Long Face Growth Patterns
Maxillary Vertical Excess with Mandibular Deformity
• The Role of Growth Modification in the Preadolescent Patient
• The Orthodontic Camouflage Approach
• An Orthodontic Molar Intrusion Approach
• Postsurgical Orthodontic Maintenance and Detailing
• Complications, Informed Consent, and Patient Education
• Malocclusion after Orthodontics and Orthognathic Surgery
• Temporomandibular Disorders: Effects of Orthodontics and Orthognathic Surgery
The prevalence of a long face growth pattern at a prominent U.S. maxillofacial center was documented as representing 22% of jaw deformity evaluations as judged from the parameter of excessive anterior facial height.114 The lower anterior facial height was specifically long in 88% of the affected individuals.54,74,75 The term long face is generally used to describe a maxillofacial growth pattern that typically also includes a gummy smile, an anterior open bite, and a lack of chin prominence. This combination of problems seems to be harder for the individual to live with; it results in a personal and family decision to seek treatment more frequently than most other patterns of dentofacial deformity (e.g., mandibular deficiency alone).112 Halfway around the world, in South Africa, Reyneke estimated that, in his orthognathic practice, approximately 30% of those seeking treatment have a long face with complaints about a gummy smile and concerns caused by malocclusion.117
The basic diagnostic criteria for a long face growth pattern include an excessive anterior facial height (i.e., the elongation of the lower third) that leads to disproportion between facial height and width.26,28,69,70 Studies confirm that the excessive eruption of the posterior maxillary dentition causes the mandible to rotate downward and backward (clockwise rotation) and results in increased lower facial height.24,34 This makes any baseline mandibular anteroposterior deficiency seem worse and any true mandibular prognathism seem better.31,123 As the mandible rotates down and back during facial development, the lower incisors often adapt by becoming more upright, with crowding. The mandibular clockwise rotation tends to separate the upper and lower incisors vertically, thereby creating an open bite with an accentuated curve of Spee.76 Not all long face growth patterns involve an anterior open bite. The maxillary incisors also supra-erupt.111,139 The anterior bite may stay closed or even become deep, depending on the extent of maxillary and mandibular incisor supra-eruption.5,23,71,93–97,133 Whether the incisor relationship remains deep, normal, or open, lip incompetence (i.e., ≥4 mm of lip separation at rest) occurs, with mentalis strain that results from attempts to achieve lip closure.27,99,100
Functional Aspects
• Wide lip separation occurs, with excessive effort required during attempts to achieve lip seal.
• Chronic obstructive nasal breathing as a result of increased intranasal airway resistance (e.g., septal deviation, enlarged inferior turbinates, tight nasal aperture, elevated nasal floor) is frequent (see Chapter 10).
• Classic articulation errors in speech as a result of the anterior open bite and lip incompetence are expected (see Chapter 8).
• Chewing and swallowing difficulties caused by the anterior open-bite malocclusion are expected (see Chapter 8).
• Detrimental effects on the dentition and the periodontium as a result of long-term traumatic malocclusion, the displacement of the teeth outside of the alveolar bone housing, or previous camouflage orthodontic and restorative treatments may be seen.
• The incidence of temporomandibular disorder may be higher than it is among individuals with normal jaw harmony and occlusion (see Chapter 9).
Clinical Characteristics
• Excessive anterior facial height, primarily in the lower third of the face
• Lip incompetence (i.e., resting lip separation of ≥4 mm)
• Increased exposure of the gingiva with a broad smile (i.e., a gummy smile)
• Increased frequency of anterior open bite (although one third of patients present with a normal or deep bite and only 15% have an open bit of >4 mm)
• Mandibular deficiency with Class II malocclusion is frequent (this can range from Class I to Class III)
• A mandible that is rotated downward and backward (i.e., clockwise rotation)
• An excessively full, curled lower lip when in a relaxed position
• Increased vermillion exposure of the lower lip
• A constricted or narrow alar base width, with depressed paranasal regions
• The appearance of a flat or sunken midface, without aesthetically pleasing facial curves or contours
• A negative vector relationship of the ocular globe to the lower eyelid
Dental Findings
• Anterior open bite (may be normal or deep)
• Excessive alveolar height in the anterior maxillary region (this will raise the floor of the nose and partially obstruct nasal airflow)
• Mandibular incisors that are upright, with crowding
• Accentuated curve of Spee as a result of the overeruption of the mandibular incisors
• Tendency toward a narrow, V-shaped maxillary arch with posterior crossbites (this is seen in approximately 50% of patients)
• Occlusal surface enamel wear on the posterior teeth as a result of grinding (secondary occlusal trauma) or previous occlusal equilibration performed in an attempt to close the anterior open bite
Radiographic Findings
• Excessive eruption of the maxillary posterior teeth (i.e., the distance from the palatal plane to the cusps of the molars)
• Maxillary horizontal deficiency
• Clockwise rotation of the maxilla (i.e., an increased palatal plane angle)
• Increased lower anterior facial height
• Clockwise rotation of the mandible (i.e., an increased mandibular plane angle)
• Normal or short mandibular ramus height
• Mandibular posterior teeth not excessively erupted
• Excessive eruption of the maxillary and mandibular incisors: with enough anterior hypereruption, a normal or deep overbite is more likely
• Measurable excessive eruption of the maxillary incisors (i.e., the distance from the floor of the nose to the incisal edge)
• Measurable excessive eruption of the mandibular incisors (i.e., the distance from the menton to the incisal edge)
Fields and colleagues presented simplified cephalometric diagnostic criteria.44 If a patient has all three of the following criteria, he or she can be considered to have a long face growth pattern:
Etiologic Considerations
Current thinking is that both environmental influences and inherited tendencies play a role in the development of a long face.53,66,67,85–87 A significant percentage of patients with long faces have been found to have an increased oral and decreased nasal breathing pattern.25,33,37,52,59,82,134,146,150 Interestingly, nasal obstruction is not always present with long face growth patterns, but an open-mouth posture during development is typical. Other causes of an open-mouth posture in the preadolescent patient have been shown to result in similar long face dysmorphology.1,2,4,51,61,78,80,140 This includes muscle weakness syndromes (e.g., Moebius syndrome, facial nerve palsy, cerebral palsy, muscular dystrophy) and the presence of a large tongue (e.g., Beckwith-Wiedemann syndrome, hemangioma, vascular malformations, neurofibromatosis, Proteus syndrome; see Chapter 4).
There is experimental animal model research to support the theory that a long face anterior open-bite malocclusion is a physiologic adaptation to an open-mouth protrusive tongue posture that is present during facial development (see Chapters 4 and 10).62–65 It has also been clarified that, in humans, a resting open-mouth protrusive tongue posture is an etiologic factor in the development of a long face with an anterior open bite. Interestingly, the intermittent occurrence of tongue thrust during speech and swallowing is not thought to be the cause of an open bite. In fact, periodic tongue thrusting is an adaptive response to an open bite rather than the cause.47 When the incisors overlap in an average way (i.e., with a normal overbite), the normal-sized tongue is naturally placed behind the teeth to create the necessary anterior seal for successful swallowing and the articulation of specific consonant sounds (see Chapter 8). In the presence of anterior open bite, the normal tongue must protrude past the teeth to seal against the lips. This is an expected adaptive mechanism to assist with swallowing and speech. Confirmation that the protrusive tongue position during swallowing and speech is a reversible adaptation has been routinely documented after the individual with a long face and an anterior open bite undergoes successful orthognathic surgery and orthodontic treatment.89,142,155 When the open bite is closed with the use of sound biologic mechanics (i.e., without orthodontic dental compensation) and when lip competence is achieved through surgery (i.e., there is no longer excess lower facial height), there is a fairly reliable elimination of the tongue thrust without the need for active myofunctional physical therapy retraining. However, if a skeletal anterior open bite has been closed with the use of unsound orthodontic maneuvers (i.e., excessive eruption of the anterior teeth or buccal tipping of the molars outside of the alveolar bone housing) and if lip competence is not achieved (i.e., inadequate facial height shortening), dental relapse is to be expected. In this case, tongue thrusting should not be blamed for the recurrent malocclusion.
An Orthodontic Molar Intrusion Approach
Sato and colleagues believe high-angle Class II malocclusions can be corrected with the use of “multiloop edgewise arch wires.”124 With the use of tip-back mechanics and vertical elastics, the researchers believe that the occlusal plane inclination can be altered by intruding the molars via the autorotation of the mandible and the closure of the open bite. Unfortunately, scientific evidence in support of this method of treatment for a patient with a long face and an anterior open bite has not been forthcoming.
With the use of skeletal temporary anchorage devices, the intrusion of the molars has been recommended by some to close an open bite.105,157,158 Man-Suk and colleagues completed a study to examine the long-term stability of anterior open-bite correction via the intrusion of the maxillary posterior teeth in adults.88 In the first group (n = 5 adults), mini-screw implants were placed on the buccal and palatal sides, between the roots of the maxillary second premolars and first molars and between the roots of the maxillary first and second molars. Intrusion forces were directly applied to the molars with elastomeric chains. In the second group (n = 4 adults), mini-screw implants were placed on the buccal side only between the roots of the maxillary second premolars and first molars and between the roots of the maxillary first and second molars. A rigid transpalatal arch was placed before applying the intrusive forces to prevent the buccal tipping of the teeth. Lateral cephalograms were taken at the initial evaluation and again at 1 and 3 years after treatment. The cephalograms were traced and analyzed. The study documented that the maxillary first molars were intruded on an average of 2.39 mm during treatment, with relapse of 0.45 mm at the 3-year follow up (i.e., 22.9% relapse). A majority of the relapse occurred during the initial posttreatment year. The molar relapse had a significant effect on the eventual incisal overbite. There was no significant difference in molar relapse or the maintenance of overbite between the two different methods of skeletal anchorage used. It would appear as though there is currently no known way to fully retain an orthodontically intruded molar.
For patients with borderline long face growth patterns in whom the open bite has been successfully closed with the use of orthodontic mechanics and in whom the remaining gummy smile and lip incompetence is only mild, a vertical reduction with horizontal advancement genioplasty may improve the profile aesthetics and lip competence enough to be a satisfactory compromise for the patient (see Chapter 37 and 40).
Definitive Reconstruction
Timing of Orthognathic Surgery
Orthodontic or surgical interventions undertaken in the individual with a long face growth pattern will not be definitive if significant jaw growth continues after treatment. In our experience, when the increased intranasal airway resistance is simultaneously managed as part of the definitive jaw reconstruction, excessive ongoing vertical growth ceases.108,110 Even if minor degrees of vertical growth were to continue, it should occur in both the mandible and the maxilla in a proportionate way.
