Chapter 15 Liposuction of upper back/bra rolls
• Liposuction of the upper back and bra rolls can produce excellent outcomes, provided that attention is paid to patient selection and surgical technique.
• Positioning of the patient during surgery is important in order to achieve the best outcome.
• Wetting solution infiltration permits the procedure to be accomplished with the least amount of blood loss and minimizes surgeon fatigue.
• In our experience, there are minimal complications from performing liposuction to the upper back and bra rolls.
• Patients find satisfaction with their outcomes from this treatment, once swelling is resolved.
Anatomical Aspects
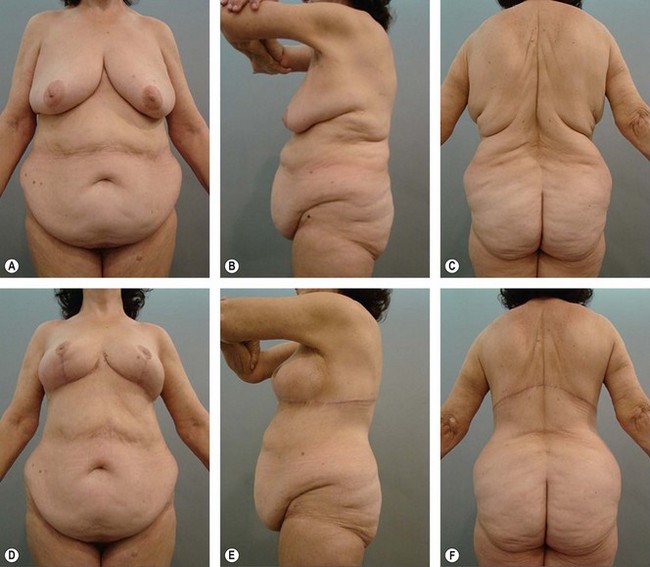
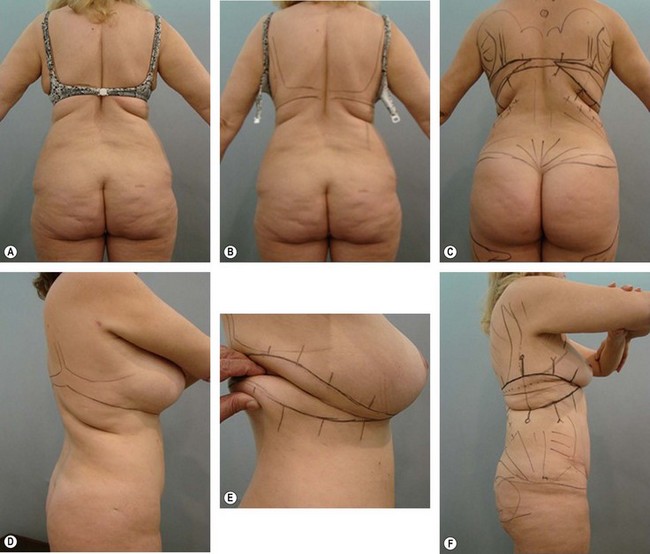
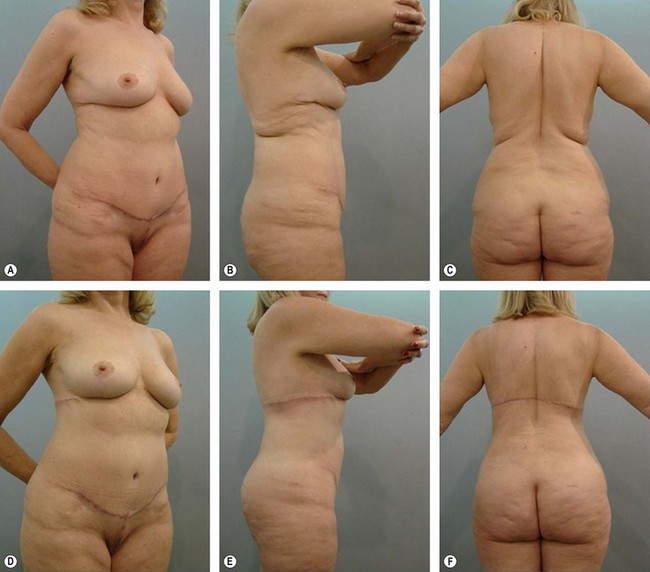
In liposuction the dense connective tissue is very important because it is thicker in the upper back region, especially in the grooves formed by the excess skin that can result from both genetic inheritance (Fig. 15.1), obesity (Fig. 15.2A and D), sagging senile (Fig. 15.3A, B) or post liposuction (see Fig. 15.2 C and F).
