Chapter 45 Light Agents
OVERVIEW.
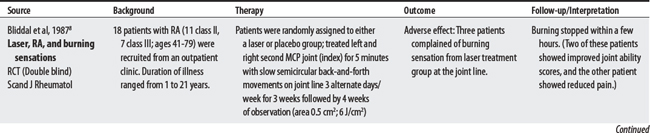
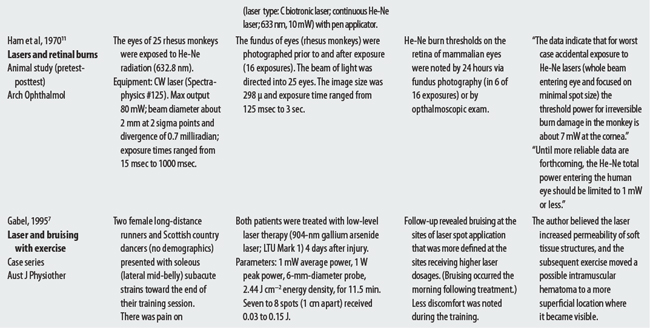
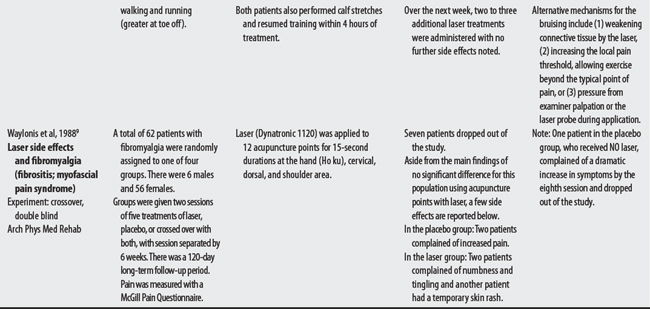
Laser stands for light amplification by stimulated emission of radiation. Cold (low power) lasers use less than 60 mW of power and produce little or no thermal response. The He-Ne cold laser has generated interest in physical therapy because of its purported wound healing and analgesic effects (when used over acupuncture or trigger points).1–5 Users must obtain an investigational device exemption from the FDA for this class III medical device. In 2002, the FDA approved its use for carpal tunnel syndrome.5,6
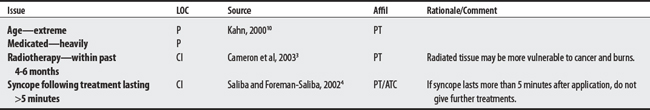
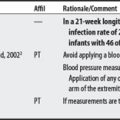
SUMMARY: CONTRAINDICATIONS AND PRECAUTIONS.
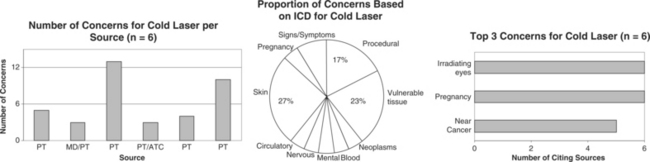
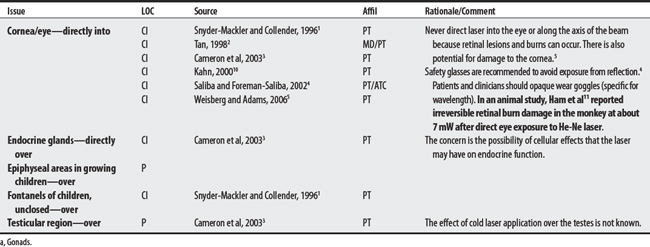
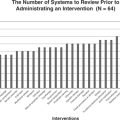
Six sources cited a total of 23 concerns for cold laser. Concerns ranged from 3 to 13 per source, with a physical therapist citing the largest number. The largest proportion of concerns were listed under skin, vulnerable tissue, or procedural categories. Many concerns are inadequately explained for cold laser; perhaps the basis for some concerns is a lack of information on its effects on tissue.3 The most frequently cited concern was irradiating the eyes (a concern well supported by evidence), use during pregnancy, and application near cancerous lesions.