Horizontal jaw growth maturation may be analyzed with the use of serial lateral cephalometric radiographs. These sequential radiographs can be used to make direct mandibular measurements. Surgery is delayed until the deceleration of growth can be documented. The best evidence available indicates that, when orthognathic surgery is undertaken in the mandibular-deficient patient as early as completion of the adolescent growth spurt, forward growth of the mandible almost never occurs.135 Further horizontal growth of the maxilla at this age is also not expected.
For all of these reasons, proceeding with definitive orthognathic and intranasal surgery for the patient with a Class II long face growth pattern when he or she is as young as 14 years old is generally safe from a growth perspective, but only after the eruption and orthodontic alignment of the teeth (Fig. 21-4).
Preorthodontic Periodontal Considerations
Orthodontic attempts to compensate the occlusion in the patient with a long face growth pattern may result in gingival recession along the labial aspect of the lower incisors and the buccal aspect of the posterior maxillary teeth. The advantage of bicuspid extractions in the mandible or the maxilla should always be considered to achieve full positioning of the dental roots solidly in the alveolar bone (see Chapter 6).
When lip competence and an improved nasal airway have been achieved as a result of jaw and intranasal procedures, the dryness of the gingiva (ex. inflammation) will also diminish (see Chapter 6).
Orthodontic Preparation for Orthognathic Surgery
The orthodontic mechanics should be oriented toward positioning of the teeth solidly in the alveolar housing within each arch and specifically within each maxillary segment as indicated.128,132,145,149,151 A goal is for the teeth to occlude together appropriately at the time of surgery and after finishing orthodontics. The preferred and anticipated occlusion is best confirmed via the periodic review of dental models (see Chapter 5).
With maxillary surgical segmentation planned, the orthodontist’s presurgical goal is to level the teeth independently within each segment. With a decision made to also defer arch expansion to the surgical phase (i.e., segmental osteotomies with widening), the orthodontic alignment of the teeth within each segment becomes the preoperative objective. Furthermore, there is no need or advantage for the orthodontist to create a space at the planned interdental osteotomy sites (i.e., between the lateral incisor and canine on each side or between the central incisors), because the roots are naturally divergent (see Chapter 17). The orthodontic preparation before surgery should incorporate the following basic concepts:
1. The mandibular arch is leveled with the use of standard orthodontic mechanics before surgery. A patient with a long face does not generally have a severely exaggerated curve of Spee in the lower arch. Therefore, complete leveling is generally carried out before surgery (with or without the need for extractions).
2. The presence of an excessive reverse curve of Spee in the maxillary arch is an indication of a skeletal problem rather than a dental one. Orthodontic leveling of the arch in segments (i.e., four incisors, the canine through the second molar on the left side, and the canine through the second molar on the right side) is generally consistent with the skeletal dysmorphology, and it is carried out before surgery. With the curve of Spee orthodontically leveled in each of the three components, segmental Le Fort I osteotomies will allow for the placement of the three individually leveled components over the orthodontically leveled mandibular arch to achieve the preferred occlusion at operation.
3. The presence of a narrow maxilla is an indication of skeletal dysplasia rather than dental malposition. Orthodontic tooth movement should remain consistent with the narrow skeletal width. Each posterior segment (i.e., the canine through the second molar on the left side and the canine through the second molar on the right side) should be independently orthodontically leveled. Segmentation of the down-fractured maxilla will then adjust the arch width to the orthodontically leveled mandibular arch. If the posterior teeth have not been orthodontically positioned fully within the alveolar housing (e.g., if there is buccal tipping of molars), dental relapse after surgery with a return of the narrow maxillary arch width and the open-bite malocclusion is more likely to occur (see Chapter 17).
Basic Mandibular Arch Mechanics
• Routine orthodontic mechanics are used to level, align, close up spaces, and achieve appropriate arch form in the lower jaw.
• Extraction of a bicuspid in each quadrant (or of a single incisor, in rare cases) or interproximal reduction may be needed in the lower arch to uncrowd the dental crowns, to set the roots solidly in the alveolar housing, and to correct incisor inclination.
Basic Maxillary Arch Mechanics
• In the presence of vertical skeletal discrepancies, presurgical orthodontic stabilization may be achieved with sectional finishing wires that conform to the arch shape of each segment.
• If no vertical segmental skeletal discrepancies exist, then the maxillary arch is leveled with a continuous arch wire. Care is taken to prevent the forward flaring of the incisors. Posterior intrusion mechanics are also avoided, because they predispose the patient to late dental relapse.
• The advantage of bicuspid extractions to position the remaining roots solidly in alveolar housing should always be considered.
• In our experience, planning the interdental osteotomies between the canines and the first bicuspids is rarely preferred. Segmentation in this location is technically more time-consuming for the orthodontist (i.e., precise intercanine width orthodontic detailing becomes necessary), and it is more prone to dental injury and periodontal sequelae (i.e., pocketing and gingival recession) from the interdental osteotomy at surgery.
• Segmentation between the lateral incisors and the canines is generally preferred. When segmenting in this location, it is not necessary or advantageous for the orthodontist to create space at the planned osteotomy sites, because the roots are naturally divergent. The advantages of segmenting the maxilla in this location (i.e., between the lateral incisor and the canine) on each side and then parasagittally (i.e., down the hard palate) include the simplification of orthodontic mechanics, the prevention of periodontal sequelae, and the ability to positively influence incisor inclination without negatively affecting the vertical facial height.
Basic Surgical Approach
The surgical approach for the treatment of a classic long face is best carried out through a combination of osteotomies, including Le Fort I osteotomy in segments, bilateral sagittal split ramus osteotomies, and oblique osteotomy of the chin (Figs. 21-1 through 21-10).* Management of the anterior neck soft tissues—including cervical soft-tissue flap elevation, neck defatting, and vertical platysmal muscle plication—can also be carried out, if desired (see Chapter 40). The removal of the impacted wisdom teeth is frequently recommended for long-term dental health. If this is planned, it can be accomplished at the same time (see Chapters 15 and 16).



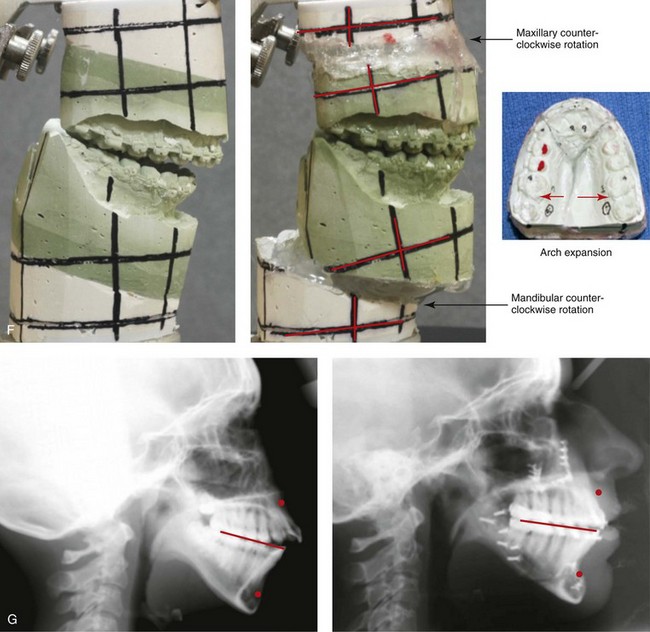
Figure 21-1 A 15-year-old girl arrived with her parents for surgical evaluation. Her history and physical examination confirmed nasal obstruction, heavy snoring, lip incompetence, difficulty chewing, and frequent speech articulation errors. The facial aesthetic concerns included an awareness of a weak chin, a gummy smile, and the impression of having a large nose. The patient had been under an orthodontist’s care since the mixed dentition. Rapid palatal expansion and full bracketing with attempted closure of the anterior open bite were not successful. Further evaluations were carried out by a speech pathologist and an otolaryngologist, and a fresh look was taken at the patient’s orthodontic needs. Orthodontic decompensation in combination with orthognathic and intranasal surgery was chosen. The simultaneous procedures carried out included Le Fort I osteotomy in segments (horizontal advancement, and vertical shortening, counterclockwise rotation, arch expansion, and the correction of the curve of Spee); sagittal split ramus osteotomies (horizontal advancement and counterclockwise rotation); osseous genioplasty (vertical shortening and horizontal advancement); and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Oblique facial views before and after reconstruction. D, Profile views before and after reconstruction. E, Occlusal views before retreatment, with orthodontic decompensation in progress, and after the completion of treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after surgery.



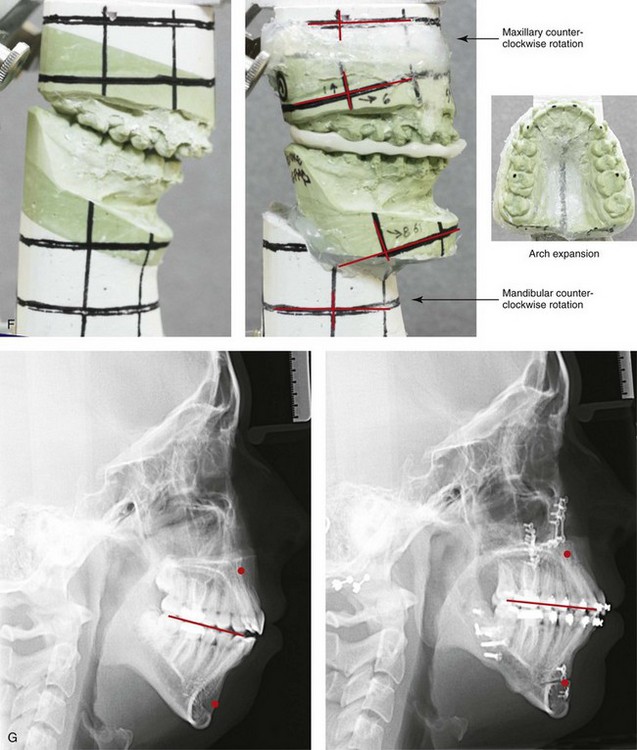
Figure 21-2 A 15-year-old girl arrived with her parents for surgical evaluation. Her history and physical examination confirmed lifelong nasal obstruction, heavy snoring, and lip incompetence. The facial aesthetic concerns included an awareness of a weak chin, a gummy smile, wide lip separation, and a deep lip curl. The patient had been under orthodontic observation since the mixed dentition. Further evaluations were carried out by a speech pathologist and an otolaryngologist. Orthodontic decompensation in combination with orthognathic and intranasal surgery was chosen. The simultaneous procedures carried out included Le Fort I osteotomy in segments (horizontal advancement, vertical shortening, arch expansion, the correction of the curve of Spee, and counterclockwise rotation); sagittal split ramus osteotomies (horizontal advancement and counterclockwise rotation); osseous genioplasty (vertical shortening and horizontal advancement); and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Profile facial views before and after reconstruction. D, Oblique views before and after reconstruction. E, Occlusal views before treatment, with orthodontic decompensation in progress, and after the completion of treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after surgery.



