Chapter 10 Liver, Gall Bladder and Pancreas
Liver – Anatomy
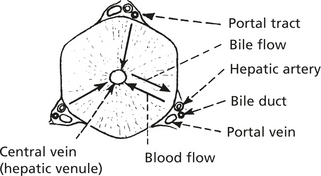
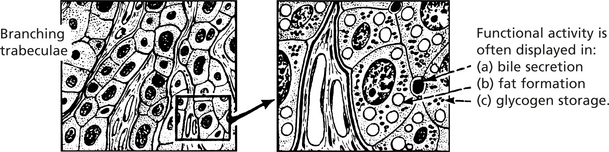
Conventionally the liver was considered to be composed of regular lobules, each arranged around a ‘central vein’ with portal tracts at the periphery.
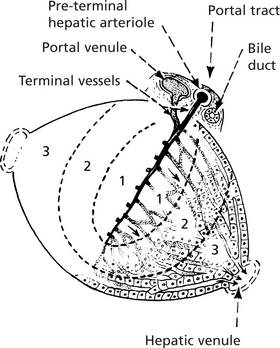
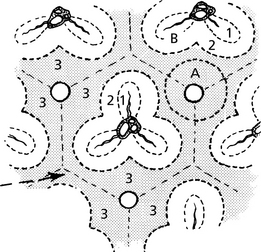
The acinar concept is now used.
The smallest unit is the simple acinus.
In terms of oxygen supply and other nutrients, 3 zones exist.
Anatomy – Hepatic Lesions
Adjacent liver acini form a complex architecture best appreciated when diseases affect the varying zones. Factors involved in this include the pO2 of blood and enzyme function of the zones.
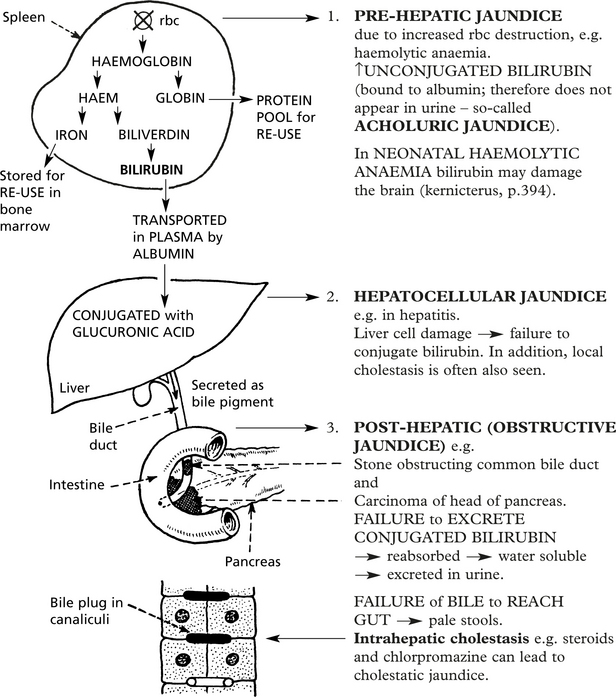
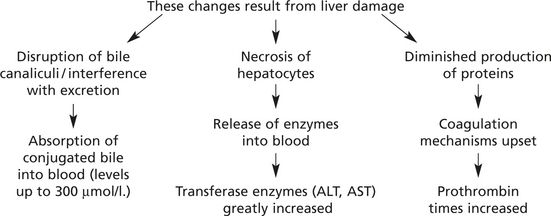
Jaundice
If the serum bilirubin level exceeds 50 μmol/l, the patient becomes jaundiced.
Study of haemoglobin catabolism shows 3 main forms of jaundice:
Viral Hepatitis
Acute Viral Hepatitis
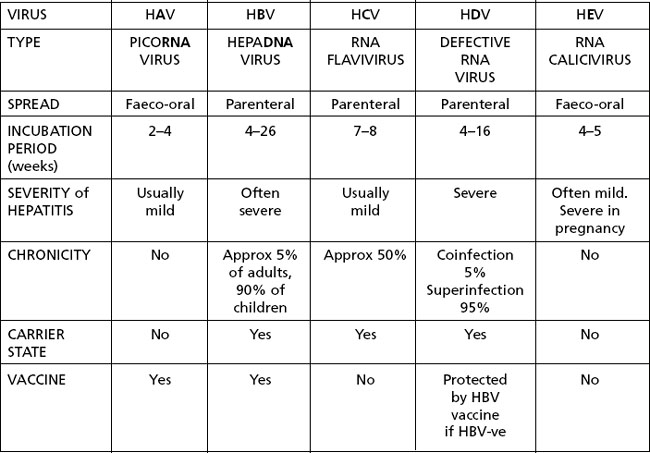
Viral hepatitis is the most important form of hepatitis. It is seen worldwide. Viral hepatitis may be sporadic or epidemic and, depending on the responsible virus, transmitted by the faeco-oral or parenteral route.
