CHAPTER 38 Local Flaps for Tuberous and Asymmetric Breasts
Key Points
Summary
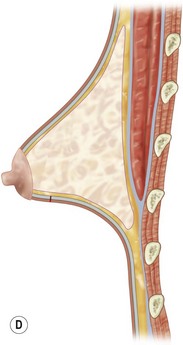
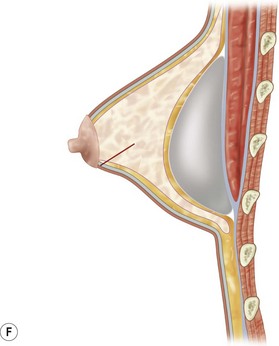
In this chapter I will consider only the ‘heavily hypoplastic tuberous breast.’
Many surgical techniques have been described to best treat these malformations1–20 but none of them, in my opinion, seem to be perfectly applicable to each case and to each different morphological anomaly.
I have developed a new ‘basic idea’ which can be tailored to fit each clinical case.
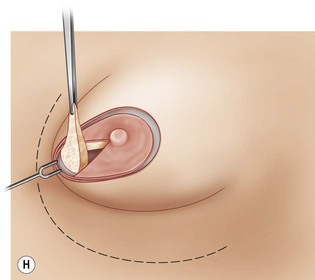
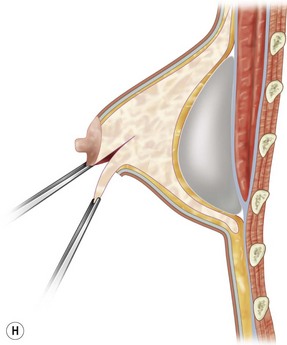
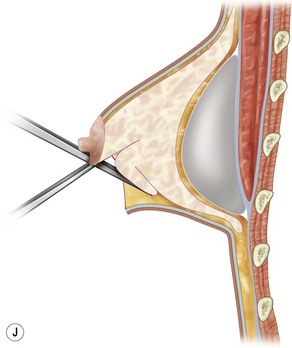
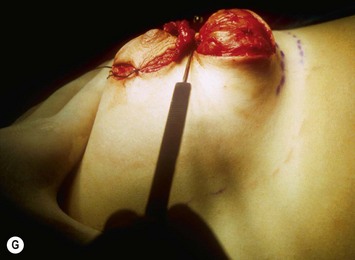
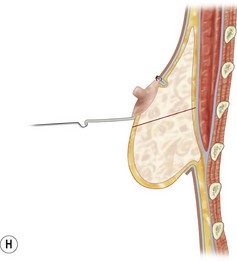
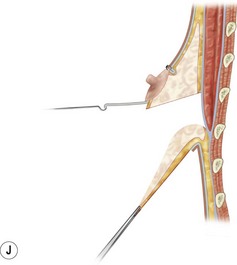
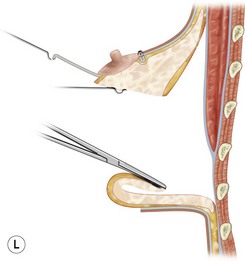
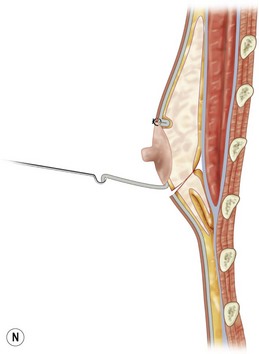
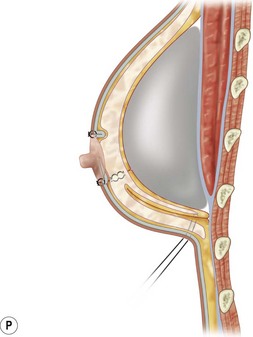
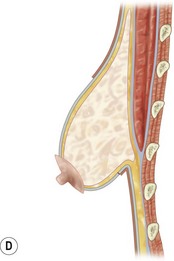
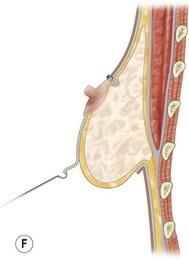
The flaps need to be long enough to reach the pectoralis muscles once the fibrotic constriction of the breast base is released. This constriction often needs to be released by radial and transverse incisions from the deep surface as described by Aston and Rees,14 and Maxwell.9
Patient Selection and Indications
Basically I distinguish three different types of flaps that can fit different types of deformities:
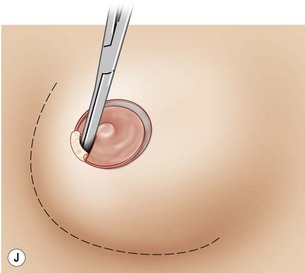
Operative Technique
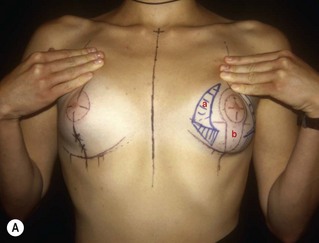
Markings
The fundamental points on the breast are marked as follows:
After the preoperative skin markings are drawn, two other important points must be considered:
Intraoperative preparation
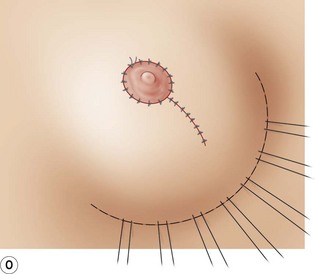
Some temporary tacking stitches are usually needed to control the results and the symmetry.