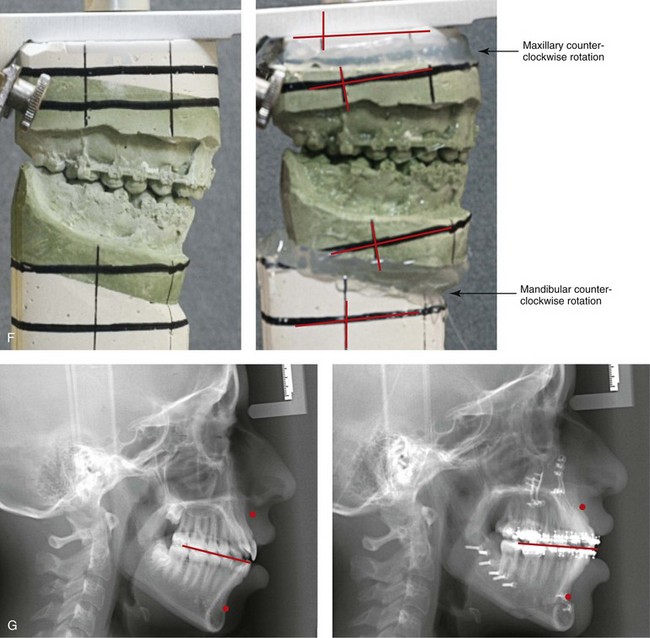
Figure 21-3 A 15-year-old girl arrived with her parents for surgical evaluation. Her history and physical examination confirmed lifelong nasal obstruction and lip incompetence. The facial aesthetic concerns included an awareness of a weak chin, a gummy smile, and wide lip separation. The patient had been under an orthodontist’s care since the mixed dentition and underwent a full course of treatment. Further evaluations were carried out by a speech pathologist and an otolaryngologist, and a fresh look was taken at the patient’s orthodontic needs. Orthodontic decompensation in combination with orthognathic and intranasal surgery was chosen. The simultaneous procedures carried out included Le Fort I osteotomy in segments (horizontal advancement, vertical); sagittal split ramus osteotomies (horizontal advancement and counterclockwise rotation); osseous genioplasty (vertical shortening and horizontal advancement); and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Oblique facial views before and after reconstruction. D, Profile views before and after reconstruction. E, Occlusal views before retreatment, with orthodontic decompensation in progress, and after the completion of treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after surgery.


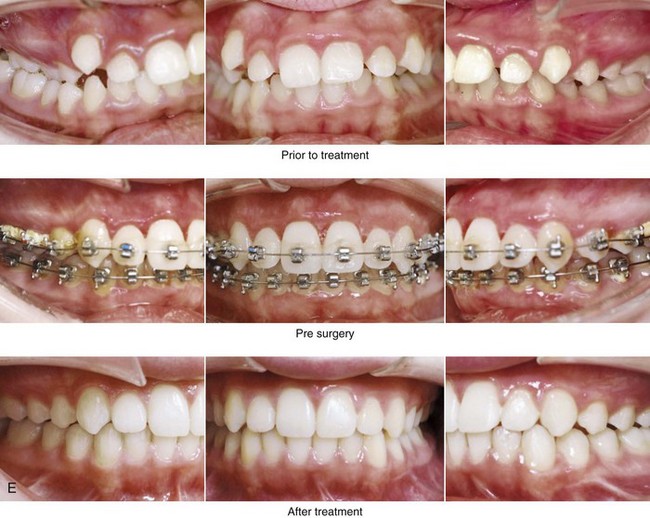
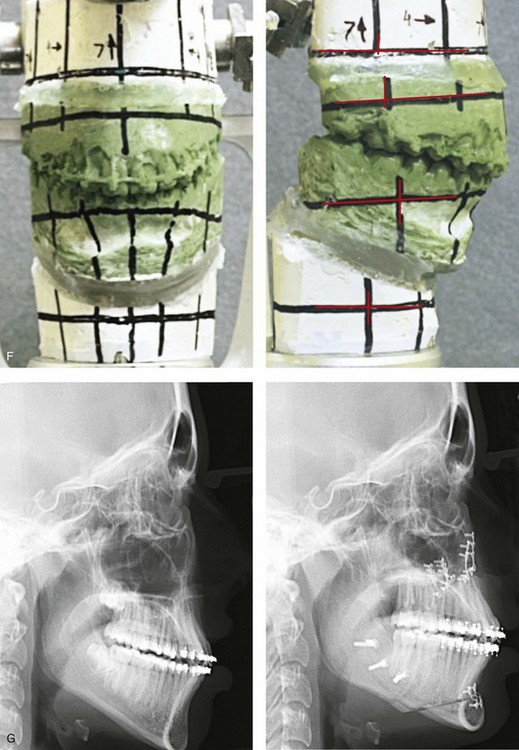
Figure 21-4 A 13-year-old girl arrived with her parents for surgical evaluation. Her history and physical examination confirmed lifelong nasal obstruction, heavy snoring, lip incompetence, and persistent gingivitis despite good home care. The facial aesthetic concerns included an awareness of a weak chin, a gummy smile, and severe lip strain. Further evaluations were carried out by a speech pathologist and an otolaryngologist, and a fresh look was taken at the patient’s orthodontic needs. Orthodontic decompensation in combination with orthognathic and intranasal surgery was chosen. The simultaneous procedures carried out included Le Fort I osteotomy (horizontal advancement, and vertical shortening); sagittal split ramus osteotomies (horizontal advancement and counterclockwise rotation); osseous genioplasty (vertical shortening and horizontal advancement); and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Oblique facial views before and after reconstruction. D, Profile views before and after reconstruction. E, Occlusal views before treatment, with orthodontic decompensation in progress, and after the completion of treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after surgery.


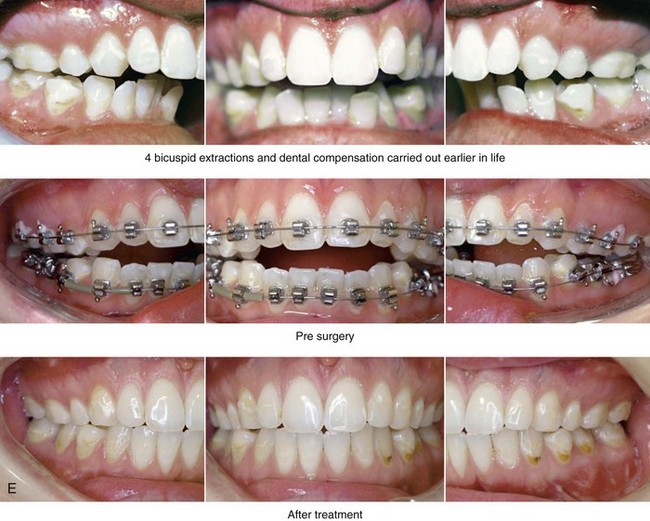
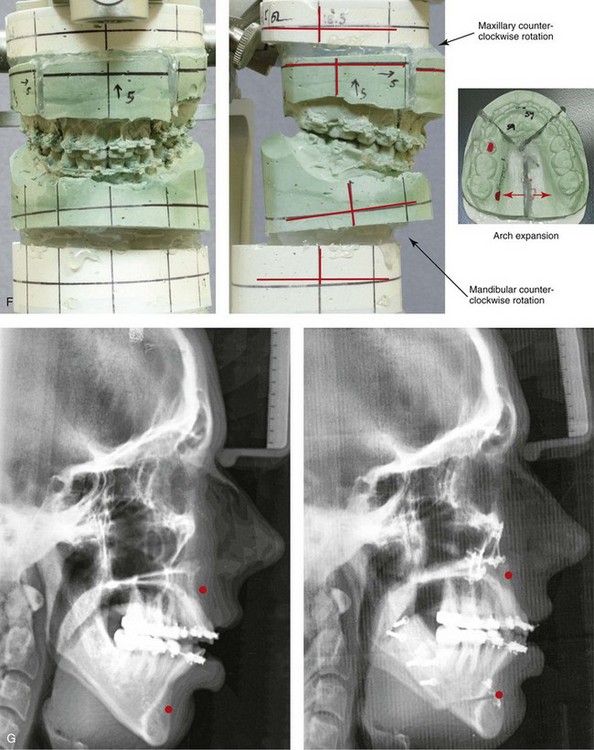
Figure 21-5 A 21-year-old woman arrived for surgical evaluation. Her history and physical examination confirmed lifelong nasal obstruction, lip incompetence, difficulty chewing, and frequent speech articulation errors. The facial aesthetic concerns included an awareness of a weak chin, a gummy smile, lip strain, and the impression of having a larger nose. The patient had been under an orthodontist’s care since the mixed dentition and through the high school years. Growth modification attempts followed by rapid palatal expansion and full bracketing with four bicuspid extractions were unsuccessful to close the anterior open bite. Early periodontal and dental deterioration were evident. Further evaluations were carried out by a speech pathologist, an otolaryngologist, and a periodontist, and a fresh look was taken at the patient’s orthodontic needs. Orthodontic decompensation in combination with orthognathic and intranasal surgery was chosen. The simultaneous procedures carried out included Le Fort I osteotomy in segments (horizontal advancement, vertical shortening, counterclockwise rotation, arch expansion, and the correction of the curve of Spee); sagittal split ramus osteotomies (horizontal advancement and counterclockwise rotation); osseous genioplasty (vertical shortening and horizontal advancement); and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Oblique facial views before and after reconstruction. D, Profile views before and after reconstruction. E, Occlusal views before retreatment, with orthodontic decompensation in progress, and after the completion of treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after surgery.