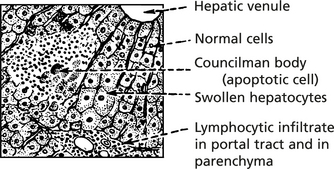
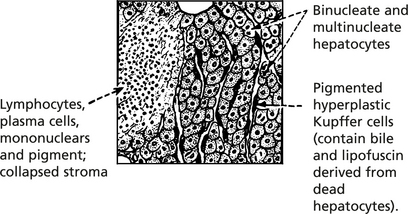
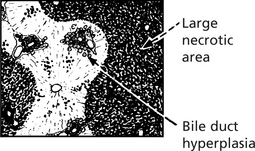
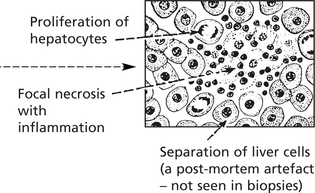
Pathological Features
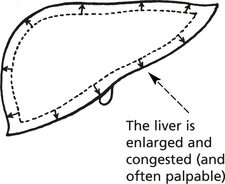
Liver cell necrosis is always present. It is most marked in Zone 3 (p.338).
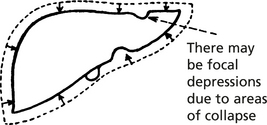
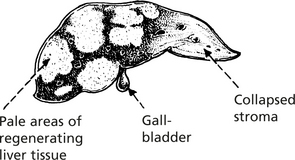
Liver is smaller, yellow or greenish
There is evidence of healing with mitotic activity in the hepatocytes.
Clinical Progress
Remaining liver tissue opaque, yellowish, without markings and is largely necrotic
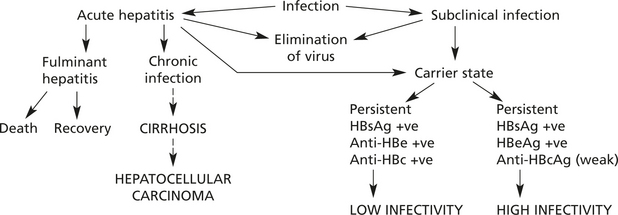
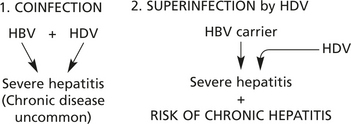
At least 5 viruses cause liver damage without significantly damaging other tissues (hepatitis A,B,C,D and E). The features are summarised and then discussed individually.
Other viruses which can affect the liver, but also affect other tissues include:
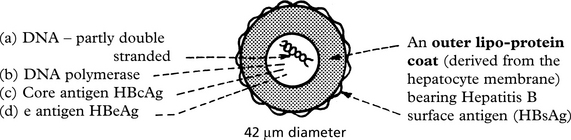
Hepatitis B Infection
The hepatitis B virus is a member of the HEPA DNA virus group. Infection is by the parenteral route – mainly IV drug abuse, blood products and sexual transmission, and in high prevalence areas in childbirth.
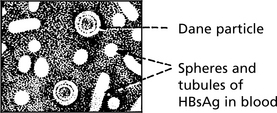
The virus has several components:
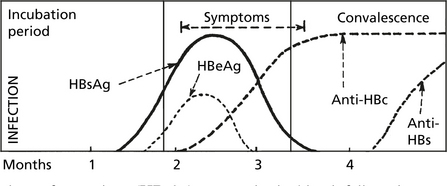
These antigens and antibodies to them are the basis for diagnosis of hepatitis B infection.
HBsAg accumulates in the cytoplasm of cells – giving a ‘ground glass’ appearance.
or can be stained by immunocytochemistry.
Serology: Antibodies to the various antigens appear in the blood.
