Chapter 19 Liposculpture
Introduction
Liposculpture is a technique used to restore or improve facial and body contouring by removing localized fat deposits with small blunt-tipped cannulas connected in a suction device. This procedure can be associated with injections of the removed autologous adipose tissue where needed.1,2 It is also named as liposuction, lipoplasty, suction lipectomy or suction-assisted fat removal.
The development of liposuction techniques made the autologous fat injection a more reliable procedure. The term liposculpture was initially used by Fournier to describe syringe liposuction associated with fat injection.3 However, considering the etymology of the word ‘liposculpture’, its concept can be extended for all of liposuction techniques because most of these procedures are performed to improve body shape only by removing fat deposits.
Although many authors have reported good results with the use of suction-assisted liposuction, power-assisted liposuction or ultrasonicassisted liposuction.4,5,6 or vibrating cannulas, others support the use of syringe liposculpture,7,8,9 mainly because this technique is precise and promotes less trauma of the adipose tissue. Therefore, this chapter will detail the main liposculpture techniques with special attention for syringe liposculpture.
Considerations About the Adipose Tissue
Adipose tissue is composed by fat cells organized in lobules. Each lobule has its own vascularization. Adipose cells are originated from fibroblast-like cells, called preadipocytes, which develop to become a mature adipose cell. These cells increase in number along childhood and adolescence10
Therefore, the number of cells is constant along adult life. The accumulation of fat occurs by the increase in deposition of the intracellular lipid, not by the increase of number of adipose cells.11,12
Fat cells are extremely delicate, and should be manipulated with special care.13 Therefore, the amount of viable fat cells will depend on the liposuction technique.
Adipose tissue is divided in two layers: the superficial layer and the deep layer. The superficial layer, also named areolar, represents small compact fat lobules that are separated by a greater number of membranes (septa). Its thickness is uniform in all of the body parts. The deep layer is also named reticular or lamellar ayer. In this layer fat lobules present an irregular distribution as well as a small number of membranes (septa) that show an irregular pattern when compared with the superficial layer.14
The accumulation of fat occurs in the adipose tissue of the deep layer. Patients who are classified as obese present an increase in thickness of this layer.15
Body adipose tissue deposits present variations depending on the gender and the type of hormones. Therefore, presentation will be in two distinct patterns: androgenic pattern and gynecoid pattern. Men present with the androgenic pattern when fat deposits will occur in the abdomen and dorsal regions. On the other hand, women present with the gynecoid pattern when fat accumulation occurs in thighs and ankles.16
Indications
Liposculpture is essentially used for body contouring for aesthetic and reconstructive purposes by the removal of fatty deposits with or without re-injection of the removed fat.10 The technique was described for the treatment of localized fat deposits that may not have responded to efforts of weight loss through exercise and dieting. It is important to stress, however, that liposuction is not a weight-loss method.16 Patients submitting to liposculpture should present with good skin elasticity with no flaccidness or a less elastic skin, as skin in this condition does not tighten so readily around the newly contoured shape.14
Penile augmentation can also be done with fat injection. Panfilov (2006)20 showed that the circumference of the penis increased 2 cm to 3 cm in 88 patients.
Liposuction techniques are also indicated for reconstructive purposes mainly to reduce flap thickness. It also can be used in association with fat transplantation to treat Romberg’s disease, HIV-related lipodystrophy, hemifacial microsomia syndrome and to correct liposuction sequelae.13,21
Other reconstructive indications include: laryngoplasty22 and treatment of urinary incontinence by lipoinjections in the periurethral area.23
Anesthesia and Preoperative Preparation
Liposuction can be performed under local anesthesia with or without intravenous sedation, regional anesthesia (epidural or spinal) and general anesthesia.14
Preparation of the Adipose Tissue to be Aspirated, Materials Used to Perform Liposuction and Surgical Techniques
Since the initial description of the liposuction technique, there has been a significant evolution regarding the preparation of the adipose tissue to be aspirated as well as the operative techniques and the surgical instruments used.24 Therefore, these three aspects of the liposuction techniques will be discussed in detail.