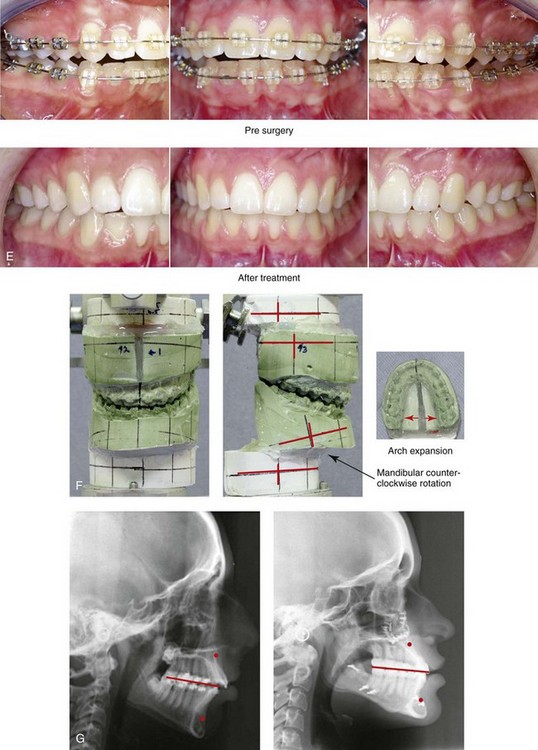
Figure 21-6 A 15-year-old girl arrived with her parents for surgical evaluation. Her history and physical examination confirmed lifelong nasal obstruction, heavy snoring, lip incompetence, difficulty chewing, and frequent speech articulation errors. The facial aesthetic concerns included an awareness of a weak chin, a gummy smile, and difficulty holding the lips together. The patient had been under an orthodontist’s care since the mixed dentition. Rapid palatal expansion and full bracketing with attempted closure of the anterior open bite were unsuccessful. Further evaluations were carried out by a speech pathologist and an otolaryngologist, and a fresh look was taken at the patient’s orthodontic needs. Orthodontic decompensation in combination with orthognathic and intranasal surgery was chosen. The simultaneous procedures carried out included Le Fort I osteotomy in segments (horizontal advancement, vertical shortening, counterclockwise rotation, and arch expansion); sagittal split ramus osteotomies (horizontal advancement and counterclockwise rotation); osseous genioplasty (vertical shortening and horizontal advancement); and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Oblique facial views before and after reconstruction. D, Profile views before and after reconstruction. E, Occlusal views with orthodontic decompensation in progress and after the completion of treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after surgery.
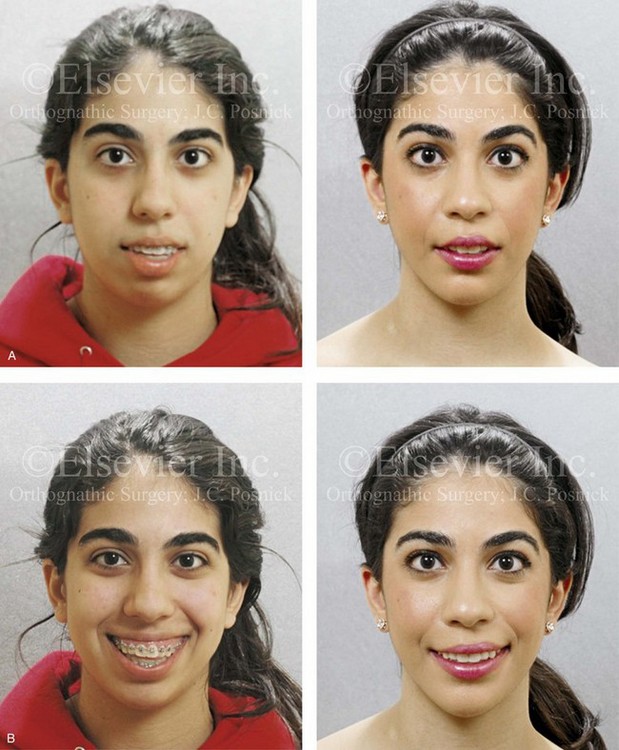

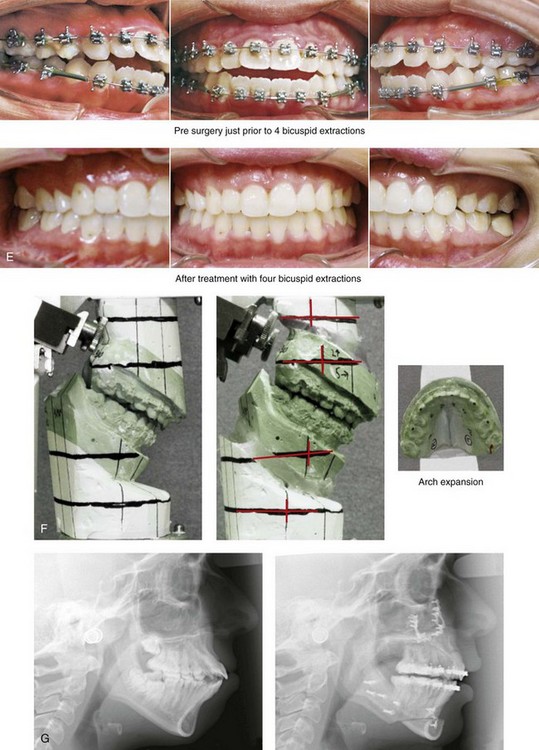
Figure 21-7 A high-school girl arrived with her parents for evaluation. She refused an orthognathic approach at the time but then returned during her college years to request correction. Her history and physical examination confirmed nasal obstruction, lip incompetence, and difficulty chewing. The facial aesthetic concerns included an awareness of a weak chin, a gummy smile, lip strain, and the impression of having a larger nose. The patient had been under an orthodontist’s care since the mixed dentition. Rapid palatal expansion and full bracketing with attempted closure of the anterior open bite were not successful. Further evaluations were carried out by a speech pathologist and an otolaryngologist, and a fresh look was taken at the patient’s orthodontic needs. Orthodontic decompensation that included four bicuspid extractions in combination with orthognathic and intranasal surgery was chosen. The simultaneous procedures carried out included Le Fort I osteotomy in segments (horizontal advancement, vertical shortening, and arch expansion); sagittal split ramus osteotomies (horizontal advancement); osseous genioplasty (vertical shortening and horizontal advancement); and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Oblique facial views before and after reconstruction. D, Profile views before and after reconstruction. E, Occlusal views with orthodontic decompensation in progress and then after the completion of treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after surgery.


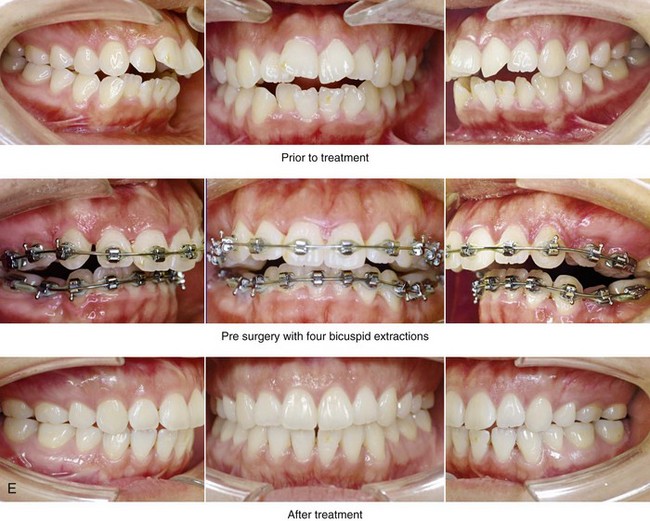
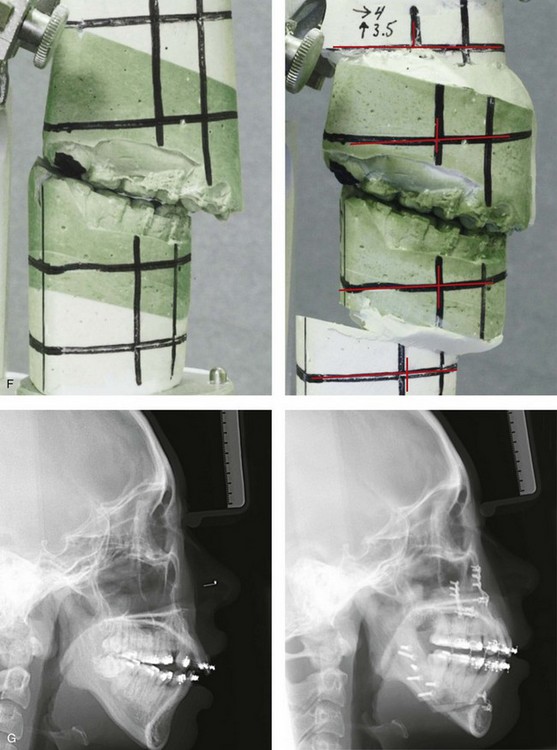
Figure 21-8 A high-school girl arrived with her parents for evaluation. Her history and physical examination confirm a long face growth pattern with nasal obstruction, lip incompetence, and a gummy smile. Orthodontic decompensation including four bicuspid extractions in combination with orthognathic and intranasal surgery was chosen. The simultaneous procedures carried out included Le Fort I osteotomy in segments (horizontal advancement, vertical shortening, and arch expansion); sagittal split ramus osteotomies (horizontal advancement); osseous genioplasty (vertical shortening and horizontal advancement); and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A, Frontal views in repose before and four years after reconstruction. B, Frontal views with smile before and after reconstruction. A degree of gummy smile remains but without lip strain during closure and with satisfactory lip separation in repose. C, Oblique facial views before and after reconstruction. D, Profile views before and after reconstruction. E, Occlusal views before treatment, with orthodontic decompensation including four bicuspid extractions in progress, and after the completion of treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after surgery.
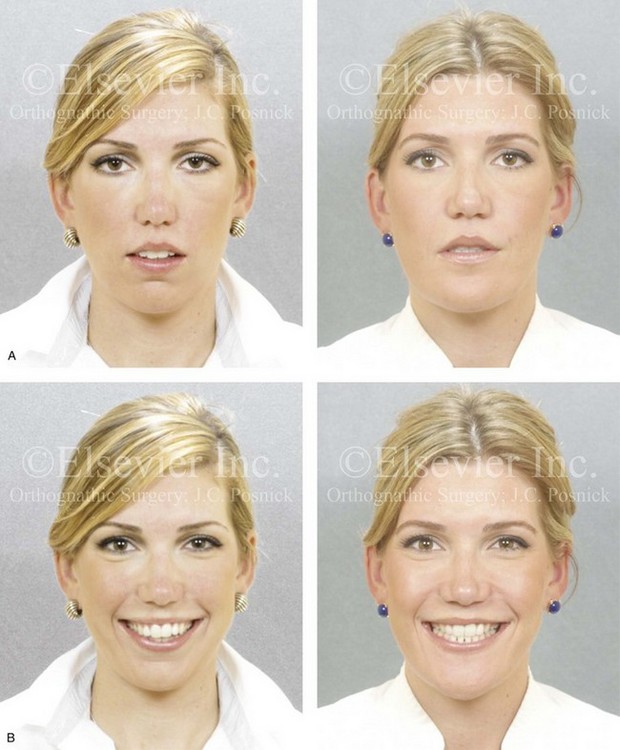


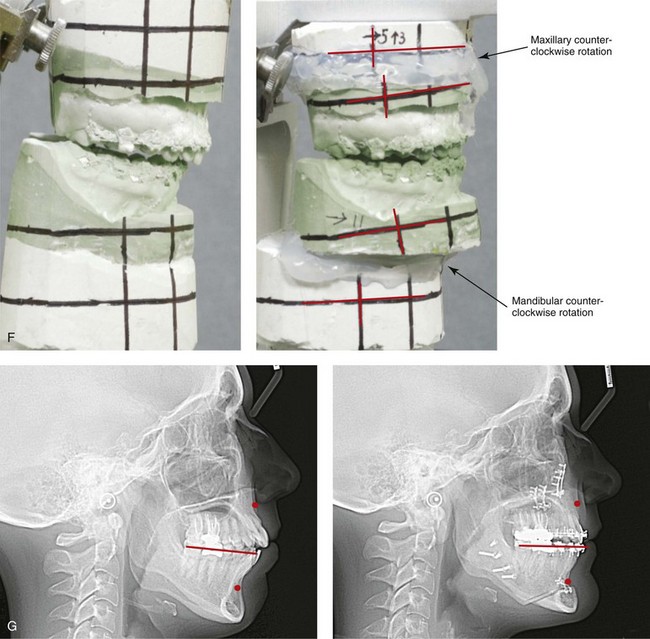
Figure 21-9 A young woman arrived for surgical evaluation. Her history and physical examination confirmed lifelong nasal obstruction, lip incompetence, difficulty chewing, and frequent speech articulation errors. The facial aesthetic concerns included an awareness of a weak chin, a gummy smile, lip strain, and the impression of having a larger nose. The patient had experienced secondary occlusal trauma with a need for root canal therapy and crowns on multiple posterior teeth. Further investigations were carried out by a speech pathologist and an otolaryngologist, and a fresh look was taken at the patient’s requirements for the achievement of a satisfactory occlusion. Orthodontic decompensation including four bicuspid extractions in combination with orthognathic and intranasal surgery was chosen. The simultaneous procedures carried out included Le Fort I osteotomy (horizontal advancement, vertical shortening, and counterclockwise rotation); sagittal split ramus osteotomies (horizontal advancement and counterclockwise rotation); osseous genioplasty (vertical shortening and horizontal advancement); and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Oblique facial views before and after reconstruction. D, Profile views before and after reconstruction. E, Occlusal views before retreatment, with orthodontics in progress including four bicuspid extractions in progress, and after the completion of treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after surgery.