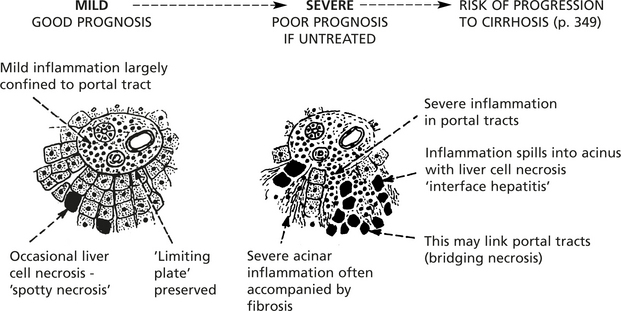
Chronic Hepatitis
Inflammation of the liver which lasts for more than 6 months is regarded as chronic. (This definition excludes disorders such as alcoholic hepatitis.)
Histologically, three areas of inflammation are seen to varying degrees.
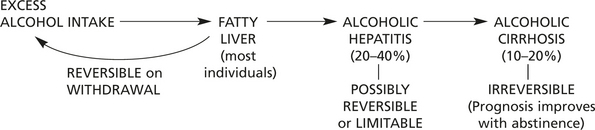
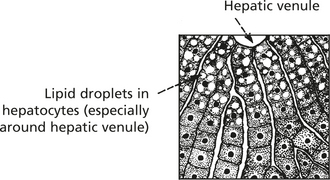
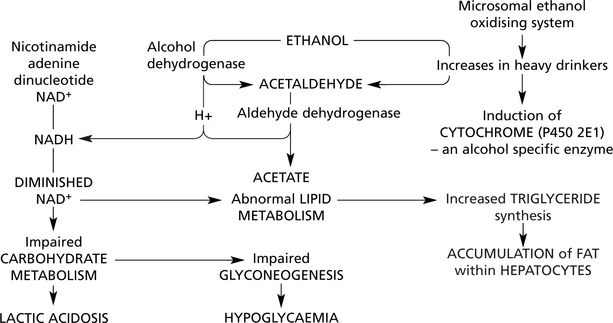
Alcoholic Liver Disease
Excess consumption of alcohol is associated with liver disease in three main forms.
Alcoholic Hepatitis
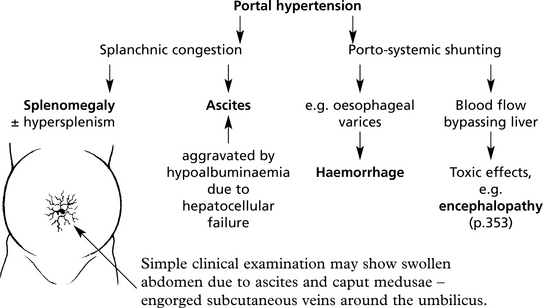
In 20–40% of heavy drinkers, alcoholic hepatitis is superimposed on fatty change. This varies from asymptomatic hepatitis to a life threatening condition with nausea, vomiting, abdominal pain and jaundice. Signs of liver failure and portal hypertension may be found.
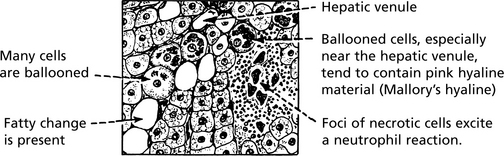
Histologically, the main features are seen around hepatic venules:
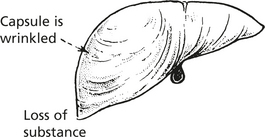
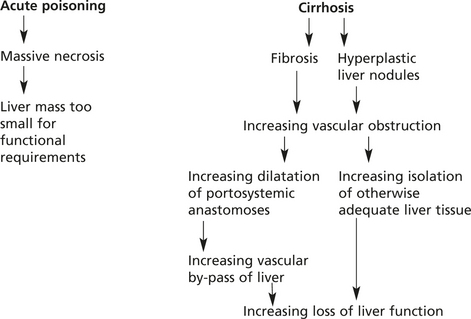
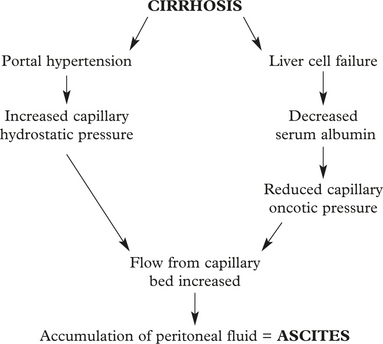
