Chapter 23 Limitations and Uses of the ECG
Important Limitations of the ECG
Like most clinical tests the ECG yields both false-positive and false-negative results, as previously defined. A false-positive result is exemplified by an apparently abnormal ECG in a normal subject. For example, prominent precordial voltage may occur in the absence of left ventricular hypertrophy (LVH) (see Chapter 6). Furthermore, Q waves may occur as a normal variant and therefore do not always indicate heart disease (see Chapters 8 and 9). In other cases, Q waves may be abnormal (e.g., due to hypertrophic cardiomyopathy) but lead to a mistaken diagnosis of myocardial infarction (MI).
False-negative results, on the other hand, occur when the ECG fails to show evidence of some cardiac abnormality. For example, some patients with acute MI may not show diagnostic ST-T changes, and patients with severe coronary artery disease may not show diagnostic ST segment depressions during stress testing (see Chapter 9).
Utility of the ECG in Special Settings
Although the ECG has definite limitations, it often helps in the diagnosis of specific cardiac conditions and sometimes aids in the evaluation and management of general medical problems such as life-threatening electrolyte disorders (Box 23-1). Some particular areas in which the ECG may be helpful are described here:
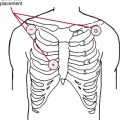
ST segment elevation in right chest precordial leads (e.g., V4-6R) in a patient with acute inferior infarction indicates associated right ventricular ischemia or infarction (see Chapter 8).
Persistent ST elevations several weeks after an MI should suggest a ventricular aneurysm.
A new S1Q3T3 pattern or right bundle branch block (RBBB) pattern, particularly in association with sinus tachycardia, should suggest the possibility of acute cor pulmonale resulting from, for example, pulmonary embolism (see Chapter 11).
Low QRS voltage in a patient with elevated central venous pressure (distended neck veins) and sinus tachycardia suggests possible pericardial tamponade. Sinus tachycardia with electrical alternans is virtually diagnostic of pericardial effusion with tamponade (see Chapter 11).
LVH is seen in most patients with severe aortic stenosis or severe aortic regurgitation.
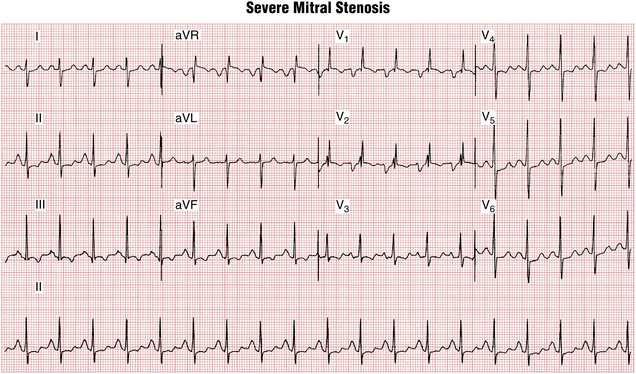
ECG signs of left atrial enlargement (abnormality) with concomitant RVH strongly suggest mitral stenosis (Fig. 23-1).
Most patients with a moderate to large atrial septal defect have an RBBB pattern.
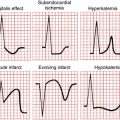
Severe hyperkalemia, a life-threatening electrolyte abnormality, virtually always produces ECG changes, beginning with T wave peaking, loss of P waves, QRS widening, and finally asystole (see Chapter 10).
Unexplained AF (or sinus tachycardia at rest) should prompt a search for hyperthyroidism.
The combination of low voltage and slow precordial R wave progression is commonly seen with chronic obstructive lung disease (see Chapter 11).
The ECG-CHF (chronic heart failure) triad of relatively low limb lead voltage, prominent precordial voltage, and slow R wave progression suggests an underlying dilated cardiomyopathy (see Chapter 11).
Common General Medical Applications of the ECG
Syncope
Patients with syncope resulting from aortic stenosis generally show LVH on their resting ECG. Primary pulmonary hypertension is most common in young and middle-aged adult women. The ECG generally shows RVH. The presence of frequent VPBs may be a clue to intermittent sustained VT. Evidence of previous Q wave MI with syncope should suggest the possibility of sustained monomorphic VT. Syncope with QT(U) prolongation should suggest torsades de pointes, a potentially lethal ventricular arrhythmia (see Chapter 16). A severe bradycardia (usually from high-degree atrioventricular (AV) heart block, sometimes with torsades) in a patient with syncope constitutes the Adams-Stokes syndrome (see Chapter 17).