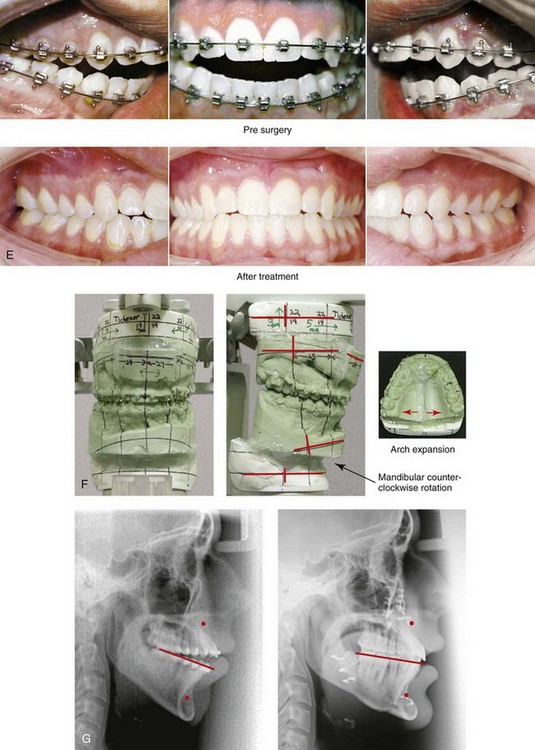
Figure 21-10 A 17-year-old boy arrived with his parents for surgical evaluation. His history and physical examination confirmed lifelong nasal obstruction, heavy snoring, difficulty chewing, and frequent speech articulation errors. The facial aesthetic concerns include an awareness of a gummy smile, lip strain, and a weak profile. Earlier during his life, he had undergone orthodontics that included rapid palatal expansion and full bracketing, without success. An anterior open bite and constricted arch-width malocclusion remained. Further evaluations were carried out by a speech pathologist and an otolaryngologist, and a fresh look was taken at the patient’s orthodontic needs. Orthodontic decompensation in combination with orthognathic and intranasal surgery was chosen. The simultaneous procedures carried out included Le Fort I osteotomy in segments (horizontal advancement, vertical shortening, counterclockwise rotation, arch expansion, and the correction of the curve of Spee); sagittal split ramus osteotomies (horizontal advancement and counterclockwise rotation); osseous genioplasty (vertical shortening and horizontal advancement); and septoplasty, inferior turbinate reduction, and nasal floor recontouring. A, Frontal views in repose before and after reconstruction. B, Frontal views with smile before and after reconstruction. C, Oblique facial views before and after reconstruction. D, Profile views before and after reconstruction. E, Occlusal views with orthodontic decompensation in progress and after the completion of treatment. F, Articulated dental casts that indicate analytic model planning. G, Lateral cephalometric radiographs before and after surgery.
If septoplasty, inferior turbinate reductions, or both are required to improve nasal airflow, then the procedures are carried out simultaneously (see Chapter 10).108–110 For the patient with a long face growth pattern, an important aspect of nasal aesthetics and airway management is to also simultaneously lower and recontour the floor of the nose, the pyriform rims, and the anterior nasal spine region. In 1985, Ellis used lateral cephalometric radiographs to study the specific regions of vertical maxillary excess in mature individuals (i.e., >17 years old) with long faces.36 In the study patients, the linear distance between the incisal edge and the floor of the nose (i.e., the upper incisal edge to the anterior nasal spine) was found to be significantly increased. In other words, the anterior floor of the nose was excessively high, which at least partially accounted for the diminished nasal aperture opening. Ellis recognized that, when a standard Le Fort I maxillary intrusion is carried out to decrease the gummy smile, the elimination of any excessive alveolar bone in the area of the pyriform fossa should also be considered. In these cases, I recommend that the floor of the nose and the anterior nasal spine regions be recontoured to lower the floor. When this is done, the nasal airway is improved, and the “bunching” of the nasal and paranasal soft tissues is avoided. I agree with Ellis and Westermark that the popular use of an alar cinch stitch is generally carried out as a soft-tissue attempt to solve a skeletal problem.36,154 Although the alar cinch stitch will have effects on the nasal base width, it will also have secondary effects on the nasolabial angle and the nasal tip projection that may not be positive.118 In addition, if the cinch stitch is completed without fully correcting the skeletal aspects (i.e., lowering the nasal floor and recontouring the anterior nasal spine), suboptimal nasal aesthetics and further airway obstruction are likely.55,92,144
One of the indications for the segmenting of the maxilla is to correct transverse dental width deficiencies.7,9,10,22,56,77,79,129,130 In the past, problems of stability with transverse expansion have led some clinicians to recommend a two-stage surgical approach to maxillary reconstruction for a long face growth pattern. The first stage involves surgically assisted rapid palatal expansion to widen the maxilla during the presurgical orthodontic phase of treatment. Approximately 6 to 18 months later, a Le Fort I down-fracture osteotomy is carried out as part of the definitive orthognathic correction to reposition the maxilla vertically and horizontally, as indicated. As discussed in Chapter 17, I recommend a single-stage orthognathic approach in most cases. This includes a Le Fort I down-fracture osteotomy with segmentation to simultaneously correct the curve of Spee; any transverse discrepancy; vertical dysplasia; horizontal dysplasia; canting (i.e., roll orientation); any midline discrepancies (i.e. yaw orientation); and A-point to B-point discrepancies (i.e., pitch orientation).
Immediate Presurgical Planning
The immediate presurgical planning takes into account collaborative clinical efforts among the orthodontist, the surgeon, the patient, and the family that will have been ongoing since the initial consultation visits.* Depending on the condition of the dentition and the supporting structures, the restorative dentist and the periodontist may also have been intricately involved.The patient’s specific medical and dental records are reviewed, including radiographs (e.g. computed tomography scans; panoramic, lateral, and posteroanterior cephalometric images and periapical radiographs); facial and occlusal photographs; and dental models. Immediate presurgical records (i.e., within 2 to 6 weeks of surgery) will most importantly include facial measurements taken during a direct visual examination of the patient; alginate impressions of the maxilla and the mandible; centric relation bite recording; and face-bow registration.
First, broad-stroke decisions are made regarding the preferred vector changes for each jaw; only then are the precise millimeter distances and angular changes required in each jaw to achieve the desired end result determined (see Chapter 12). Analytic model planning is carried out on the articulated dental casts with use of the Erickson Model Table. Splints are constructed to assist with the achievement of the precise occlusion and preferred facial aesthetics in the operating room (see Chapters 13 and 14).
• The desired vertical positioning of the maxillary incisor crown
• The desired horizontal positioning of the maxillary incisor crown
• The need to reposition the maxillary dental midline to match the facial midline (i.e., yaw orientation)
• The need to alter or correct any maxillary cant (i.e., roll orientation)
• The need to vertically adjust the posterior maxillary height to establish a preferred A-point to B-point relationship of the jaws (i.e., pitch orientation); counterclockwise rotation of the maxillary plane is a frequent maneuver
• The need to or benefit of segmenting the maxilla to alter the arch width or the curve of Spee
Immediate presurgical planning will confirm the anticipated functional and aesthetic advantages of sagittal split ramus osteotomies to reposition the mandible into occlusion with the new maxillary position versus accepting the limitations of mandibular autorotation (i.e., one-jaw surgery). The baseline anterior projection of the maxilla in a patient with a long face is generally deficient and requires horizontal advancement at the level of the maxillary incisors. Horizontal advancement in combination with vertical intrusion and pyriform rim recontouring will limit the undesirable widening of the nose that would otherwise occur with a “straight-up” intrusion of the maxilla and autorotation of the mandible. Simultaneous sagittal split ramus osteotomies of the mandible (i.e., two-jaw surgery) are required to achieve these objectives in almost all cases.118–121 It is also likely that an oblique osteotomy of the chin with vertical shortening and limited horizontal advancement will be advantageous.
The clinician should confirm or refute a lifelong history of chronic obstructive nasal breathing in the patient (see Chapter 10). During the physical examination, intranasal findings that are consistent with increased nasal airway resistance are likely to include septal deviations and inferior turbinate hypertrophy. If the history and physical findings warrant, then septoplasty and inferior turbinate reduction should be carried out to improve nasal breathing. The baseline presence of excess vertical height in the anterior maxilla (i.e., a high nasal floor) with lip incompetence and a constricted nasal width (i.e., a tight nasal aperture) is also typical and will benefit from midface intrusion, arch expansion through segmental osteotomies, and horizontal advancement. Recontouring of the nasal floor, the pyriform rims, and the anterior nasal spine region with a bur on a rotary drill is also an important surgical maneuver to achieve preferred upper lip and nasal aesthetics as well as to ensure maximum improvements in upper airway function (see Chapters 10 and 15).
These maxillary surgical maneuvers will also improve the negative vector ocular globe to lower eyelid relationship that was present preoperatively (see Chapter 25). In the teenager and young adult, this will stabilize the midface and periorbital soft tissues and limit the negative effects that would otherwise likely occur with age (e.g., soft-tissue descent, rounding of the palpebral fissure, lengthening of the lower lid, loss of cheek region soft-tissue prominence).