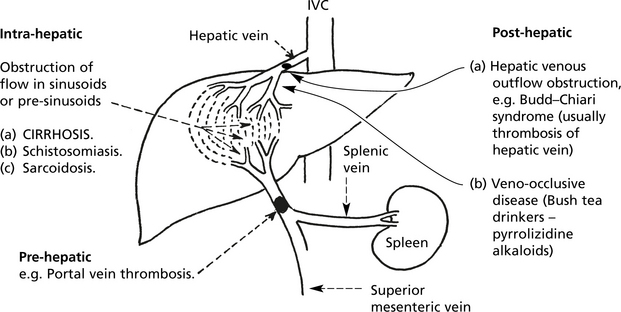
Cirrhosis
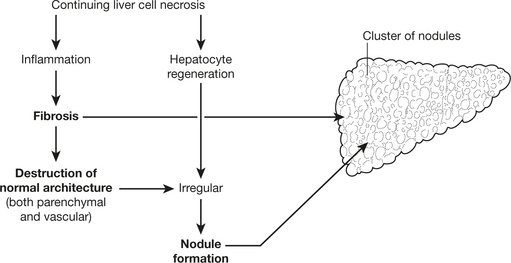
Cirrhosis is the end stage of many liver diseases. It is defined as:
Cirrhosis
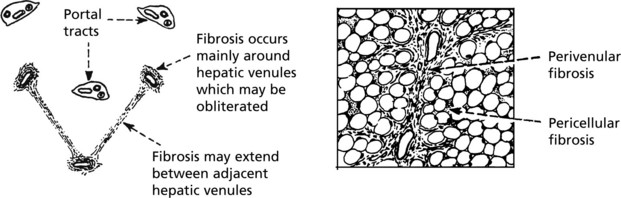
The initiating factor in the progression to cirrhosis is continuing hepatocellular damage. Its location within the acinus (p.338) and also its cause are reflected in the progression to irreversible damage.
Biliary Disease
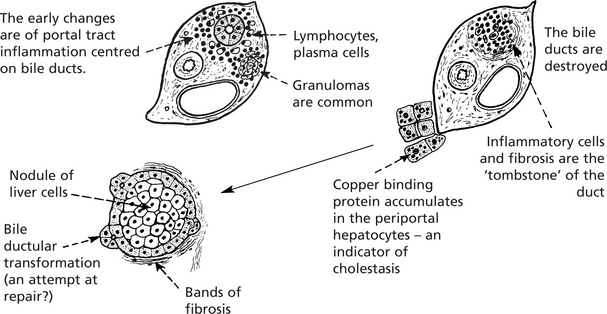
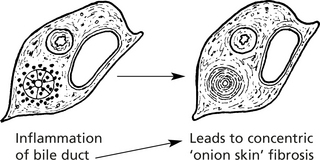
Primary Biliary Cirrhosis (PBC)
This is a chronic disorder mainly affecting middle-aged women. Destruction of intra-hepatic bile ducts leads to scarring and eventually to cirrhosis. Patients typically present with fatigue, itching (from bile salt retention) or jaundice. Hyperlipidaemia is common.
Hepatocellular Failure
Failure of Liver Function can be:
The mechanism is different in the 2 types.
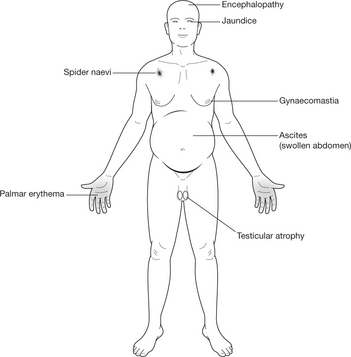
The cardinal signs of hepatocellular failure are:
Other features include hypoglycaemia, acidosis and endocrine disturbances.