CONTRAINDICATIONS AND PRECAUTIONS
D50-D89 DISEASES OF 3BLOOD AND BLOOD-FORMING ORGANS
F00-F99 MENTAL AND BEHAVIORAL DISORDERS
G00-G99 DISEASES OF THE NERVOUS SYSTEM
I00-I99 DISEASES OF THE CIRCULATORY SYSTEM
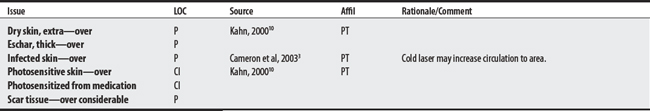
L00-L99 DISEASES OF THE SKIN AND SUBCUTANEOUS TISSUE
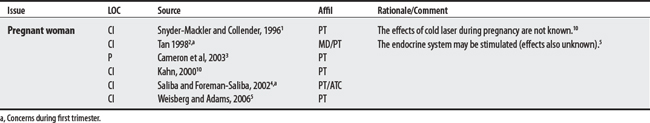
O00-O99 PREGNANCY, CHILDBIRTH, AND PUERPERIUM
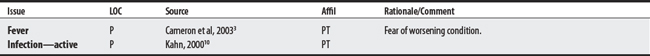
R00-R99 SYMPTOMS, SIGNS, AND ABNORMAL CLINICAL AND LABORATORY FINDINGS (NOT ELSEWHERE CLASSIFIED)
1 Snyder-Mackler L, Collender SL. Therapeutic uses of light in rehabilitation. In Michlovitz SL, editor: Thermal agents in rehabilitation, ed 3, Philadelphia: F.A. Davis, 1996.
2 Tan JC. Practical manual of physical medicine and rehabilitation: diagnostics, therapeutics, and basic problems. St. Louis: Mosby, 1998.
3 Cameron MH, Perez D, Otaño-Lata S. Electromagnetic radiation. In: Cameron MH, editor. Physical agents in rehabilitation: from research to practice. St. Louis: Saunders, 2003.
4 Saliba E, Foreman-Saliba S. Low-power lasers. In Prentice WE, editor: Therapeutic modalities for physical therapists, ed 2, New York: McGraw-Hill, 2002.
5 Weisberg J, Adams D. Low-level laser therapy. In: Hecox B, Mehreteab TA, Weisberg J, editors. Integrating physical agents in rehabilitation. Upper Saddle River (NJ): Pearson Prentice Hall, 2006.
6 Basford JR. Therapeutic physical agents. Delisa JA, editor. Physical medicine and rehabilitation: principles and practices, ed 4, vol 1. Philadelphia: Lippincott Williams & Wilkins, 2005.
7 Gabel P. Does laser enhance bruising in acute sporting injuries? Aust J Physiother. 1995;41:273-275.
8 Bliddal H, Hellesen C, Ditleven P, et al. Soft-laser therapy of rheumatoid arthritis. Scand J Rheumatol. 1987;16:225-228.
9 Waylonis GW, Wilke S, O’Toole D, et al. Chronic myofascial pain management by low-output helium-neon laser therapy. Arch Phys Med Rehab. 1988;69(12):1017-1020.
10 Kahn J. Principles and practice of electrotherapy, ed 4. New York: Churchill Livingstone, 2000.
11 Ham WTJr, Geeraets WJ, Mueller HA, et al. Retinal burn thresholds for the helium-neon laser in the rhesus monkey. Arch Ophthalmol. 1970;84(6):797-809.
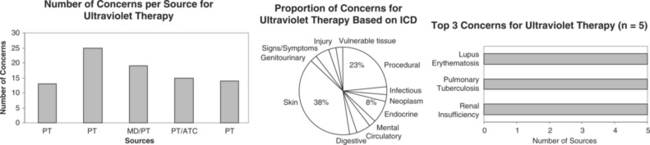
45.2 Ultraviolet (UV) Therapy
OVERVIEW.