Surgical Planning Pitfalls
Treating the Gummy Smile
When considering the enhancement of the relationship of the upper lip to the maxillary upper incisors, it is important to avoid the planning pitfall of treating the gummy smile as an isolated feature. The clinician should make decisions about the degree of excessive anterior maxillary height and the extent of planned intrusion primarily on the basis of the anticipated upper lip position in repose and not on its position during a smile (see Fig. 21-8). In the patient with a long face, surgical alteration of the upper lip to tooth relationship will occur for a variety of reasons, including vertical maxillary intrusion; horizontal maxillary advancement; arch expansion; closure of the open bite; shortening of the chin; recontouring the pyriform rims; and recontouring and lowering of the nasal floor. The dynamic lip function and the static lip position after healing cannot be entirely predicted from the combination of skeletal changes that are generally carried out. No accurate quantitative mathematic formula for predicting the postoperative hard tissue to soft tissue changes with this condition is currently available. Keep in mind that as much as 4 mm of incisor crown exposure at rest is fine; a few millimeters of lip incompetence is acceptable, and it is better to show more teeth than less.
Postsurgical Orthodontic Maintenance and Maintenance
In general, the maintenance of the new arch form is the most challenging aspect of the postsurgical orthodontic phase of treatment. With segmentation of the maxilla, a rigid acrylic occlusal splint is prefabricated and secured to the maxillary dentition in the operating room (see Chapter 13). The splint remains in place during the initial bone-healing phase, (approximately 5 weeks). Intermittent intermaxillary elastics are used during this time to retrain the masticatory muscles, to provide motion in the temporomandibular joints, to increase patient comfort, and to confirm the stability of the occlusion. When the splint is removed, the patient should immediately (ideally within 24 hours) return to the orthodontist for the placement of a continuous maxillary arch wire. The surgically expanded arch width and the corrected curve of Spee must be actively orthodontically maintained throughout occlusal finishing (see Chapter 17). In accordance with the orthodontist’s clinical judgment, this is accomplished via some combination of a rigid labial wire, a transpalatal appliance, and a palatal acrylic plate. The placement of a transpalatal appliance at the time of splint removal is facilitated by preoperatively banding the first molars with lingual attachments. The transpalatal appliance can be constructed in advance from the maxillary cast of the model planning. It is often tempting for the orthodontist to rapidly finish treatment and remove the brackets, but this is almost always a mistake. The dentoalveolar segments are generally not fully stable for approximately 6 months. If the maxillary posterior segments relapse after surgery, not only will there be a return of posterior crossbites, but the occlusion also tends to open anteriorly (see Chapter 16).
Complications, Informed Consent, and Patient Education
The orthodontist and the surgeon are asked to evaluate the individual with a long face and then to attempt to alter nature’s events. With a sound understanding of the natural progression of the uncorrected dentofacial deformity and with knowledge of how specific interventions will affect function and facial aesthetics, predictable results are generally expected. The potential risks as compared with the anticipated benefits of each procedure and the review of alternative approaches to manage each problem are taken into account, because complications (i.e., unfavorable outcomes) will always occur in a small percentage of patients. The patient’s willingness to make an informed decision and then to accept responsibility for that choice is an integral aspect of the patient–doctor interaction (see Chapter 17).115
Malocclusion after Orthodontics and Orthognathic Surgery
There are inherent biologic challenges to the orthodontic movement of the teeth within the alveolar process and the surgical repositioning of the jaws and jaw segments in the individual with a long face.* This includes the technical aspects of the repositioning; the initial healing requirements; and the difficulties associated with the long-term maintenance of the mechanically relocated teeth, jaws, and jaw segments. When following sound aesthetic and biomechanical principles, clinicians are able to carry out orthodontic treatment and surgical procedures in the individual with a long face to safely and reliably achieve the desired results in most cases. Potential intraoperative technical difficulties associated with sagittal split ramus osteotomies of the mandible and the maxillary Le Fort I osteotomy that can result in an immediate (early) malocclusion are preventable in most cases (see Chapter 17). Timing the surgical procedures to limit the risk of ongoing jaw growth after surgery is generally possible. The orthodontic removal of dental compensations with the use of bicuspid extractions as needed to place the teeth solidly in the alveolar housing will best ensure stable long-term occlusion and periodontal health (see Chapter 17).
Temporomandibular Disorders: Effects of Orthodontics and Orthognathic Surgery
It is estimated that an average of 32% of the population reports at least one symptom of temporomandibular disorder, whereas an average of 55% demonstrate at least one clinical sign. Temporomandibular disorders include various symptoms and signs of the temporomandibular joints, the masticatory muscles, and the related structures. The symptoms and signs may include a spectrum of referred head and neck discomforts; joint noise (e.g., popping, clicking, crepitus); reduced or altered mandibular movements as a result of muscle spasm or disc displacement, with or without reduction; condylar head erosion; and pain on direct palpation of either temporomandibular joint or of the masticatory muscles. The presence of an anterior open-bite malocclusion is often claimed to be a factor in temporomandibular disorder. The successful correction of the Long Face dentofacial deformity through orthodontics and orthognathic surgery has been documented to improve the pretreatment symptoms of many individuals, but it may accentuate symptoms in others (see Chapter 9).3,103
References
1. Adamides, IP, Spyropoulos, MN. The effects of lymphadenoid hypertrophy on the position of the tongue, the mandible and the hyoid bone. Eur J Orthod. 1983; 5:287–294.
2. Ackerman, RI, Klapper, L. Tongue position and open bite: The key roles in growth and nasopharyngeal airway. ASDC J Dent Child. 1981; 48:339.
3. Aghabeigi, B, Hiranaka, D, Keith, DA, et al. Effect of orthognathic surgery on the temporomandibular joint in patients with anterior open bite. Int J Adult Orthodon Orthognath Surg. 2001; 16:153.
4. Alexander, RG. The effects on tooth position and maxillofacial vertical growth during treatment of scoliosis with the Milwaukee brace. Am J Orthod. 1966; 52:161.
5. Angle, EH. Malocclusion of the teeth, ed 7. Philadelphia: SS White; 1907.
6. Arvystas, MG. Treatment of anterior skeletal open-bite deformity. Am J Orthod. 1977; 72:147–164.
7. Bailey, LJ, White, RP, Proffit, WR, et al. Segmental Le Fort I osteotomy for management of transverse maxillary deficiency. J Oral Maxillofac Surg. 1997; 55:728.
8. Baumrind, S, Korn, EL, West, E. Prediction of mandibular rotation: An empirical test of clinician performance. Am J Orthod. 1984; 86:371–385.
9. Bays, RA, Greco, JM. Surgically assisted rapid palatal expansion. J Oral Maxillofac Surg. 1992; 50:110.
10. Bell, RA. A review of maxillary expansion in relation to rate of expansion and patient’s age. Am J Orthod. 1982; 81:32.
11. Bell, WH. Revascularization and bone healing after anterior maxillary osteotomy: A study using adult rhesus monkeys. J Oral Surg. 1969; 27:249–255.
12. Bell, WH, Levy, BM. Revascularization and bone healing after posterior maxillary osteotomy. J Oral Surg. 1971; 29(4):313–320.
13. Bell, WH. Correction of skeletal type of anterior open bite. J Oral Surg. 1971; 29:706.
14. Bell, WH, Dann, JJ. Correction of dentofacial deformities by surgery in the anterior part of the jaws. Am J Orthod. 1973; 64:162.
15. Bell, WH, Turvey, TA. Surgical correction of posterior crossbite. J Oral Surg. 1974; 32:811.
16. Bell, WH. Le Fort I osteotomy for correction of maxillary deformities. J Oral Surg. 1975; 33:412.
17. Bell, WH, Epker, BN. Surgical-orthodontic expansion of the maxilla. Am J Orthod. 1976; 70:517.
18. Bell, WH, Creekmore, TD, Alexander, RG. Surgical correction of the long face syndrome. Am J Orthod. 1977; 71:40.
19. Bell, WH, McBride, KL. Correction of the long face syndrome by Le Fort I osteotomy. Oral Surg. 1977; 44:493.
20. Bell, WH, Sinn, D. Turbinectomy to facilitate superior movement of the maxilla by Le Fort I osteotomy. J Oral Surg. 1979; 37:129.
21. Bell, WH, Proffit, WP. Vertical maxillary excess. In: Bell WH, Proffit WP, White RP, eds. Surgical correction of dentofacial deformities. Philadelphia: WB Saunders; 1980:272.
22. Betts, NJ, Vanarsdale, RL, Barber, HD, et al. Diagnosis and treatment of transverse maxillary deficiency. Int J Adult Orthodon Orthognath Surg. 1995; 10:75.
23. Bishara, SE, Jakobsen, JR. Longitudinal changes in three normal facial types. Am J Orthod. 1985; 88:466–502.
24. Bjork, A. Prediction of mandibular growth rotation. Am J Orthod. 1969; 55:585–599.
25. Bresolin, D, Shapiro, PA, Shapiro, GG, et al. Mouth breathing in allergic children: its relationship to dentofacial development. Am J Orthod. 1983; 84:334.
26. Brunell, JA, Bhat, M, Lipton, JA. Prevalence and distribution of selected occlusal characteristics in the US population, 1988–1991. J Dent Res. 1996; 75:706.
27. Burstone, CJ. Lip posture and its significance in treatment planning. Am J Orthod. 1967; 53:262.
28. Cangialosi, T. Skeletal morphologic features of anterior open bite. Am J Orthod. 1984; 85:28–36.
29. Cao, Y, Zhou, Y, Li, Z. Surgical-orthodontic treatment of Class III patients with long face problems: A retrospective study. J Oral Maxillofac Surg. 2009; 67:1032–1038.
30. Chamberland, S, Proffit, WL. Short-term and long-term stability of surgically assisted rapid palatal expansion revisited. Am J Orthod Dentofacial Orthop. 2011; 139:815–822.
31. Coben, SE. Growth and class II treatment. Am J Orthod. 1966; 52:5–26.
32. Daniel, HT, White, RP, Proffit, WR. Anterior maxillary osteotomy in dental treatment. J Am Dent Assoc. 1971; 83:338.
33. D’Ascanio, L, Lancione, C, Pompa, G, et al. Craniofacial growth in children with nasal septum deviation: a cephalometric comparative study. Int J Pediatr Otorhinolaryngol. 2010; 74:1180.
34. Dibbets, JMH. The puzzle of growth rotation. Am J Orthod. 1985; 87:473–480.
35. Donatsky, O, Bjorn-Jorgensen, J, Holmqvist-Larsen, M, et al. Computerized cephalometric evaluation of orthognathic surgical precision and stability in relation to maxillary superior repositioning combined with mandibular advancement or setback. J Oral Maxillofac Surg. 1997; 55:1071.