Hepatocellular Failure
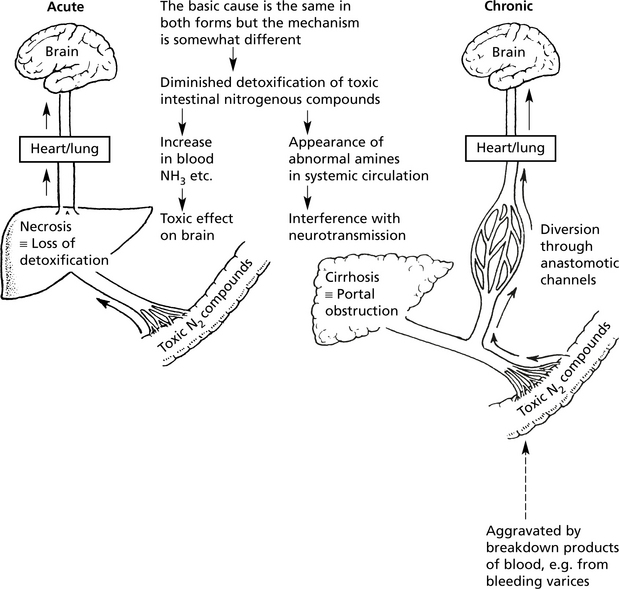
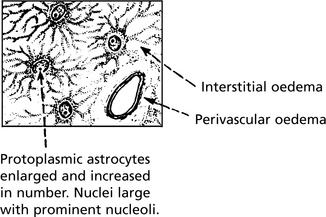
Hepatic Encephalopathy
This term refers to the impaired mental state and neurological function due to liver failure. It takes the form of tremors, behavioural changes, convulsions, delirium, drowsiness and coma. In the acute form, severe symptoms such as convulsions, delirium and coma develop rapidly, while in chronic conditions milder changes are seen and coma is a late feature, unless a complication arises.
Metabolic Disorders and the Liver
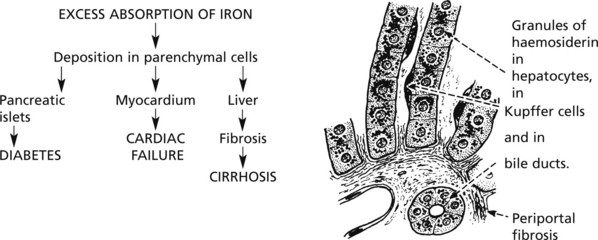
Haemochromatosis
Almost all cases are due to a mutation on chromosome 6, encoding the HFE protein which regulates iron absorption.
Although heterozygotes absorb excess iron, only homozygotes develop the disease.
Infections
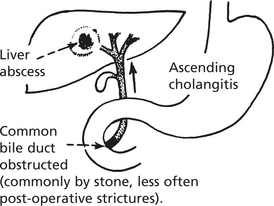
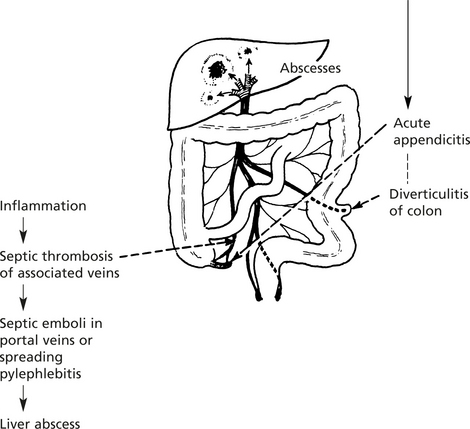
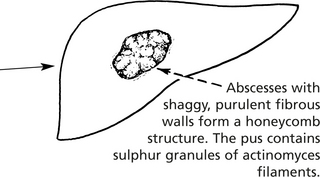
Pyogenic Infections
These are now much less common due to the use of antibiotics. Abscess of the liver, usually due to coliforms, occurs mainly in two conditions:
Infections
Spirochaetal Infections
Three spirochaetal infections can involve the liver.
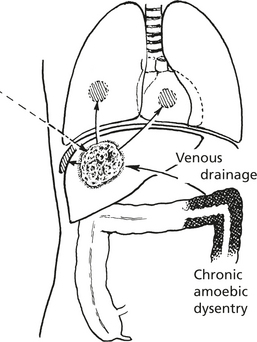
Protozoal Diseases
Amoebic ‘Abscess’
This is a complication of amoebic dysentery due to Entamoeba histolytica. The ‘abscess’ is usually single, in the upper right lobe of liver. An irregular fibrous wall encloses off necrotic liver cells, debris and red cells. Amoebae may be found in the inner wall. It may remain localised or track through the diaphragm into the lung, pleural or pericardial cavities.
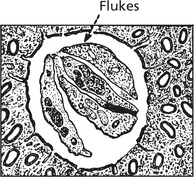
Metazoal Diseases Trematodes (Flukes)
Schistosomiasis (Bilharzia)
Two other varieties of fluke disease exist — clonorchiasis (Chinese fish fluke) and fascioliasis (sheep fluke). Both produce an ascending cholangitis. Clonorchiasis can cause biliary obstruction and marked proliferation of bile ducts. Cholangiocarcinoma may develop. Infestation in both cases is due to eating raw or undercooked food.
