5 Liver and Biliary Tract Disorders
Abnormal liver biochemistry
‘Liver function tests’ are routinely requested.
The doctor asks: would an ultrasound be helpful?
No. This is not the pattern of biliary or pancreatic disease.
On examination you notice a few spider naevi. The liver is not palpable.
The results of the tests performed by the doctor are now available (Table 5.1). HCV antibodies indicate HCV infection (chronic hepatitis) and the patient will require HCV RNA, liver biopsy and possible treatment with anti-viral therapy with pegylated interferon and ribavirin, or with one of the newer protease inhibitors (boceprevir or telaprevir).
Table 5.1 Further investigations into the cause of the abnormal liver function test
| Test | Result | Implication |
|---|---|---|
| Repeat LFTs | Similar to above | |
| Hepatitis A | IgG positive IgM negative |
Patient has been infected with HAV in the past or immunised. This virus does not cause chronic liver disease |
| HBsAg | Negative | See below |
| HCV antibodies | Positive | |
| Autoantibody screen | Negative | Positive titres usually found in autoimmune hepatitis |
| Serum ferritin | 110 µg/L | This excludes hereditary haemochromatosis |
Although this patient did not have HBV, you need to know the significance of HBV markers (Table 5.2).
Table 5.2 Significance of viral markers in hepatitis B
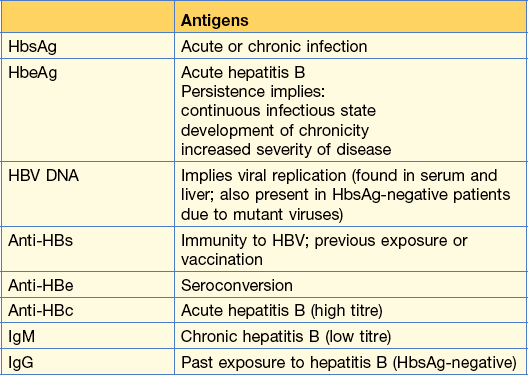
From Kumar and Clark Clinical Medicine, 8th edn, 2012.
Jaundice
Jaundice is detected clinically when the serum bilirubin is greater than 50 µmol/L (3 mg/dL).
Case history (1)
Abdominal examination is unhelpful; there were no signs of chronic liver disease.
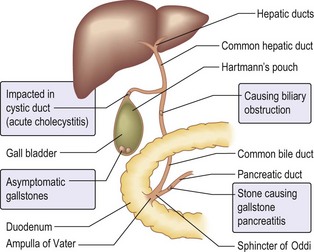
The blood tests showed a raised serum bilirubin, an ALT of 50 units and a high alkaline phosphate of 410 units. You order an ultrasound examination of the liver and biliary tree as you suspect that she has got gallstone disease (Fig. 5.1).
Ultrasound in extra-hepatic obstruction can show:
• Dilatation of the intra-hepatic biliary tree
• Dilatation of the common bile duct
• Gallstones in the gall bladder
In this patient, the ultrasound showed gallstones in the gall bladder and a dilated common bile duct. Provided this patient’s clotting is satisfactory, the next procedure should be an ERCP. This would enable a better visualisation of the system and would allow a gallstone that is causing the obstruction in the common bile duct to be removed. A sphincterotomy would need to be performed beforehand and the stone could be removed with a basket or a balloon. If the stone is very large, the stone can be crushed and the debris removed. In an elderly patient, stent insertion to maintain drainage is an option.
Acute liver disease
How do you approach this situation?
On examination, apart from jaundice, there are no other abnormal signs.
You tell him to go back to his student flat, be careful with his personal hygiene and return in 2 days for his results (Table 5.3).
| Test | Result | Implication |
|---|---|---|
| Serum bilirubin | 70 µmol/L | |
| AST | 300 iu/L | Compatible with acute |
| ALT | 280 iu/L | hepatitis |
| ALP | 140 iu/L | |
| HAV IgM | Negative |
Ascites
Case history (1)
A 45-year-old woman presents with ascites gradually increasing over 2 weeks.
Information
Paracentesis (ascitic tap):
Ascitic fluid
In this case, a high ascitic protein (> 25 g/L) suggests tumour or infection.
What should you do?
An ascitic tap is necessary to rule out infection and malignancy, even though he has chronic liver disease.
Immediate management
• Start diuretics – spironolactone 100 mg/day (increasing gradually to 400 mg/day) to obtain a weight loss of 500 g/day
• If inadequate response to above, introduce furosemide 40–120 mg/day
The patient must stop drinking.