Preparation of the adipose tissue to be aspirated
Preparation of the adipose tissue is also known as ‘injection of the liposuction fluid’. This is very important mainly because the fluid injection determines the amount of fat to be aspirated, the amount of blood loss during the procedure and has a role on some postoperative complications.25
The liposuction technique was initially described with an initial injection of a hypotonic solution containing saline (100 cc), distilled water (20 cc), hyaluronidase (100 U) and epinephrine (0.1 cc).15,21 The purpose of this was to damage the fat cell membrane thus making the later aspiration of the adipose tissue easier.
Fournier, in 1983, described the liposuction technique with no previous injection of hypotonic fluids. This technique was named the dry method. According to this author the hypotonic solution did not damage the surface of fat cells and also increased surgical time. The main disadvantage of the dry method was the greater amount of perioperative blood loss, which required postoperative blood transfusion.3 This method is seldom used today.
In the tumescent method a larger amount of fluid is injected into the area to be aspirated; as much as 2-3 times the volume of adipose tissue to be aspirated. The volume of blood loss is about 1% of the final aspirated volume.16
Materials used to perform liposuction
According to the initial descriptions of the technique, cannulas presented a greater evolution. Initially, blunt-tipped cannulas with more than 5-mm bore were used. These cannulas allowed surgeons to remove a greater amount of adipose tissue; however, it was noted that the number of complications in the postoperative period was directly proportional to the diameter of the cannula. The main and most serious postoperative complication was blood loss and skin irregularities. Illouz demonstrated that if a 1500-3000 cc fat was removed, 25% of total blood volume needed to be transfused in the immediate postoperative period.15,26
Despite the development of new liposuction techniques such as the methods described above, syringe liposuction seems to be the one that allows the best control over the final volume of aspirated fat and results in the best surgical refinement, with the least risk of postoperative complications and need for retouching. Syringe liposuction also allows surgeons to remove a larger number of viable fat cells that can be used for fat transplantation, because of the reduced trauma to the adipose tissue. When fat transplantation is being considered, the removed fat should be re-injected immediately in multiple tunnels, as recommended by Coleman.27,28 This procedure is widely used to treat depressions or irregularities, improve anatomical structures of the face and body, and treat liposuction sequelae.29
Surgical techniques
Liposuction can be performed using many different techniques and the mechanisms by which the cannulas work are also varied. The main liposuction techniques are: syringe liposuction, suction-assisted liposuction (cannula attached to a vacuum device), power-assisted liposuction, ultrasound-assisted liposuction, laser-assisted liposuction and external ultrasound-assisted liposuction. The last four techniques use a standard suction device to remove the fat.
Syringe and suction-assisted liposculpture are the most commonly used methods of liposuction. In these techniques localized fat deposits are removed via a small cannula, which is inserted into a previously marked treatment region through a stab incision and attached to a syringe or a vacuum device.1
Power-assisted liposuction was developed to reduce both trauma to nerves and vessels, and surgeon fatigue. In this technique a special cannula is connected to a device that produces mechanized movements so that the surgeon does not need to move the cannula manually.14 This device can be powered electrically or by compressed air.
Ultrasound-assisted liposuction is also named ultrasonic liposuction. In this technique fat is removed via a special cannula linked in an ultrasound device that transmits vibrations to the treatment region. The vibrations rupture the walls of the fat cells, liquefying the adipose tissue and making it easier to remove. Afterwards, suction-assisted liposuction is performed to remove the liquefied adipose tissue. It is important to stress the potential for skin necrosis with this technique if superficial liposuction is performed.4–6
Laser-assisted liposuction works in a similar way to ultrasoundassisted liposuction. There are, however, many reports of skin burns when this technique is used to perform superficial liposuction.30 Therefore, when superficial liposuction is indicated this technique should be avoided.
The techniques described above were developed to reduce trauma, surgical time and surgeon fatigue, and to facilitate fat suction.16,30 However, as suction-assisted and syringe liposuction are the most commonly used methods this chapter will detail syringe liposuction; the technique outlined is associated with a previous infiltration of a fluid containing saline (500 ml) and epinephrine (1 : 1000 000) – a super-wet method.