Tumours of the Liver
Primary Benign Tumours
Primary Carcinoma of Liver
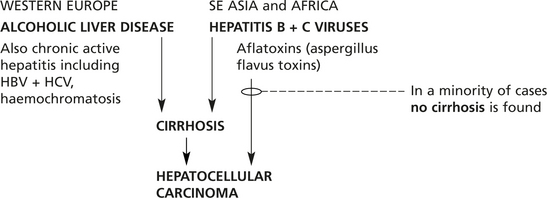
Hepatocellular Carcinoma (HCC)
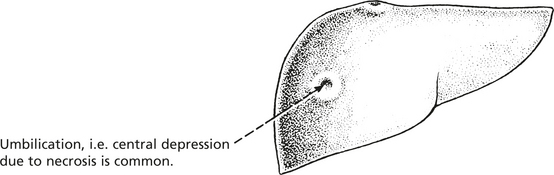
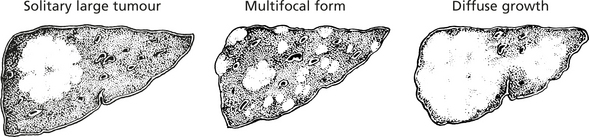
This, the commonest primary malignancy of the liver, is unusual in Western Europe, but is very common in Africa and South-East Asia. Males are particularly affected.
Three main types of growth are described:
In all three forms the liver is often cirrhotic (80%) (particularly in the West).
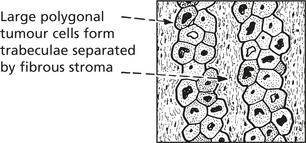
Histological structure: The cells grow in columns resembling normal liver.
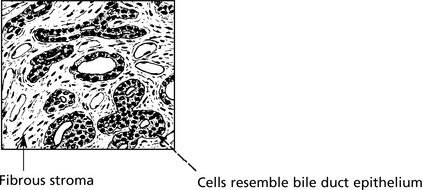
Primary Liver Cell Tumours
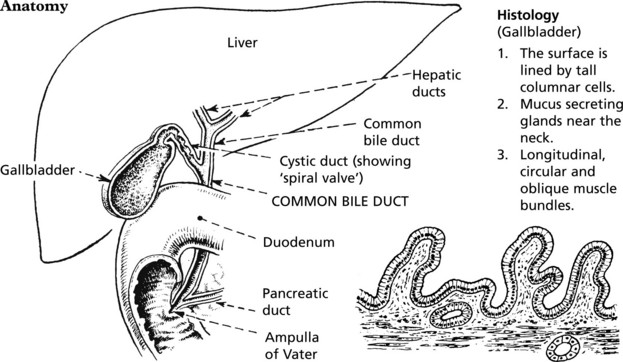
Gallbladder And Bile Duct – Anatomy
The function of the gallbladder is to concentrate and store bile.
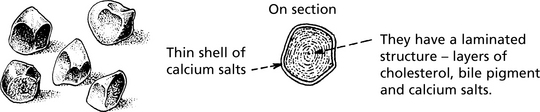
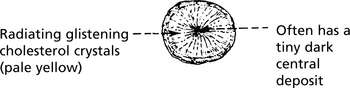
Gallstones
Gallstones are the principal cause of gallbladder disease and its consequences.