36. Ellis, E. The nature of vertical maxillary deformities: Implications for surgical intervention. J Oral Maxillofac Surg. 1985; 43:756–762.
37. Enache, AM, Nimigean, VR, Mihaltan, F, et al. Assessment of sagittal and vertical skeletal patterns in Romanian patients with obstructive sleep apnea. Rom J Morphol Embryol. 2010; 51:505.
38. Epker, BN, Wolford, LM. Middle third facial osteotomies: Their use in the correction of acquired and developmental dentofacial and craniofacial deformities. J Oral Surg. 1975; 33:491.
39. Epker, BN, Fish, LC. Surgical-orthodontic correction of open-bite deformity. Am J Orthod. 1977; 71:278–299.
40. Epker, BN. A modified anterior maxillary osteotomy. J Maxillofac Surg. 1977; 5:35.
41. Epker, BN, Fish, LC. Superior repositioning of the maxilla: What to do with the mandible? Am J Orthod Dentofacial Orthop. 1980; 78:164.
42. Epker, BN. Superior surgical repositioning of the maxilla: Long-term results. J Maxillofac Surg. 1981; 9:199.
43. Epker, BN, Turvey, TA, Fish, LD. Indications of simultaneous mobilization of the maxilla and mandible for the correction of dentofacial deformities. Oral Surg Oral Med Oral Pathol. 1982; 54:369.
44. Fields, HW, Proffit, HW, Nixon, WL, et al. Facial pattern differences in long-faced children and adults. Am J Orthod. 1984; 85:217–223.
45. Finn, RA. Biomechanical considerations in the surgical correction of mandibular deficiency. J Oral Surg. 1980; 38:257–264.
46. Fish, LC, Wolford, LM, Epker, BN. Surgical-orthodontic correction of vertical maxillary excess. Am J Orthod. 1978; 73:241–257.
47. Fletcher, SG, Casteel, RL, Bradley, DP. Tongue-thrust swallow, speech articulation, and age. J Speech Hear Disord. 1961; 26:201.
48. Forssell, K, Turvey, TA, Phillips, C, et al. Superior repositioning of the maxilla combined with mandibular advancement: Mandibular RIF improves stability. Am J Orthod Dentofacial Orthop. 1992; 102:342.
49. Freihofer, HP, Jr. Results after midface osteotomies. J Maxillofac Surg. 1973; 1:30.
50. Freihofer, HP, Jr. Results of osteotomies of the facial skeleton in adolescence. J Maxillofac Surg. 1977; 5:267.
51. Freng, A, Kvam, E. Facial sagittal growth following partial basal resection of the nasal septum: A retrospective study in man. Eur J Orthod. 1979; 1:89–96.
52. Freng, A. Dentofacial development in the long-lasting nasal stenosis. Scand J Dent Res. 1979; 89:260–267.
53. Ghafari, J, Brin, I, Kelley, MB. Mandibular rotation and lower face height indicators. Angle Orthod. 1989; 59:31–36.
54. Grainger, RM. The Orthodontic Treatment Priority Index. Washington, DC: US Department of HEW, DHEW publication (PHS); 1967.
55. Guenther, TA, Sather, AH, Kern, EB. The effect of Le Fort I maxillary impaction on nasal airway resistance. Am J Orthod Dentofacial Orthop. 1984; 85:308.
56. Haas, AJ. Long-term post treatment evaluation of rapid palatal expansion. Angle Orthod. 1980; 50:189.
57. Hall, HD, Roddy, SC, Jr. Treatment of maxillary alveolar hyperplasia by total maxillary osteotomy. J Oral Surg. 1975; 33:180.
58. Hall, HD, West, RA. Combined anterior and posterior maxillary osteotomy. J Oral Surg. 1976; 34:126.
59. Hannuksela, A. The effects of moderate and severe atopy on the facial skeleton. Eur J Orthod. 1981; 3:187–193.
60. Hapak, FM. Cephalometric appraisal of the open-bite case. Angle Orthod. 1964; 34:65–72.
61. Hart, DL, Lundquist, DO, Davis, HC. The effect of vertical dimension on muscular strength. J Orthop Sports Phys Ther. 1981; 3:57–61.
62. Harvold, EP. The role of function in the etiology and treatment of malocclusion. Am J Orthod. 1968; 54:883–898.
63. Harvold, EP, Chierici, G, Varervik, K. Experiments on the development of dental malocclusion. Am J Orthod. 1972; 61:38–44.
64. Harvold, EP, Vargervik, K, Chierici, G. Primate experiments on oral sensation and dental malocclusion. Am J Orthod Dentofacial Orthop. 1973; 63:494.
65. Harvold, EP, Tomer, BS, Varervik, K, Chierici, G. Primate experiments on oral respiration. Am J Orthod. 1981; 79:359–372.
66. Haryett, RD, Hansen, FC, Davidson, PO. Chronic thumb sucking: The psychological effects and relative effectiveness of various methods of treatment. Am J Orthod Dentofacial Orthop. 1967; 53:569.
67. Haryett, RD, Hansen, FC, Davidson, PO. Chronic thumb sucking: A second report on treatment and its psychological effects. Am J Orthod Dentofacial Orthop. 1970; 57:164.
68. Hedemark, A, Freihofer, HP, Jr. The behaviour of the maxilla in vertical movements after Le Fort I osteotomy. J Maxillofac Surg. 1978; 6:244.
69. Isaacson, JR. Extreme variation in vertical facial growth and associated variation in skeletal and dental relations. Angle Orthod. 1970; 71:219–229.
70. Isaacson, JR, Isaacson, RJ, Speidel, MD, et al. Extreme variations in vertical growth and associated variations in skeletal and dental relations. Angle Orthod. 1971; 41:219.
71. Isaacson, JR, Zappel, RJ, Worms, FW, et al. Effects of rotational jaw growth on the occlusion and profile. Am J Orthod. 1977; 72:276–286.
72. Kahnberg, KE, Ridell, A. Combined Le Fort I osteotomy and oblique sliding osteotomy of the mandibular rami: A follow-up. J Craniomaxillofac Surg. 1988; 16:151.
73. Kawamoto, HK, Jr. Treatment of the elongated lower face and the gummy smile. Clin Plast Surg. 1982; 9:479.
74. Kelley, JE, Sanchez, M, Van Kirk, GE. An assessment of the occlusion of teeth of children 6-11 years. Washington, DC: National Center for Health Statistics, US Dept of Health, Education, and Welfare, Public Health Service publication (HRA); 1973.
75. Kelley, JE, Harvey, CR. An assessment of the occlusion of teeth of youths 12-17 years. Washington, DC: National Center for Health Statistics, US Dept of Health, Education, and Welfare, Public Health Service publication (HRA); 1977.
76. Kondo, E. The course of treatment of a class III skeletal open bite case and its analysis. Aust Orthod J. 1993; 12:217.
77. Krebs, A. Expansion of the midpalatal suture, studied by means of metallic implants. Acta Odontol Scand. 1958; 17:491.
78. Kreiborg, S, Jensen, BL, Møller, E, Björk, A. Craniofacial growth in a case of congenital muscular dystrophy. Am J Orthod. 1978; 74:207–215.
79. Kuo, PC, Will, LW. Surgical-orthodontic treatment of maxillary constriction. Oral Maxillofac Surg Clin North Am. 1990; 2:751.
80. Lear, CSC, Moorrees, CFA. Bucco-lingual muscle force and dental arch form. Am J Orthod Dentofacial Orthop. 1969; 56:379.
81. LeBanc, JP, Turvey, TA, Epker, BN. Results following simultaneous mobilization of the maxilla and mandible for the correction of dentofacial deformities: Analysis of 100 consecutive patients. Oral Surg Oral Med Oral Pathol. 1982; 54:607.
82. Linder-Aronson, S. Adenoids: Their effect on mode of breathing and nasal airflow and their relationship to characteristics of the facial skeleton and the dentition. A biometric, rhino-manometric and cephalometro-radiographic study on children with and without adenoids. Acta Otolaryngol Suppl. 1970; 265:1.
83. Luhr, HG. Zur stabilen osteosynthese bei unterkiefer-frakturen. Dtsch Zahnarztl Z. 1968; 23:754.
84. Luhr, HG. Skelettverlagernde operationen zur harmonisierung des gesichtsprofils-probleme der stabilen fixation von osteotomiesegmenten. In: Pfeifer Gvon, ed. Die esthetik von form und funktion in der plastischen und wiederherstellungs-chirurgie. Berlin: Springer-Verlag; 1985:87.
85. Lundström, A. The importance of genetic and non-genetic factors in the facial skeleton studies in 100 pairs of twins. Trans Eur Orthod Soc. 1954.
86. Lundström, A, Woodside, DG. Individual variation in growth directions expressed at the chin and the midface. Eur J Orthod. 1980; 2:65–79.
87. Lundström, A. Nature versus nurture in dento-facial variation. Eur J Orthod. 1984; 6:77–91.
88. Man-Suk, B, Yoon-Jeong, C, Yu, HS, et al. Long-term stability of anterior open-bite treatment by intrusion of maxillary posterior teeth. Am J Orthod Dentofacial Orthop. 2010; 138:396e1–396e9.
89. Mason, RM, Proffit, WR. The tongue thrust controversy: Background and recommendations. J Speech Hear Disord. 1974; 39:115.
90. McNance, AM, Moss, JP, James, DR. Stability of surgical correction of patients with skeletal III and skeletal II anterior open bite, with increased maxillary mandibular plane angle. Eur J Orthod. 1992; 14:198.
91. Miguel, JA, Turvey, TA, Phillips, C, Proffit, WR. Long-term stability of two-jaw surgery for treatment of mandibular deficiency and vertical maxillary excess. Int J Adult Orthodon Orthognath Surg. 1995; 10:235–245.
92. Mommaerts, MY, Lippens, F, Abeloos, JV, Neyt, LF. Nasal profile changes after maxillary impaction and advancement surgery. J Oral Maxillofac Surg. 2000; 58:470–475.
93. Moss, M, Salentijn, L. Differences between the functional matrices in anterior open-bite and in deep-bite. Am J Orthod. 1971; 60:264–280.
94. Moyers, RE, van der Linden, FPGM, Riolo, ML, et al. Standards of human occlusal development. Ann Arbor: University of Michigan Center for Human Growth and Development; 1976.
95. Muller, G. Growth and development of the middle face. J Dent Res. 1963; 42:385–399.
96. Nahoum, HI. Vertical proportions and the palatal plane in anterior open-bite. Am J Orthod. 1971; 59:273–282.
97. Nahoum, HI, Horowitz, SL, Benedicto, EA. Varieties of anterior open-bite. Am J Orthod. 1972; 61:486–492.
98. Nahoum, HI. Anterior open-bite: A cephalometric analysis and suggested treatment procedures. Am J Orthod. 1975; 67:513–521.
