoeffel DP, et al. Analysis of unicompartmental knee arthroplasty in a community-based implant registry. Clin Orthop Relat Res. 2003;416:111-119.
46 Marmor L. Unicompartmental arthroplasty of the knee with a minimum ten-year follow-up period. Clin Orthop Relat Res. 1988;228:171-177.
47 Newman J, Pydisetty RV, Ackroyd C. Unicompartmental or total knee replacement: the 15-year results of a prospective randomised controlled trial. J Bone Joint Surg [Br]. 2009;91:52-57.
48 O’Rourke MR, Gardner JJ, Callaghan JJ, et al. The John Insall Award. Unicompartmental knee replacement: a minimum twenty-one-year followup, end-result study. Clin Orthop Relat Res. 2005;440:27-37.
49 Scott RD, Cobb AG, McQueary FG, Thornhill TS. Unicompartmental knee arthroplasty: eight- to 12-year follow-up evaluation with survivorship analysis. Clin Orthop Relat Res. 1991;271:96-100.
50 Weale AE, Newman JH. Unicompartmental arthroplasty and high tibial osteotomy for osteoarthrosis of the knee: a comparative study with a 12- to 17-year follow-up period. Clin Orthop Relat Res. 1994;302:134-137.
51 Argenson JN, Parratte S, Bertani A, et al. Long-term results with a lateral unicondylar replacement. Clin Orthop Relat Res. 2008;466:2686-2693.
52 Berger RA, Meneghini RM, Jacobs JJ, et al. Results of unicompartmental knee arthroplasty at a minimum of ten years of follow-up. J Bone Joint Surg [Am]. 2005;87:999-1006.
53 Berger RA, Meneghini RM, Sheinkop MB, et al. The progression of patellofemoral arthrosis after medial unicompartmental replacement: results at 11 to 15 years. Clin Orthop Relat Res. 2004;428:92-99.
54 Bert JM. 10-year survivorship of metal-backed, unicompartmental arthroplasty. J Arthroplasty. 1998;13:901-905.
55 Hernigou P, Deschamps G. Patellar impingement following unicompartmental arthroplasty. J Bone Joint Surg [Am]. 2002;84:1132-1137.
56 Kennedy WR, White RP. Unicompartmental arthroplasty of the knee: postoperative alignment and its influence on overall results. Clin Orthop Relat Res. 1987;221:278-285.
57 Lewold S, Robertsson O, Knutson K, Lidgren L. Revision of unicompartmental knee arthroplasty: outcome in 1,135 cases from the Swedish Knee Arthroplasty study. Acta Orthop Scand. 1998;69:469-474.
58 Li MG, Yao F, Joss B, et al. Mobile vs. fixed bearing unicondylar knee arthroplasty: a randomized study on short term clinical outcomes and knee kinematics. Knee. 2006;13:365-370.
59 Mercier N, Wimsey S, Saragaglia D. Long-term clinical results of the Oxford medial unicompartmental knee arthroplasty. Int Orthop. 2010;34:1137-1143.
60 Parratte S, Argenson JN, Pearce O, et al. Medial unicompartmental knee replacement in the under-50s. J Bone Joint Surg [Br]. 2009;91:351-356.
61 Pennington DW, Swienckowski JJ, Lutes WB, Drake GN. Lateral unicompartmental knee arthroplasty: survivorship and technical considerations at an average follow-up of 12.4 years. J Arthroplasty. 2006;21:13-17.
62 Pennington DW, Swienckowski JJ, Lutes WB, Drake GN. Unicompartmental knee arthroplasty in patients sixty years of age or younger. J Bone Joint Surg [Am]. 2003;85:1968-1973.
63 Saenz CL, McGrath MS, Marker DR, et al. Early failure of a unicompartmental knee arthroplasty design with an all-polyethylene tibial component. Knee. 2010;17:53-56.
64 Squire MW, Callaghan JJ, Goetz DD, et al. Unicompartmental knee replacement: a minimum 15 year followup study. Clin Orthop Relat Res. 1999;367:61-72.
65 Tabor OBJr, Tabor OB. Unicompartmental arthroplasty: a long-term follow-up study. J Arthroplasty. 1998;13:373-379.
66 Weale AE, Murray DW, Baines J, Newman JH. Radiological changes five years after unicompartmental knee replacement. J Bone Joint Surg [Br]. 2000;82:996-1000.
* The authors have not received any financial support for the work and have no other financial or personal connections to the work presented in this manuscript. Dr. Foran is on the governing/editorial board of an AAOS publication. Dr. Della Valle performs consulting services for Angiotech, Smith and Nephew, Biomet, and Kinamed and has received research support from Zimmer.