Results
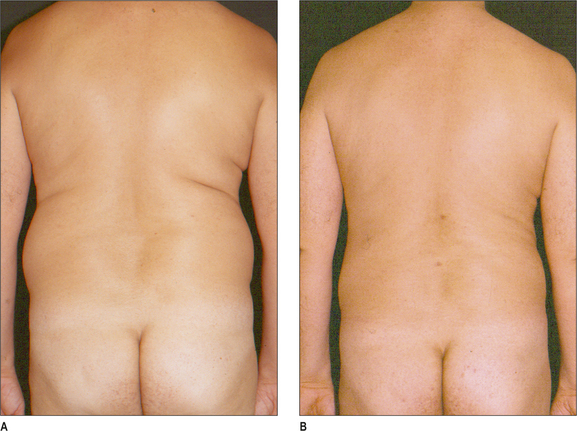
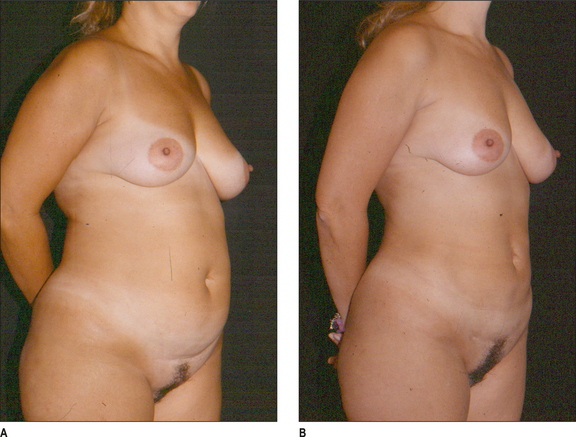
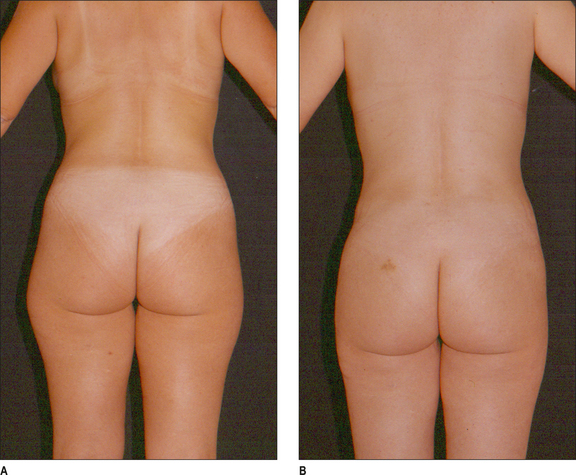
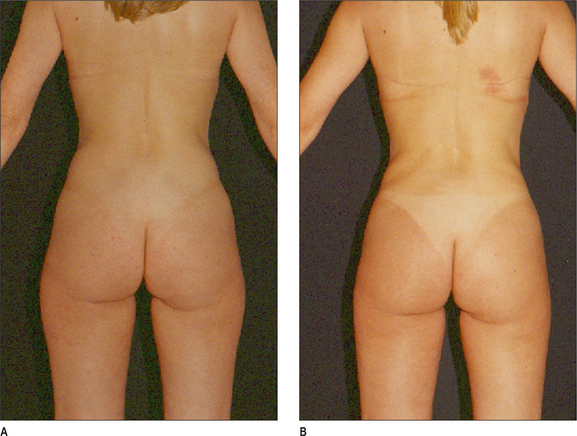
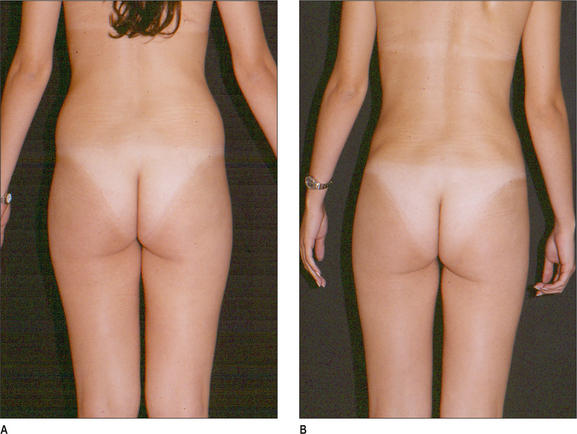
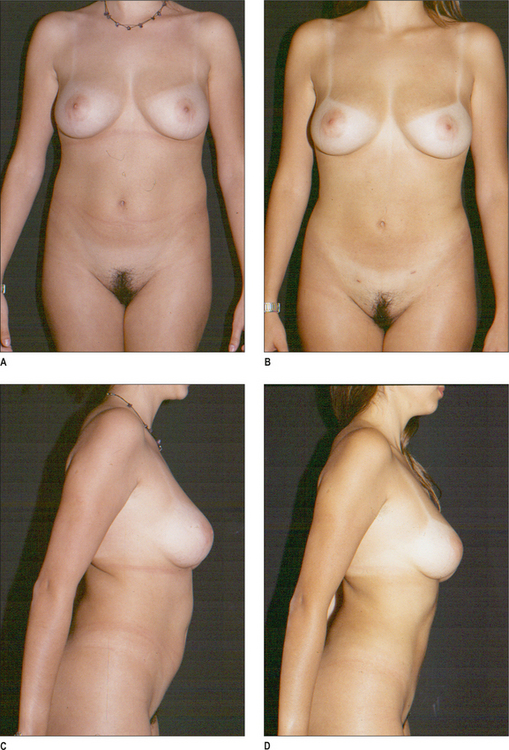
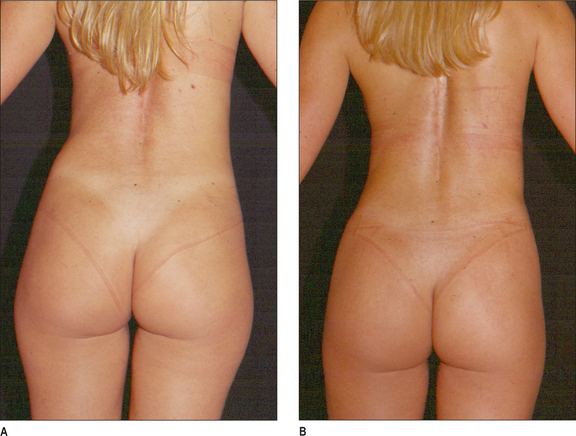
Some clinical examples using syringe liposuction plus super-wet method are shown in the figures.
Complications
Complications of liposuction can be minimized by correct selection of the technique to be used, proper preoperative planning regarding the site and volume of fat to be removed, and attention to the principles of the surgical technique. When they do occur, complications can be divided into two categories: 1) systemic and 2) local.
Systemic complications
This became possible for several reasons. The volume injected during liposuction promotes some com pression on the wall of the vessels, thus decreasing reabsorption; lidocaine absorption is low in subcutaneous tissue; this drug is diluted in a large amount of fluid which also decreases the reabsorption; and, finally, before the whole amount of injected lidocaine is in the serum, part of it has already been eliminated.
Infiltration of lidocaine has been used in patients who had undergone liposuction under general anesthesia. These plastic surgeons advocate the use of lidocaine to prevent postoperative pain. Perry et al33 verified that there is no postoperative pain reduction when this method is used.
Other cited34 though rare, complications are: vasculopathy,17 hyperpigmentation,19 third space fluids shifts, and hemorrhage.7
Local complications
Local complications are more frequent than the systemic ones and some of them could be avoided or the effects minimized. Edema, ecchymosis and seroma at the aspirated areas are common events and can occur in almost every surgical procedure.19 The effects usually disappear 2-3 weeks after surgery.
Although rare, prolonged edema and induration can last for up to 1 year.26 Manual lymphatic drainage35 and the use of a compressive dressing are adjuvant postoperative care procedures that can minimize edema and pain.
Liponecrosis and pseudocyst formation are complications that can occur when the volume of fat injected into one site exceeds 20 cc.14,15 These complications can be avoided with the injection of a small amount of fat graft through multiple tunnels.20,21
Depressions or irregularities in the liposuctioned area may also occur after any treatment.10 These deformities can be treated with fat injection. These complications can occur when patients have excess skin and also if aggressive superficial liposuction is carried out.
