20 Lip augmentation
Summary and Key Features
• The lips are a defining feature of the face; enhancement of lip volume and structure through the use of fillers is a commonly requested cosmetic procedure
• Ethnic variations and aesthetic preferences should be considered in the evaluation and treatment planning for lip augmentation
• Hyaluronic acids are commonly used filler products for lip rejuvenation; their safety profile coupled with their potential reversibility using hyaluronidase makes them a frequent choice for treatment of the lips. Semipermanent and permanent fillers such as calcium hydroxylapatite, poly-L-lactic acid, silicone, and polymethylmethacrylate have higher incidences of nodule and granuloma formation and should therefore be avoided in the lips
• Injection of filler product into the rolled border of the lip will produce definition of the lip. Injection of filler product along the wet–dry junction of the lip will augment the volume of the lips
• Bruising and swelling are common, temporary side effects of lip augmentation. Small-volume injections can minimize these effects. Touch-up treatments 1–2 weeks later may be necessary
• Multimodality treatments including soft tissue fillers, botulinum toxins, and resurfacing techniques can be incorporated into treatment of the lips and perioral area
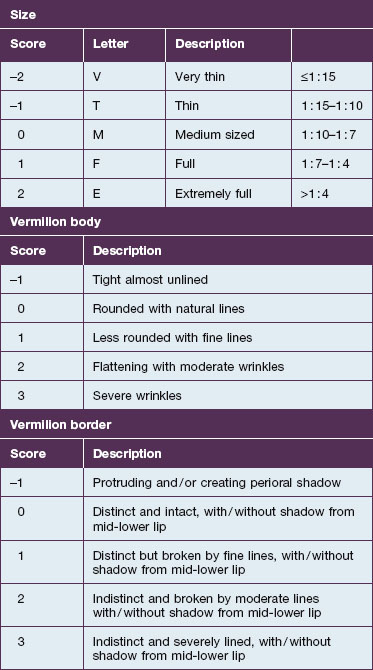
The aging process on the lips
Multiple assessment scales have been developed to quantify these changes. A numeric CKC scale (Table 20.1) was developed to aid in the initial assessment of patients, as well as their response to rejuvenation. Additionally, multiple lip-specific photographic scales have been developed in clinical studies. A recently presented abstract by Werschler et al developed, validated, and utilized a Lip Fullness Scale. Another recently presented abstract by Cohen et al validated the Perioral Lines at Rest (POL), Perioral Lines at Maximum Contraction (POLM), and Oral Commissure Severity (OCS) scales. Previous studies by Carruthers et al and Rossi et al have determined and validated photonumeric grading systems for assessing lip fullness, volume, and thickness (Figs 20.1 and 20.2). These scales may be of benefit in the initial assessment of patients and their clinical improvement following lip augmentation.

Figure 20.1 Photonumeric grading scale for assessing lip volume and thickness.
(Reprinted with permission from Rossi AB et al 2011 Development and validation of a photonumeric grading scale for assessing lip volume and thickness. J Eur Acad Dermatol Venereol 25(5):523-531.)
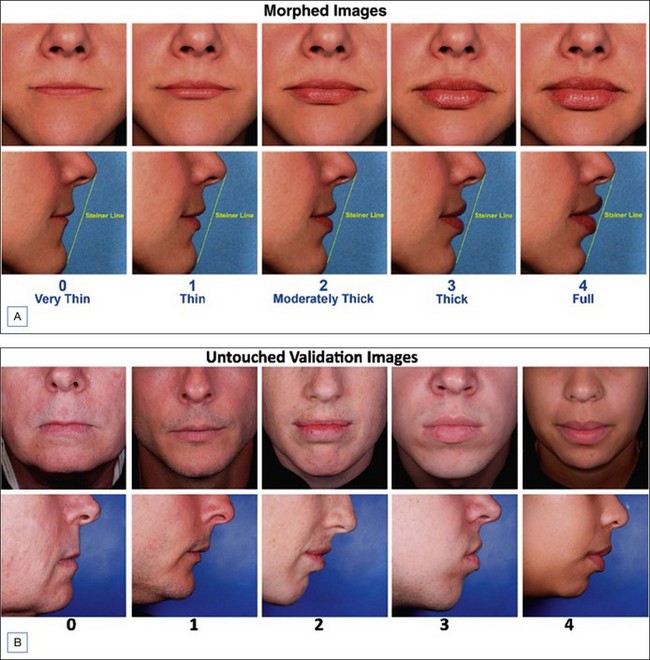
Figure 20.2 Validated lip fullness grading scale.
Reprinted with permission from Carruthers A, Carruthers J, Hardas B, et al 2008 A validated lip fullness grading scale. Dermatologic Surgery 34(suppl 2):S161-S166.
When done well, lip augmentation and rejuvenation can dramatically address many of these changes associated with aging lips to both replace the volume loss and redefine the lip structure. In a 2009 study by Werschler et al, after treatment with a hyaluronic acid (HA) filler (Juvéderm® Ultra®, Allergan Inc., Irvine, CA), multiple features of the lips were improved, including: (1) proportional lip size relative to the face, (2) proportional upper and lower central lip fullness, (3) sharp, well-defined vermilion borders, (4) distinct Cupid’s bow peaks and a well-defined philtrum, and (5) oral commissure fullness to support the lateral aspect of the lip. In the study, the investigators rated these five attributes as ‘adequate’ in only 32–48% of subjects prior to augmentation; after the augmentation was performed, the attributes were scored as ‘adequate’ in 80–90% of subjects.