Surgical steps
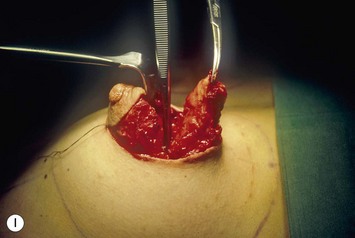
The most common steps of the operative technique can be summarized as follows:
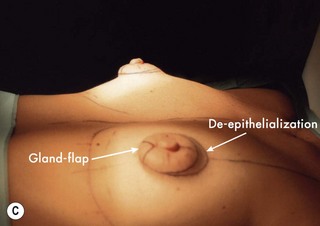
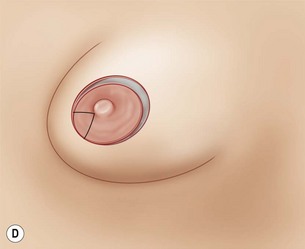
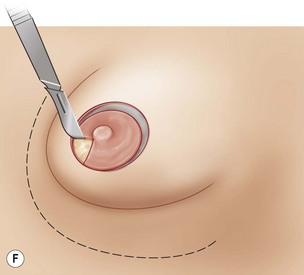
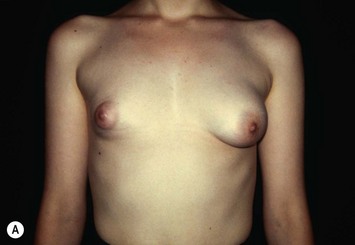
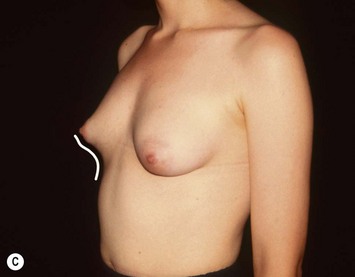
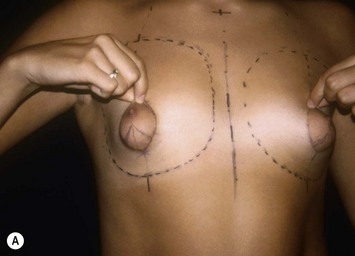
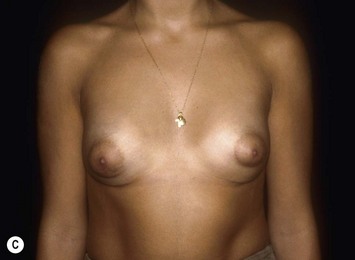
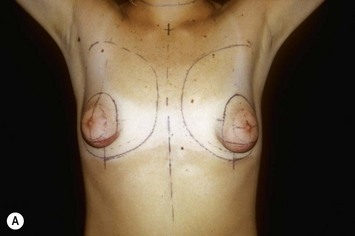
Hypoplastic tuberous breast deformity (Cases 1–3)
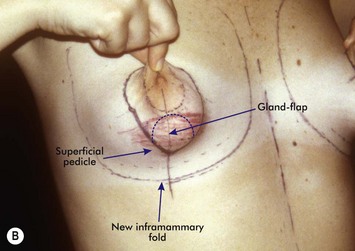
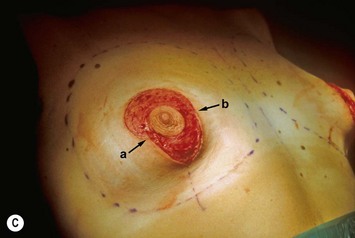
The high morphological complexity of this malformation and its multiple details must be individually considered in approaching surgical repair. This makes it difficult, almost impossible, to describe one complete step-by-step operative sequence for its correction. I have illustrated three different surgical cases presenting different morphological characteristics and the relative intraoperative sequences and drawings (Case 1, Fig. 38.1; Case 2, Fig. 38.2; Case 3, Fig. 38.3).