Ultraviolet therapy uses electromagnetic radiation beyond the violet end, acting to facilitate steroid metabolism, enhance vasomotor responses, and elicit bacteriocidal and antirachitic (“against rickets”) effects.1 Clinically, it is used to treat psoriasis (for nonacute stages by promoting exfoliation), acne vulgaris (by promoting exfoliation), uremic pruritus (by reducing skin itchiness in chronic renal failure), jaundice (by eliminating bilirubin in newborns), and wounds (by killing bacteria, boasting immune response and circulation).2
OTHER ISSUES: UV AND INFANTS.
In 1992, Siegfried et al3 reported a case series of two premature infants who received phototherapy (UVA) for neonatal jaundice and sustained phototherapy-induced erythema, one with second-degree burns after exposure to UVA without protective Plexiglas shields (see Thermotherapy for details).
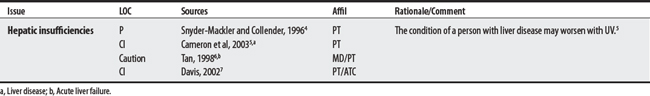
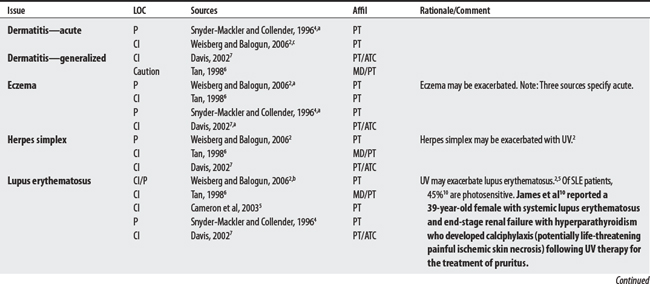
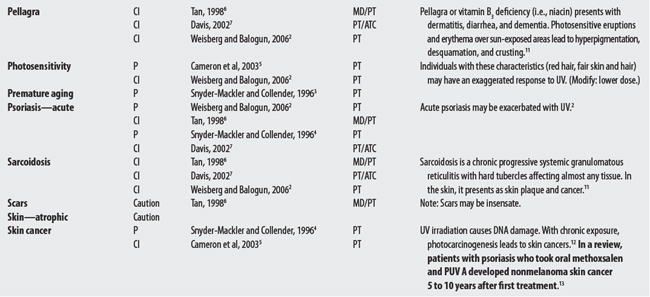
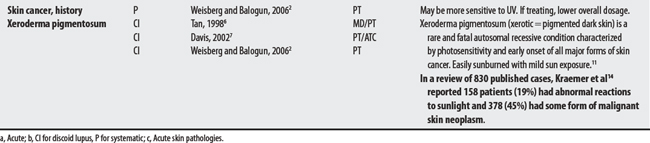
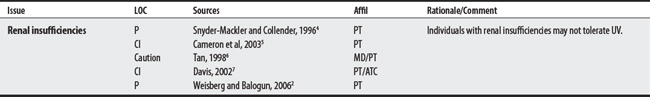
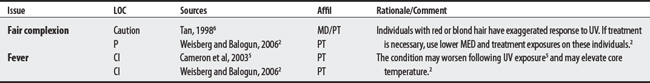
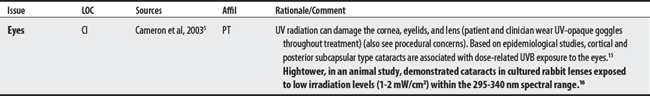
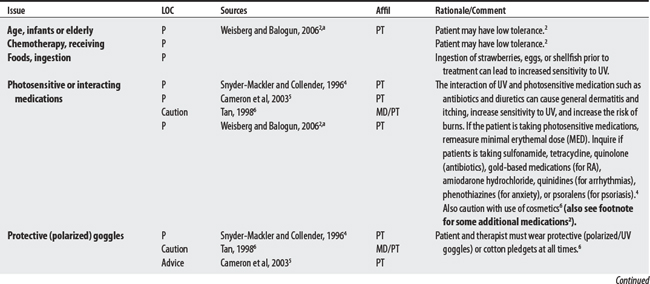
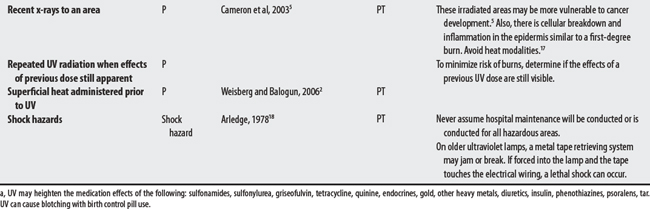
CONTRAINDICATIONS AND PRECAUTIONS
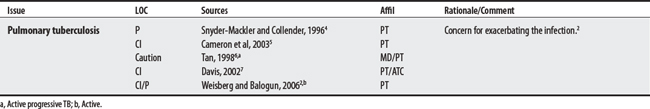
A00-B99 CERTAIN INFECTIONS AND PARASITIC DISEASES
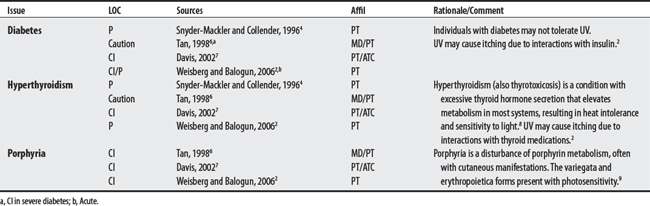
E00-E90 ENDOCRINE, NUTRITIONAL, AND METABOLIC DISEASES
F00-F99 MENTAL AND BEHAVIORAL DISORDERS
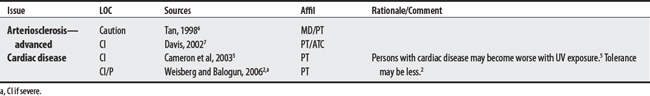
I00-I99 DISEASES OF THE CIRCULATORY SYSTEM