Limits
The maximum volume of fat that can be injected has not yet been determined.36,37 It is known that if a large volume of fat is injected into one area there is a greater possibility of fat necrosis and fat-graft reabsorption, and oily cysts may form. Also, calcification may occur with time.
The risks associated with the procedure increase when a large volume of fat is aspirated. The safety limit for liposuction was around 2000 cc when the dry technique was used. However, after the superwet technique was described by Klein38 in 1987, surgeons began to remove larger volumes of fat.
During the 1990s there was an increase in the number of fatalities following these procedures in comparison with the previous decade. These casualties did not occur due to hemorrhage but were secondary to other factors. Grazer and de Jong39 found that the mortality rate for patients who had undergone liposuction was approximately 1 : 5000. The main causes of death were pulmonary embolism (23.1%) and abdominal organ perforation (14.6%). Deaths related to anesthesia, sedation and medication occurred in 10% of the cases; however, this number is probably an underestimate, as most deaths related to lidocaine toxicity occur at home and in 28.5% of the cases an etiologic cause of death was not identified.
1. Toledo L.S. Syringe liposculpture: a two year experience. Aesth Plast Surg. 1991;15:321-326.
2. Har-Shai Y., Lindenbaum E., Bem-Itzhak O., Hirshowitz B. Large liponecrotic pseudocyst formation following cheek augmentation by fat injection. Aesth Plast Surg. 1996;20:417-419.
3. Fournier P.F. Reduction syringe liposculpturing. Dermatol Clin. 1990;8:539-551.
4. Zocchi M. Ultrasonic liposculpturing. Aesth Plast Surg. 1992;16:287-298.
5. Bruno G., Amadei F., Abbiati G. Liposculpture with ultrasound: biomedical considerations. Aesth Plast Surg. 1998;22:401-403.
6. Grippaudo F.R., Matarese R.M., Macone A., Mazzocchi M., Scuderi N. Effects of traditional and ultrasonic liposuction on adipose tissue: a biochemical approach. Plast Reconstr Surg. 2000;106:197-199.
7. Fournier P.F. Fat grafting: my technique. Dermatol Surg. 2000;26:1117-1128.
8. Pereira L.H., Radwanski H.N. Fat grafting of the buttocks and lower limbs. Aesth Plast Surg. 1996;20:409-416.
9. Toledo L.S., Mauad R. Complications of body sculpture: prevention and treatment. Clin Plast Surg. 2006;33:1-11.
10. Ishizuka M.M.A. Lipoaspiração e enxerto de gordura. In: Ferreira L.M., editor. Manual de cirurgia plástica. São Paulo: Ed. Atheneu; 2000:295-297.
11. Illouz Y-G. Reutilização do tecido adiposo lipoaspirado. In: Avelar J.M., e Illouz Y.-G., editors. Lipoaspiração. São Paulo: Hipócrates; 1986:117-122.
12. Illouz Y.-G. Estudo do adipócito nas lipodistrofias. In: Avelar J.M., Illouz Y.-G., editors. Lipoaspiração. São Paulo: Ed. Hipócrates; 1986:19-23.
13. Barcellos J. Enxerto de gordura. In: Mélega J.M., Zanini S.A., Psillakis J.M., editors. Cirurgia plástica reparadora e estética. São Paulo: Ed. Medsi; 1992:801-804.
14. Pitman G.H. Liposuction and body contouring. In: Aston S.J., Beasley R.W., Thorne C.H.M., editors. Grabb and Smith’s Plastic Surgery. Philadelphia: Lippincott-Raven, 1997.
15. Barcellos J. Lipoaspiração. Mélega J.M., Zanini A.S., Psillakis J.M., editors. Cirurgia Plástica – Reparadora e Estética. Medsi., 2a. Edição. 1992: 791-800.
16. Beran S.J. Contorno corporal. In: Weinzweig J., editor. Segredos em Cirurgia Plástica. Porto Alegre: Artmed; 2001:422-425.