99. Nanda, SK. Patterns of vertical growth in the face. Am J Orthod Dentofacial Orthop. 1988; 93:103–116.
100. Nanda, RS. Growth patterns in subjects with long and short faces. Am J Orthod Dentofacial Orthop. 1990; 98:247–258.
101. Obwegeser, HL, Hadjianghelou, O. Two ways to correct bird-face deformity. Oral Surg Oral Med Oral Pathol. 1987; 64:507–518.
102. Obwegeser, HL. Variations of a standard approach for correction of the bird-face deformity. J Craniomaxillofac Surg. 1988; 16:247–265.
103. O’Ryan, F, Epker, BN. Surgical orthodontics and the temporomandibular joint: I. Superior repositioning of the maxilla. Am J Orthod Dentofacial Orthop. 1983; 83:407.
104. Otuyemi, OD, Jones, SP. Long-term evaluation of treated class II division 1 malocclusions utilizing the PAR index. Br J Orthod. 1995; 22:171–178.
105. Park, YC, Lee, HA, Choi, NC, Kim, DH. Open bite correction by intrusion of posterior teeth with miniscrews. Angle Orthod. 2008; 78:699–710.
106. Phillips, C, Medland, WH, Fields, HW, Jr. Stability of surgical maxillary expansion. Int J Adult Orthodon Orthognath Surg. 1992; 7:139.
107. Posnick, JC, Maxillary excess with or without mandibular deficiency. Craniofacial and maxillofacial surgery in children and young adults. Posnick, JC, eds. Craniofacial and maxillofacial surgery in children and young adults; Vol 39. WB Saunders Co, Philadelphia, 2000:1025–1056.
108. Posnick, JC, Fantuzzo, J, Orchin, J. Deliberate operative rotation of the maxillo-mandibular complex to alter the A-point to B-point relationship for enhanced facial esthetics. J Oral Maxillofac Surg. 2006; 64:1687–1695.
109. Posnick, JC, Fantuzzo, JJ, Troost, T. Simultaneous intranasal procedures to improve chronic obstructive nasal breathing in patients undergoing maxillary (Le Fort I) osteotomy. J Oral Maxillofac Surg. 2007; 65:2273–2281.
110. Posnick, JC, Agnihotri, N. Managing chronic nasal airway obstruction at the time of orthognathic surgery: A twofer. J Oral Maxillofac Surg. 2011; 69:695–701.
111. Proffit, WR, Fields, HW. Occlusal forces in normal- and long-face children. J Dent Res. 1983; 62:571–574.
112. Proffit, WR, Phillips, C, Dann, C, IV. Who seeks surgical orthodontic treatment? Int J Adult Orthodon Orthognath Surg. 1990; 3:153.
113. Proffit, WR, Phillips, C, Douvartzidis, N. A comparison of outcomes of orthodontic and surgical-orthodontic treatment of Class II malocclusion in adults. Am J Orthod Dentofacial Orthop. 1992; 101:556–565.
114. Proffit, WR, Fields, HW, Moray, LJ. Prevalence of malocclusion and orthodontic treatment need in the United States: estimates from the NHANES III survey. Int J Adult Orthodon Orthognath Surg. 1998; 13:97–106.
115. Rees, TD, La Trenta, GS. The long face syndrome and rhinoplasty. Perspect Plast Surg. 1989; 3:24.
116. Reyneke, JP, Evans, WG. Surgical manipulation of the occlusal plane. Int J Adult Orthodon Orthognath Surg. 1990; 5:99–110.
117. Reyneke, JP. Essentials of orthognathic surgery. Chicago: Quintessence Publishing Co Inc; 2003.
118. Rosen, H. Lip-nasal aesthetics following Le Fort I osteotomies. Plast Reconstr Surg. 1988; 82:171.
119. Rosen, H. Facial skeletal expansion: Treatment strategies and rationale. Plast Reconstr Surg. 1992; 89:798.
120. Rosen, H. Occlusal plane rotation: Aesthetic enhancement in mandibular micrognathia. Plast Reconstr Surg. 1993; 91:1231.
121. Rosen, H. Aesthetics in facial skeletal surgery. Perspect Plast Surgery. 1993; 6:1.
122. Sassouni, V, Nanda, S. Analysis of dentofacial vertical proportions. Am J Orthod. 1964; 50:801–823.
123. Sassouni, V. A classification of skeletal facial types. Am J Orthod Dentofacial Orthop. 1969; 55:109.
124. Sato, S, Kaneko, M, Sasaguri, K, et al. Different mechanics for orthodontic correction of Class II openbite and Class III openbite malocclusions. Bull Kanagawa Dent Coll. 2007; 35:65–77.
125. Schendel, SA, Eisenfeld, J, Bell, WH, Epker, B. The long face syndrome: Vertical maxillary excess. Am J Orthod. 1976; 70:398–408.
126. Schendel, SA, Eisenfeld, JH, Bell, WH, et al. Superior repositioning of the maxilla: Stability and soft tissue osseous relations. Am J Orthod Dentofacial Orthop. 1976; 70:663.
127. Schudy, F. Vertical growth versus anteroposterior growth as related to function and treatment. Angle Orthod. 1964; 34–35:75–93.
128. Schudy, FF. The rotation of the mandible resulting from growth: Its implications in orthodontic treatment. Angle Orthod. 1965; 35:36–50.
129. Shetty, V, Cardid, JM, Caputo, AA, et al. Biomechanical rationale for surgical orthodontic expansion of the adult maxilla. J Oral Maxillofac Surg. 1994; 52:742.
130. Silverstein, K, Quinn, PD. Surgically-assisted rapid palatal expansion for management of transverse maxillary deficiency. J Oral Maxillofac Surg. 1997; 55:725.
131. Simmons, KE, Turvey, TA, Phillips, C, Proffit, WR. Surgical-orthodontic correction of mandibular deficiency: Five-year follow-up. Int J Adult Orthodon Orthognath Surg. 1992; 7:67–80.
132. Simmons, KE, Turvey, TA, Phillips, C, Proffit, WR. Sagittal deficiency and vertical maxillary excess. Int J Adult Orthod orthodontic correction of mandibular deficiency: five-year. Orthognath Surg. 1995; 10:235–245.
133. Siriwat, PP, Jarabak, JR. Malocclusion and facial morphology: Is there a relationship? An epidemiologic study. Angle Orthod. 1985; 55:127–138.
134. Sousa, JB, Anselmo-Lima, WT, Valera, FC, et al. Cephalometric assessment of the mandibular growth pattern in mouth-breathing children. Int J Pediatr Otorhinolaryngol. 2005; 69:311.
135. Stahl, F, Baccetti, T, Franchi, L, McNamara, JA. Longitudinal growth changes in untreated subjects with class II division malocclusion. Am J Orthod Dentofacial Orthop. 2008; 134:125–137.
136. Stansbury, CD, Evans, CA, Miloro, M, et al. Stability of open bite correction with sagittal split osteotomy and closing rotation of the mandible. J Oral Maxillofac Surg. 2010; 68:149–159.
137. Stoker, NG, Epker, BN. The posterior maxillary osteotomy: A retrospective study of treatment results. Int J Oral Surg. 1974; 3:153.
138. Subtelny, JD, Sakuda, M. Open bite diagnosis and treatment. Am J Orthod. 1964; 50:337–358.
139. Swinehart, EW. A clinical study of open-bite. Am J Orthod. 1942; 28:18–34.
140. Throckmorton, G, Finn, R, Bell, W. Biomechanics of differences in lower face height. Am J Orthod. 1980; 77:410–420.
141. Trouten, JC, Enlow, DH, Rabine, M, et al. Morphologic factors in open-bite and deep-bite. Angle Orthod. 1983; 53:192–211.
142. Turvey, TA, Journot, V, Epker, BN. Correction of anterior open-bite deformity: A study of tongue function, speech changes and stability. J Maxillofac Surg. 1976; 4:93.
143. Turvey, TA, Hall, DJ, Fish, LC, Epker, BN. Surgical-orthodontic treatment planning for simultaneous mobilization of the maxilla and mandible in the correction of dentofacial deformities. Oral Surg Oral Med Oral Pathol. 1982; 54:491.
144. Turvey, TA, Hall, DJ, Warren, DW. Alterations in nasal airway resistance following superior repositioning of the maxilla. Am J Orthod. 1984; 85:109.
145. Tweed, CH. Clinical orthodontics. St. Louis: Mosby; 1966.
146. Valera, FC, Travitzki, LV, Mattar, SE, et al. Muscular, functional and orthodontic changes in preschool children with enlarged adenoids and tonsils. Int J Pediatr Otorhinolaryngol. 2003; 67:761.
147. Vargervik, K, Mill, AJ, Chierici, G, et al. Morphologic response to changes in neuromuscular patterns experimentally induced by altered mode of respiration. Am J Orthod. 1984; 85:115–124.
148. Verdi, GD, Alpert, B. Correction of the long face: Case report. Plast Reconstr Surg. 1978; 62:613.
149. Weinberg, H, Kronman, JH. Orthodontic influence upon anterior face height. Angle Orthod. 1966; 36:80–88.
150. Wenzel, A, Henriksen, J, Melsen, B. Nasal respiratory resistance and head posture: Effect of intra-nasal corticosteroid (Budesonide) in children with asthma and perennial rhinitis. Am J Orthod. 1983; 84:422–426.
151. Wertz, R, Dreskin, M. Midpalatal suture opening, a normative study. Am J Orthod Dentofacial Orthop. 1977; 71:367.
152. West, RA, Epker, BN. Posterior maxillary surgery: Its place in the treatment of dentofacial deformities. J Oral Surg. 1972; 30:562.
153. West, RA, McNiell, RN. Maxillary alveolar hyperplasia, diagnosis and treatment planning. J Maxillofac Surg. 1975; 3:239.
154. Westermark, AH, Bystedt, H, von Konow, L, Sällström, KO. Nasolabial morphology after Le Fort I osteotomies. Int J Oral Maxillofac Surg. 1991; 20:25–30.
155. Wickwire, NA, White, RP, Proffit, WR. The effect of mandibular osteotomy on tongue position. J Oral Surg. 1972; 30:184.
156. Wylie, WL, Johnson, EL. Rapid evaluation of facial hyperplasia in the vertical plane. Angle Orthod. 1952; 22:165–182.
157. Xun, C, Zeng, X, Wang, X. Microscrew anchorage in skeletal anterior open-bite treatment. Angle Orthod. 2007; 77:47–56.
158. Yao, CC, Lee, JJ, Chen, HY. Maxillary molar intrusion with fixed appliances and mini-implant anchorage studied in three dimensions. Angle Orthod. 2005; 75:754–760.