Gallstones
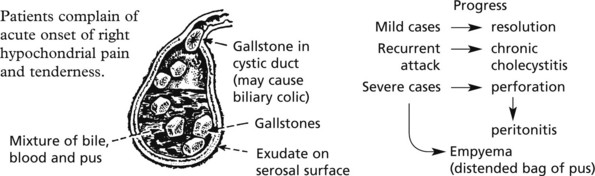
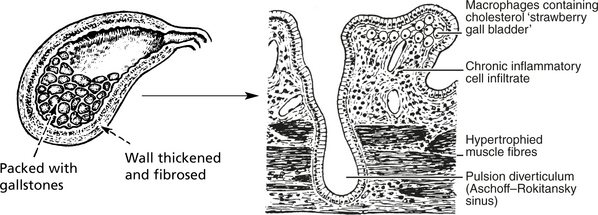
Clinical Manifestations and Complications
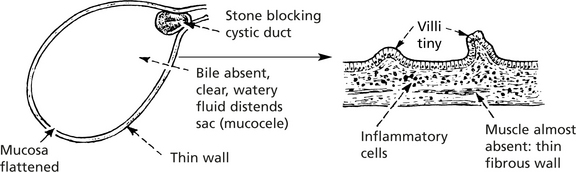
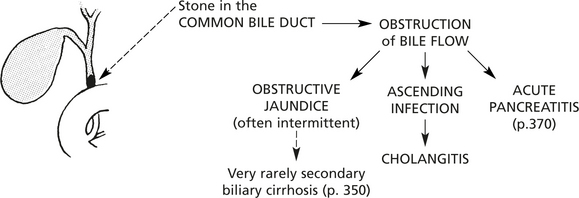
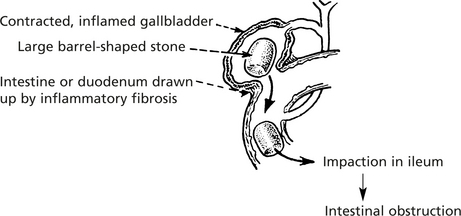
Many patients are asymptomatic or have only mild dyspepsia; others develop symptomatic complications.
This occurs when there has been long-standing obstruction of the cystic duct.
Note: In addition to jaundice, persistent skin itching, due to retention of bile salts, may occur.
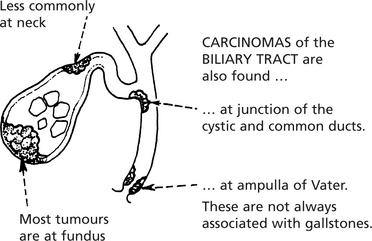
Gallstones – Aetiology
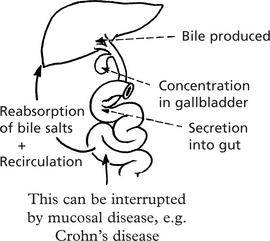
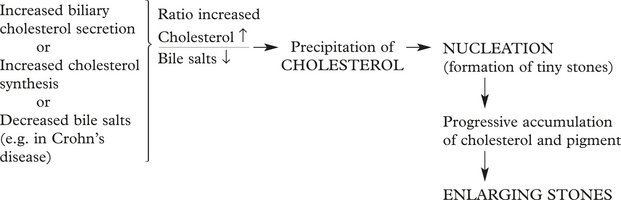
Although gallstones are found in 10–20% of the population, the prevalence increasing with age, the exact mechanisms of their formation remain incompletely understood. Risk factors include (a) female gender, (b) obesity, (c) pregnancy, (d) drugs such as the cholesterol lowering drug clofibrate now seldom used and (e) gastrointestinal disease, e.g. Crohn’s disease.
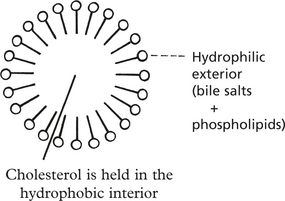
The stability of cholesterol depends on adequate amounts of bile acids. Micelles are formed.
Their enterohepatic circulation is essential to maintain adequate concentrations of bile salts.
The ratio of cholesterol:bile salts is very important.
Stones often lead to infection: it is likely that infection promotes further stone production.
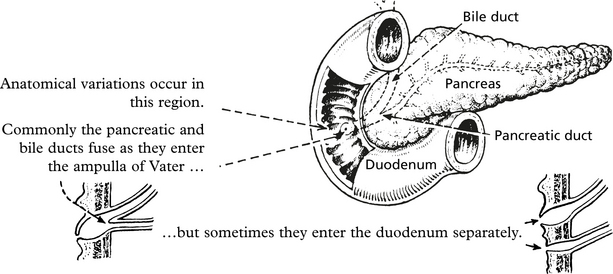
Pancreas
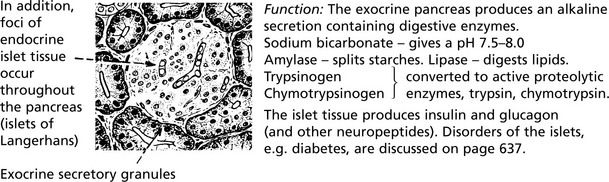
The exocrine glandular portion of the pancreas produces digestive secretions which are released into the second part of the duodenum.
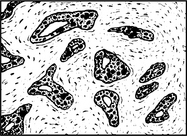
Microscopically, the exocrine tissue is similar to salivary glands.