Haematemesis and melaena
Resuscitation
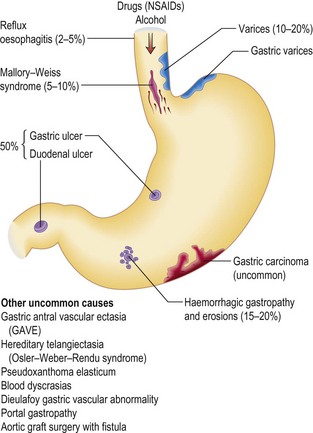
Many hospitals have multidisciplinary teams and protocols. Keep the patient nil by mouth until the bleeding has stopped. Causes of upper gastrointestinal bleeding are shown in Figure 5.2.
Management
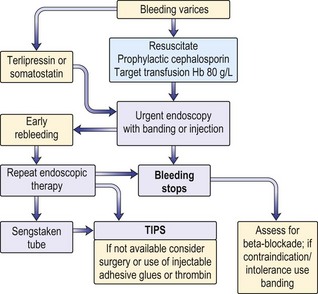
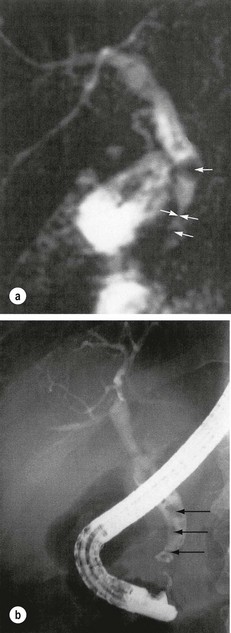
His haemoglobin returned as 90 g/L and the urea was raised at 10 mmol/L. A blood transfusion was started to resuscitate him (Fig. 5.3). On improvement he had an endoscopy which showed oesophageal varicies and these were banded (Fig. 5.4). On return to the ward he had a further haematemesis 4 hours later. Vasoconstrictor therapy was given.
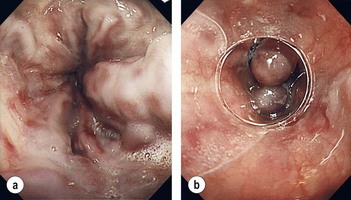
Figure 5.4 Oesophageal varicies (a), with band in place (b).
(Kumar and Clark Clinical Medicine 8th edn, 2012, p. 333).
Vasoconstrictor therapy
• Terlipressin. This is the only vasoconstrictor shown to reduce mortality. Dose is 2 mg 6-hourly, reducing to 1 mg 4-hourly after 48 hours if a prolonged dosage regimen is used. It should not be given to patients with ischaemic heart disease. The patient will complain of abdominal colic, will defecate and have facial pallor owing to the generalised vasoconstriction.
• Somatostatin. This drug has few side effects. An infusion of 250–500 µg/h appears to reduce bleeding, but has no effect on mortality. It should be used if there are contraindications to terlipressin.
Balloon tamponade with a Sengstaken–Blakemore tube can be used if the bleeding continues. Use the gastric balloon only initially but, if the bleeding is not controlled, inflate the oesophageal balloon, remembering that continuous inflation leads to oesophageal damage. It has serious complications and should be left in situ for only 24 h.
Liver failure
What signs indicate liver failure?
If there is no risk of bleeding, then concentrate on determining the level of encephalopathy:
Early signs should be demonstrated by asking the patient to copy a five-pointed star.
Immediate management
• Measure electrolytes and blood sugar (BS), liver function and liver biochemistry.
• Ascitic tap to rule out infection (p. 64).
• Low protein and low salt diet.
• Establish infusion of 5% glucose (10% if BS is low).
• Diuretic therapy (see ascites).
• Use purgatives: lactulose 10–20 mL × 3/day to produce two to three stools a day.
• Determine presence of infection both in ascites (ascitic tap) and systemically (blood culture) and treat.
Excess alcohol use
This man has two features of excess alcohol consumption.
1. Central findings – Wernicke–Korsakoff syndrome. This is sometimes reversible with parenteral thiamine therapy.
2. Peripheral neuropathy which is usually not reversible on alcohol abstinence or vitamin therapy.
Further treatment
Cholecystitis
What should you do now?
One hour later your house officer phones you to say his WCC is 19 000. Clearly he has an infection and you tell your house officer to organise an urgent ultrasound while you call the surgical registrar. The surgical registrar recognises the patient he discharged 2 days ago. You discuss possible diagnoses. The ultrasound scan (Fig. 5.5) shows: