Liver function tests
Introduction
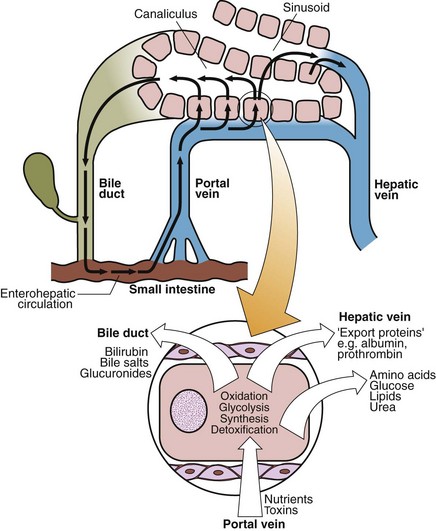
The liver plays a major role in protein, carbohydrate and lipid homeostasis (Fig 28.1). The metabolic pathways of glycolysis, the Krebs cycle, amino acid synthesis and degradation, and the processes of oxidative phosphorylation are all carried out in the hepatocytes, which are well endowed with mitochondria. The liver contains an extensive reticuloendothelial system for the synthesis and breakdown of blood cells. Liver cells metabolize, detoxify and excrete both endogenous and exogenous compounds. Excretion of water-soluble end products from the metabolism of both nutrients and toxins, and of digestive aids such as bile acids, occurs into the biliary tree.
Liver function tests
Bilirubin
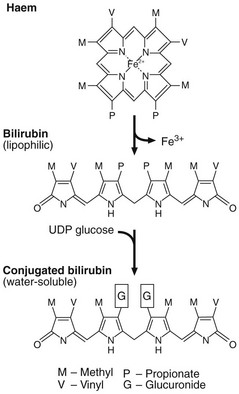
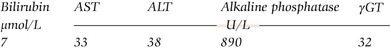
Bilirubin is derived from haem, an iron-containing protoporphyrin mainly found in haemoglobin (Fig 28.2). An adult normally produces about 450 µmol of bilirubin daily. It is insoluble in water and is transported in plasma almost totally bound to albumin. It is taken up by liver cells and conjugated to form mono- and diglucuronides, which are much more soluble in water than unconjugated bilirubin. The conjugated bilirubin is excreted into the bile. Normal bile contains bilirubin monoglucuronide as 25% and the diglucuronide as 75% of the total, accompanied by traces of unconjugated bilirubin. The main functional constituents of the bile are the bile salts, which are involved in fat digestion and absorption from the small intestine. Serum bile acid concentrations are more sensitive indices of hepatic transport function than are total bilirubin measurements.
When the biliary tract becomes blocked, bilirubin is not excreted and serum concentrations rise. The patient becomes jaundiced. The jaundiced patient is described further on pages 58–59.
The aminotransferases (AST and ALT)
The activities of two aminotransferases, AST and ALT, are widely used in clinical practice as a sensitive, albeit non-specific, index of acute damage to hepatocytes irrespective of its aetiology. Causes of liver damage include hepatitis, no matter the causative agent, and toxic injury, which may accompany any one of a large number of insults to the liver, including drug overdose. Acute liver damage due to shock, severe hypoxia and acute cardiac failure is also seen (see pp. 60–61).
Plasma proteins
Alpha-fetoprotein (AFP) is synthesized by the fetal liver. In normal adults it is present in plasma at low concentrations (<3 kU/L). Measurement of AFP is of value in the investigation of hepatocellular carcinoma in which serum concentrations are increased in 80–90% of cases. AFP is also used as a marker for germ cell tumours (pp. 140–141).
Other proteins, such as α1-antitrypsin and caeruloplasmin, are measured in the diagnosis of specific diseases affecting the liver (p. 61).