Acute Pancreatitis
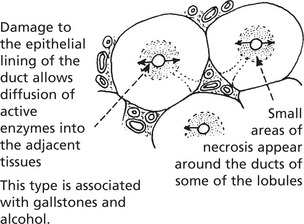
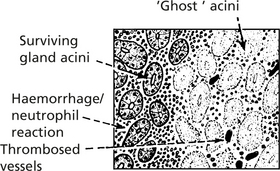
Early changes are seen in centre of the lobules.
Periductal necrosis – in the centre of each affected lobule.
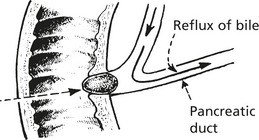
This type is associated with gallstones and alcohol.
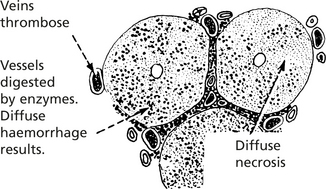
Panlobular Pancreatitis
Release of enzymes beyond the pancreas gives fat necrosis of the omentum.
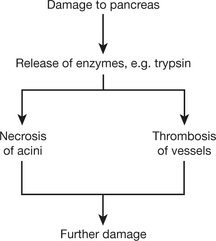
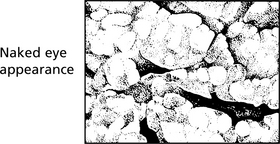
In acute pancreatitis, acute inflammation is associated with necrosis of pancreatic acini and fat.
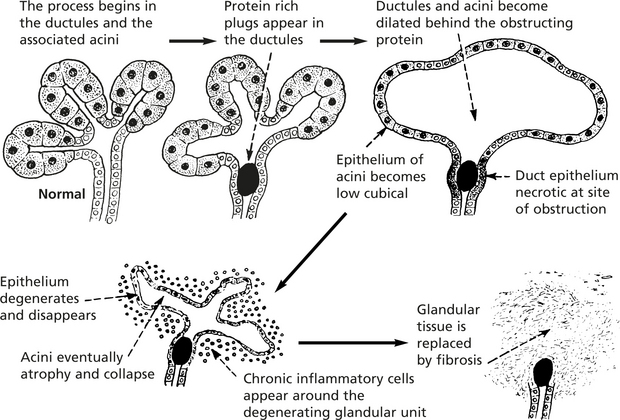
Chronic Pancreatitis
Chronic pancreatitis predominantly affects alcoholics.
Ultimately, a large proportion of the exocrine tissue is destroyed.
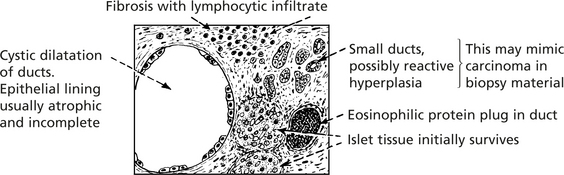
With progress of the disease, two other developments take place:
Rupture into the peritoneal cavity causes ascites, frequently haemorrhagic.
Effects
Patients typically complain of abdominal pain.
Apart from the complications due to cyst rupture, destruction of pancreatic tissue may lead to:
Aetiology
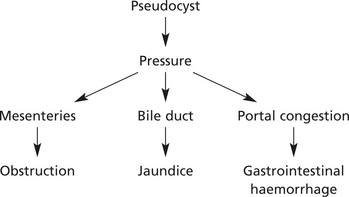
Cystic Fibrosis (Mucoviscidosis)
This is a common autosomal recessive inherited disease due to genetic mutation on chromosome 7; a high percentage (about 4%) of the population are carriers.
Tumours of Pancreas
Benign tumours of the pancreas such as cystadenomas are rare. They may produce symptoms due to pressure on other structures.
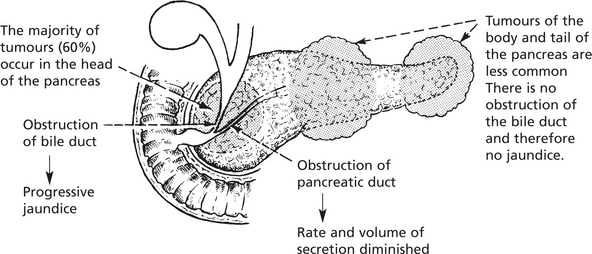
Carcinoma
Thrombosis of unknown cause and at distant sites (thrombophlebitis migrans, p. 236), e.g. femoral vein, may occur.