Coma
An ECG should be obtained in all comatose patients. If coma is from MI with subsequent cardiac arrest (anoxic encephalopathy), diagnostic ECG changes related to the infarct are usually seen. Subarachnoid hemorrhage or certain other types of central nervous system pathology may cause very deep T wave inversions (see Chapter 9), simulating the changes of MI. When coma is associated with hypercalcemia, the QT interval is often short. Myxedema coma generally presents with ECG evidence of sinus bradycardia and low voltage. Widening of the QRS complex in a comatose patient should also always raise the possibility of drug overdose (tricyclic antidepressant or phenothiazine) or hyperkalemia. The triad of: a wide QRS, a prolonged QT interval, and sinus tachycardia is particularly suggestive of tricyclic antidepressant overdose (Chapter 10).
Weakness
An ECG may be helpful in evaluating patients with unexplained weakness. Elderly or diabetic patients, in particular, may have relatively “silent” MIs with minimal or atypical symptoms, such as the onset of fatigue or general weakness. Distinctive ECG changes may also occur with certain pharmacologic and metabolic factors (e.g., hypokalemia or hypocalcemia) that cause weakness (see Chapter 10).
Reducing Medical Errors: Common Pitfalls in ECG Interpretation
You can help minimize errors in interpreting ECGs by taking care to analyze all the points listed in the first section of Chapter 22. Many mistakes result from the failure to be systematic. Other mistakes result from confusing ECG patterns that are “look-alikes.” Important reminders are provided in Box 23-2. Some common pitfalls in ECG interpretation are discussed further here.
BOX 23-2 Minimizing ECG Misinterpretation: Some Important Reminders
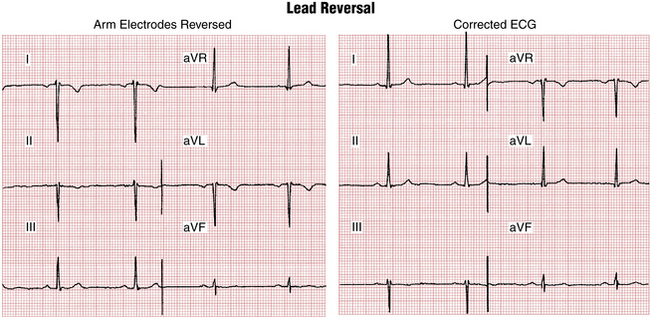
• Exclude limb lead reversal. (For example, a negative P wave with a negative QRS complex in lead I suggests a left/right arm electrode switch.)
• Look for hidden P waves, which may indicate atrioventricular (AV) block, blocked atrial premature beats, or atrial tachycardia with block.
• With a regular narrow-complex tachycardia at about 150 beats/min at rest, consider atrial flutter with 2:1 AV block versus paroxysmal supraventricular tachycardia or (less likely) sinus tachycardia.
• With group beating (clusters of QRS complexes), consider Mobitz type I (Wenckebach) or II block or blocked atrial premature beats.
• With wide QRS complexes and with short PR intervals, consider the Wolff-Parkinson-White preexcitation pattern.
• With wide QRS complexes without P waves or with AV block, think of hyperkalemia.
Unless recognized and corrected, inadvertent reversal of limb lead electrodes can cause diagnostic confusion. For example, reversal of the left and right arm electrodes usually causes an apparent rightward QRS axis shift as well as an abnormal P wave axis that simulates an ectopic atrial rhythm (Fig. 23-2). As a general rule, when lead I shows a negative P wave and a negative QRS, reversal of the left and right arm electrodes should be suspected.
Coarse AF and atrial flutter are sometimes confused. When the fibrillatory (f) waves are prominent (coarse), the rhythm is commonly mistaken for atrial flutter. However, with AF the ventricular rate is erratic, and the atrial waves are not exactly consistent from one segment to the next. With pure atrial flutter the atrial waves are identical from one moment to the next, even when the ventricular response is variable (see Chapter 15).
The Wolff-Parkinson-White (WPW) pattern is sometimes mistaken for bundle branch block, hypertrophy, or infarction because the preexcitation results in a wide QRS complex and may cause increased QRS voltage, T wave inversions, and pseudoinfarction Q waves (see Chapter 12).
Normal variant and pathologic Q waves require special attention. Remember that Q waves may be a normal variant as part of QS waves in leads aVR, aVL, aVF, III, V1, and occasionally V2 (see Chapter 8). Small q waves (as part of qR waves) may occur in leads I, II, III, aVL, and aVF as well as in the left chest leads (V4 to V6). These “septal” Q waves are less than 0.04 sec in duration. On the other hand, small pathologic Q waves may be overlooked because they are not always very deep. In some cases it may not be possible to state definitively whether or not a Q wave is pathologic.
MAT and AF are often confused because the ventricular response in both is usually rapid and irregular. With MAT, you need to look for multiple different P waves. With AF, you must be careful not to mistake the sometimes “coarse” f waves for actual P waves.
Severe hyperkalemia must be considered immediately in any patient with an unexplained wide QRS complex, particularly if P waves are not apparent. Delay in making this diagnosis can be fatal because severe hyperkalemia may lead to asystole and cardiac arrest while the clinician is waiting for the laboratory report (see Chapter 10).