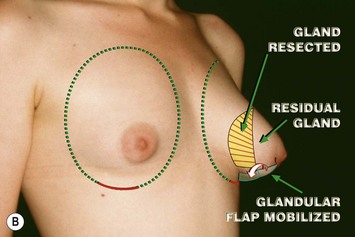
Asymmetric tuberous breast deformity (Cases 4–6)
I have called the following procedure ‘selective subcutaneous gland excision.’
1 Mandrekas AD, Zambacos GJ, Anastasopoulos A, Hapsas D, Lambrinaki N, Ioannidou-Mouzaka L. Aesthetic reconstruction of the tuberous breast deformity. Plast Reconstruct Surg. 2003;112(4):1099-1108.
2 Bass U. Herniated areola complex. Ann Plast Surg. 1978;1:203.
3 Bruck HG. Hypoplasia of the lower medial quadrant of the breast. Aesth Plast Surg. 1992;16:228-238.
4 Choupina M, et al. Tuberous breast: a surgical challenge. Aesth Plast Surg. 2002;26:50-53.
5 Dinner M, Dowden R. The tubular-tuberous breast syndrome. Ann Plast Surg. 1987;19:414-420.
6 Elliot MP. A muscle-cutaneous transposition flap: mammaplasty for correction of the tuberous breast. Ann Plast Surg. 1988;20:153-157.
7 Gasperoni C, Salgarello M, Gargani G. Tubular breast deformity: a new surgical approach. Eur J Plast Surg. 1987;9:141.
8 Longacre JJ. Correction of the hypoplastic breast with special reference to reconstruction of the ‘nipple type breast’ with local dermo-fat pedicle flaps. Plast Reconstr Surg. 1954;14:431.
9 Maxwell P. Breast asymmetry. Aesth Surg. 2001;21:552-561.
10 Mottura AA. Circumvertical reduction mastoplasty; new considerations. Aesth Plast Surg. 2003;27:85-93.
11 Muti E. Personal approach to surgical correction of the extremely hypoplastic tuberous breast. Aesth Plast Surg. 1996;20:385-390.
12 Persichetti P, Cagli B, Tenna S, Simone P, Marangi GF, Li Vecchi G. Decision making in the treatment of tuberous and tubular breast: volume adjustment as a crucial stage in the surgical strategy. Aesth Plast Surg. 2005;29:1-7.
13 Pucket CL, Concannon J. Augmenting the narrow-based breast: the unfurling technique to prevent the double bubble deformity. Aesth Plast Surg. 1990;14:15-19.
14 Rees T, Aston S. The tuberous breast. Clin Plast Surg. 1976;3:339.
15 Ribeiro L, Canwi W, Buss A, Accorsi A. Tuberous breast: a new approach. Plast Reconstr Surg. 1998;101:42.
16 Teimourian B, Menhdi N. Surgical correction of the tuberous breast. Ann Plast Surg. 1983;10:190-193.
17 Toranto R. Two-stage correction of tuberous breast. Plast Reconstr Surg. 1981;67:642-645.
18 Vecchione TR. A method for recontouring the Domes nipple. Plast Reconstr Surg. 1976;57:30-32.
19 Versaci AD, Rozzelle AA. Treatment of tuberous breast utilizing tissue expansion. Aesth Plast Surg. 1991;15:307-312.
20 Williams G, Hoffman S. Mammoplasty for tubular breast. Aesth Plast Surg. 1981;5:51-56.