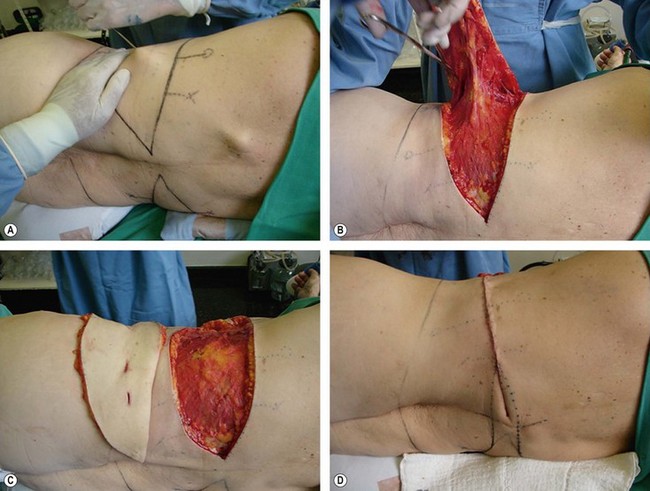
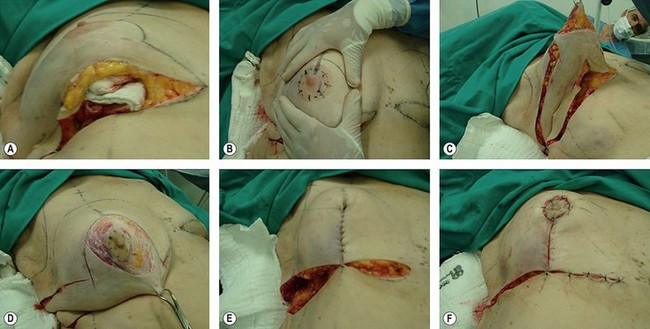
Another important feature is the loose connective tissue (Fig. 15.4B) that grips the skin and subcutaneous muscle (aponeurosis) in this region making it easier to rip of the whole skin and subcutaneous tissue without detaching it surgically during resection flaps (Fig. 15.4C and D).
Surgical Treatment
Planning – Demarcation
Liposuction of the upper back can be performed only by minimal incisions of 5 mm at each subsequent level of the armpits (see Fig. 15.1A and C).
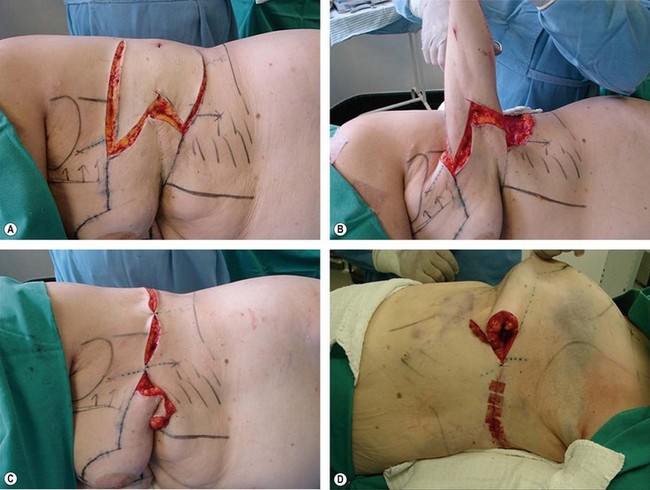
Where it is planned, resection of skin incisions may be made in the flaps (see Fig. 15.4).
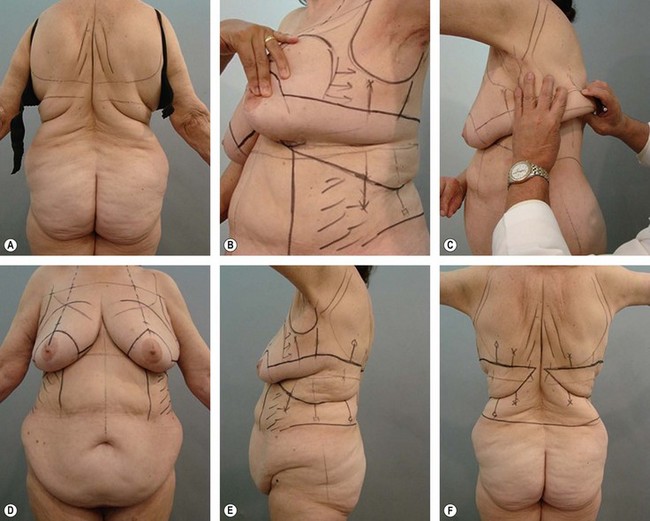
The upper line of resection of the back is marked by pulling down the skin of this region and marking ± 2 cm above the submammary horizontal extension of the line (Fig. 15.5E and 15.8F).
The score line is bound low by the amount of skin which is desirable to withdraw (see Fig. 15.5C and E).
Positioning on the Operation Table
Regardless of the surgeon’s preference for general anesthesia or upper thoracic epidural complemented with axillary local anesthesia, the position on the table may be in the prone or lateral decubitus (see Fig. 15.4A). The latter allows a better approach to the upper back, axillary contour, bra rolls and abdomen.