Injection techniques for lip rejuvenation
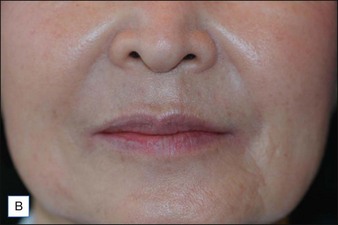
In general, injections in the wet–dry junction of the lip and the vermilion border of the lip will augment the volume of the lips, whereas injections in the rolled border of the lip produce definition (Fig. 20.3A, B). Overall, many patients require slightly more volume in the lower lip than in the upper lip, but the exact volume and proportions must be individualized for each patient. For example, African American patients may require greater volume injections into the upper lip than in the lower lip to achieve their ideal outcome.
A patient presented for lip rejuvenation (Fig. 20.3A). On examination, there is loss of the shape and structure of the upper lip. Overall, the upper lip is flat, with a loss of the Cupid’s bow. The philtral columns are also not well defined. There are multiple perioral radiating rhytides. The lower lip is also small and lacks definition.
The patient underwent lip rejuvenation with 1 mL of hyaluronic acid product (Fig. 20.3B). Following the augmentation, note the reshaped and defined Cupid’s bow; there is also greater definition of the inferior aspects of the philtral columns. The overall volume of the upper and lower lips is increased slightly as well. Finally, there is a reduction in the appearance of the radiating perioral rhytides.
Alam M, Gladstone H, Kramer EM, et al. ASDS Guidelines of care: injectable fillers. with the Guidelines Task Force. Dermatologic Surgery. 2008;34:S115–S148.
Ali M, Ende K, Maas C. Perioral rejuvenation and lip augmentation. Facial Plastic Surgery Clinics of North America. 2007;15(4):491–500.
Carruthers A, Carruthers J, Hardas B, et al. A validated lip fullness grading scale. Dermatologic Surgery. 2008;34(suppl 2):S161–S166.
Carruthers J, Glogau R, Blitzer A, the Facial Aesthetics Consensus Group Faculty. Advances in facial rejuvenation: botulinum toxin type A, hyaluronic acid dermal fillers, and combination therapies – consensus recommendations. Plastic and Reconstructive Surgery. 2008;121(suppl 5):S5–S30.
Cohen JL, Thomas J, Paradkar D, et al 2011 An inter- and intra-rater reliability study of 3 photographic scales for classifying aesthetic features of the perioral area. Presented abstract at the American Society for Dermatologic Surgery Annual Meeting, Washington DC, November
Custis T, Beynet D, Carranza D, et al. Comparison of treatment of melomental fold rhytides with cross-linked hyaluronic acid combined with onabotulinumtoxinA and cross-linked hyaluronic acid alone. Dermatologic Surgery. 2010;36(suppl 3):S1852–S1858.
Downie J, Mao Z, Lo TWR, et al. A double-blind, clinical evaluation of facial augmentation treatments: a comparison of PRI 1, PRI 2, Zyplast(r) and Perlane(r). Journal of Plastic, Reconstructive and Aesthetic Surgery. 2009;62:1636–1643.
Ibher N, Kloepper J, Penna V, et al. Changes in the aging upper lip – a photomorphic and MRI-based study (on a quest to find the right rejuvenation approach). Journal of Plastic, Reconstructive and Aesthetic Surgery. 2008;61:1170–1176.
Jacono AA. A new classification of lip zones to customize injectable lip augmentation. Archives of Facial Plastic Surgery. 2008;10(1):25–29.
Perkins NW, Smith SP, Williams EF. Perioral rejuvenation: complementary techniques and procedures. Facial Plastic Surgery Clinics of North America. 2007;15(4):423–432.
Rossi AB, Nkengne A, Stamatas G, et al. Development and validation of a photonumeric grading scale for assessing lip volume and thickness. Journal of the European Academy of Dermatology and Venereology. 2011;25(5):523–531.
Scalfani AP. Soft tissue fillers for management of the aging perioral complex. Facial Plastic Surgery. 2005;21(1):74–78.
Segall L, Ellis DA. Therapeutic options for lip augmentation. Facial Plastic Surgery Clinics of North America. 2007;15(4):485–490.
Talakoub L, Wesly NO. Differences in perceptions of beauty and cosmetic procedures performed in ethnic patients. Seminars in Cutaneous Medicine and Surgery. 2009;28:115–129.
Werschler WP, Brandt F, Thomas J, et al 2009 Lip augmentation with a 24 mg/ml hyaluronic acid filler: an open label, multicenter study. Presented abstract at the American Academy of Dermatology Annual Meeting, San Francisco, CA, March
Werschler WP, Fagien S, Grimes P, et al 2011 An inter-rater and intra-rater reliability study of a photographic scale for lip fullness. Presented abstract at the American Society for Dermatologic Surgery Annual Meeting, Washington DC, November
Wong WW, Davis DG, Camp MC, et al. Contribution of lip proportions to facial aesthetics in different ethnicities: a three-dimensional analysis. Journal of Plastic, Reconstructive and Aesthetic Surgery. 2010;63:2032–2039.