17. Mottura A.A. Facelift postoperative recovery. Aesth Plast Surg. 2002;26:172-180.
18. Saldanha O.R., De Souza Pinto E.B., Mattos W.N.Jr, et al. Lipoabdominoplasty with selective and safe undermining. Aesthetic Plast Surg. 2003;27(4):322-327.
19. Erazo P.J., de Carvalho A.C.O. ‘Lipolifting’ de braço com tratamento da fáscia superficial (‘Lift’ Fascial). In: Badin A.Z., Ferreira L.M., editors. Videoendoscopia no Contorno Corporal e Procedimentos Complementares. Ris de Janeiro: Revinter; 2007:317. 26
20. Panfilov D.E. Augmentative phalloplasty. Aesth Plast Surg. 2006;30:183-197.
21. Feinendegen D.L., Baumgartner R.W., Vuadens P., Scroth G., Mattle H.P., Regli F., Tschopp H. Autologous fat injection for soft tissue augmentation in the face: a safe procedure? Aesth Plast Surg. 1998;22:163-167.
22. Sato K., Umeno H., Nakashima T. Histological investigation of liposuctioned fat for injection laryngoplasty. Am J Otolaryngol. 2005;26:219-225.
23. Palma P.C., Riccetto C.L., Herrmann V., Netto N.R.Jr. Repeated lipoinjections for stress urinary incontinence. J Endourol. 1997;11:67-70.
24. Toledo L.S., Mauad R. Fat injection: a 20-year revision. Clin Plast Surg. 2006;33:47-53.
25. Nahas F.X. Is the measurement of the fat volume removed in liposuction realistic? Plast Reconstr Surg. 2001;108:1834-1835.
26. Illouz Y.G. Body contouring by lipolisis: A 5-year experience with over 3.000 cases. Plast Reconstr Surg. 1983;72:591.
27. Coleman S.R. Long-term survival of fat transplants: controlled demonstrations. Aesth Plast Surg. 1995;19:421-425.
28. Coleman S.R. Hand rejuvenation with structural fat grafting. Plast Reconstr Surg. 2002;110:1731-1744.
29. Illouz Y.G. Utilização da gordura aspirada. In: Badin A.Z., Ferreira L.M., editors. Videoendoscopia no Contorno Corporal e Procedimentos Complementares. Ris de Janeiro: Revinter; 2007:287-300.
30. Badin A.Z.D., Teixeira V. Laserlipólise. In: Badin A.Z., Ferreira L.M., editors. Videoendoscopia no Contorno Corporal e Procedimentos Complementares. Ris de Janeiro: Revinter; 2007:301-316.
31. Smith K.A., Levine R.H. Influence of suction-assisted lipectomy on coagulation. Aesthetic Plast Surg. 1992;16(4):299.
32. Kenkel J.M., Brown S.A., Love E.J., et al. Hemodynamics, electrolytes, and organ histology of larger-volume liposuction in a porcine model. Plast Reconstr Surg. 2004;113(5):1391-1399.
33. Perry A.W., Petti C., Rankin M. Lidocaine is not necessary in liposuction. Plast Reconstr Surg. 1999;104(6):1900.
34. Anwar U.M., Ahmad M., Sharpe D.T. Necrotizing fasciitis after liposculpture. Aesth Plast Surg. 2004;28:426-427.
35. Rubin A., Hoefflin S.M., Rubin M. Treatment of postoperative bruising and edema with external ultrasound and manual lymphatic drainage. Plast Reconstr Surg. 2002;109:1469-1471.
36. Nahas F.X. Lipoaspiracad-Ricsos e Limites. In: Toledo L.S., editor. Lipoplastia. Sâo Paulo: Di-liveos Editora; 2006:21-28.
37. Nahas F.X., Ferreira L.M. Lipoasperacão. In: Ferreira L.M., editor. Guia de Medicina Ambulatorial e Hospitalar UNIFESP – Escola Paulista de Medicina. São Paulo: Ed Marole; 2007:717-722.
38. Klein J.A. Tumescend technique. Am J Cosmetic Surg. 1987;4:623.
39. Grazer F.M., de Jong R.H. Fatal outcomes from liposuction: census survey of cosmetio surgeons. Plast Reconstr Surg. 2000;105(1):436.