Surgical Technique
Liposuction is initiated from the deepest layer (lamellar) (see Fig. 15.4A) to the most superficial layer (areolar). It should be aspirated maximally from the lamellar layer, because its larger and turgid cells are still softened by wetting solution infiltration. It will result in a thicker layer of fibrous connective tissue (see Fig. 15.4B), allowing a better grip of this flap and lower recurrence of sagging. The aspiration of the areolar layer is also significant, as it is important for the surgeon to leave the thickness of the tissues according to his preference.
In cases where the skin resection is programmed, liposuction under the flap should be total. Thus, the resection is reduced only to the skin layer, leaving the vascularization and innervation intact. This avoids areas of paresthesia and discomfort, which are sources of complaint from patients (see Fig. 15.4B and C).
Initially, our incisions, whenever possible, extend to the end of the spine area, but we leave markings that allow us to connect the incisions if necessary (see Figs 15.5F, 15.4D and 15.5E).
When indicated, these incisions can be extended to the anterior thorax with reverse resection of the upper abdomen (reverse abdominoplasty) or surgical correction of the breast (Figs 15.6 and 15.7).
Postoperative Care and Results
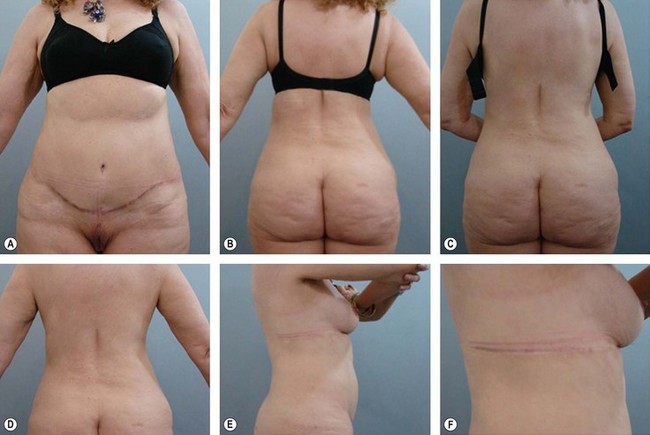
The advantage of skin resection and its applicability is questioned by the occasional widening of scars in patients with thin skin and hypertrophy scars in patients with thicker skin (see Figs 15.3B and 15.10), not excluding the fact that patients with thicker skin may also present scar enlargement.
We limit physical fitness activities for 3 months. This would not impair an early return to work.
Complications
Often liposuction of the back (see Fig. 15.1A and C) is accompanied by liposuction of the hips and sacral region, leaving these regions exposed to occasional fluid collections (seroma).
The risk of skin necrosis is avoided by supporting the operated area with a soft surface and evenly distributing the weight over the entire surface of the patient (see Fig. 15.4A and D).
Conclusion
Reviewing 902 cases of upper back liposuction, there were 23 cases (2.55%) of skin resection concurrent with liposuction of the back (see Fig. 15.2). This argues for very conservative practice, with skin resection reserved for cases of severe pre-existing sagging (Fig. 15.8B–E and C–F), and especially in patients undergoing major weight loss where the skin has already suffered its maximum retraction.
Skin resection of the back has almost a formal indication in these cases and when properly indicated and performed brings great benefits for the patient (Figs 15.9–15.11).
Aly A, Cram A, Chao M, et al. Belt lipectomy for circumferential truncal excess; the university of Iowa experience. Plast Reconstr Surg. 2003;111:398–413.
Avelar JM, Illouz YG. Lipoaspiração, 1st ed. São Paulo: Hipócrates; 1986. p. 45–57
Baroudi R. Body contour surgery. Clin Plast Surg. 1989;16(2):263–277.
Baroudi R. Flankplasty:specific treatment to improve body contouring. Ann Plast Surg. 1991;27(5):404–420.
Illouz YG. Study of subcutaneous fat. Aesth Plast Surg. 1990;14(3):165–177.
Illouz YG. Une nouvelle technique pour les lipodystrophies localisées. Rev Chir Esth France. 6(9), 1980.
Markman B, Barton FE. Anatomy of the subcutaneous tissue of the trunk and lower extremity. Plast Reconstr Surg. 1987;80(2):248–254.
Rohrich RJ, Gosman AA, Conrad MH, et al. Simplifying circumferencial body contouring: the central body lift evolution. Plast Recontr Surg. 2006;118:525.
Souza Pinto EB. Lipoaspiração superficial. Rio de Janeiro: Revinter; 1999. Chapter 3 p. 18–9
Strauch B, Herman C, Rohde C, et al. Mid-body contouring in the post-bariatric surgery patient. Plast Reconstr Surg. 2006;117:2200.
Teimourian B, Gotkin R. Contouring of the midtrunk in overweight patients. Aesth Plast Surg. 1989;13:145–153.
Van Geertruyden JP, Vanderweyer E, de Fontaine S, et al. Circumferential torsoplasty. Br J Plast Surg. 1997;52:623–628.
Van Huizum MA, Roche NA, Hoper SOP. Circular belt lipectomy. A retrospective follow-up study on perioperative complications and cosmetic outcome. Ann Plast Surg. 2005;54:459.