K00-K93 DISEASES OF THE DIGESTIVE SYSTEM
L00-L99 DISEASES OF THE SKIN AND SUBCUTANEOUS TISSUE
N00-N99 DISEASES OF THE GENITOURINARY SYSTEM
S00-T98 INJURY, POISONING, AND CERTAIN OTHER CONSEQUENCES OF EXTERNAL CAUSES
1 Bottomley JM. Quick reference dictionary for physical therapy. Thorofare (NJ): Slack, 2000.
2 Weisberg J, Balogun JA. Ultraviolet radiation. In: Hecox B, Mehreteab TA, Weisberg J, editors. Integrating physical agents in rehabilitation. Upper Saddle River (NJ): Pearson Prentice Hall, 2006.
3 Siegfried EC, Stone MS, Madison KC. Ultraviolet light burn: a cutaneous complication of visible light phototherapy of neonatal jaundice. Pediatr Dermatol. 1992;9:278-282.
4 Snyder-Mackler L, Collender SL. Therapeutic uses of light in rehabilitation. In Michlovitz SL, editor: Thermal agents in rehabilitation, ed 3, Philadelphia: F.A. Davis, 1996.
5 Cameron MH, Perez D, Otaño-Lata S. Electromagnetic radiation. In: Cameron MH, editor. Physical agents in rehabilitation: from research to practice. St. Louis: Saunders, 2003.
6 Tan JC. Practical manual of physical medicine and rehabilitation: diagnostics, therapeutics, and basic problems. St. Louis: Mosby, 1998.
7 Davis JM. Ultraviolet therapy. In Prentice WE, editor: Therapeutic modalities for physical therapists, ed 2, New York: McGraw-Hill, 2002.
8 Goodman CC, Snyder TEK. The endocrine and metabolic systems. In Goodman CC, Boissonnault WG, Fuller KS, editors: Pathology: implications for the physical therapist, ed 2, Philadelphia: Saunders, 2003.
9 Dorland’s illustrated medical dictionary. ed 24. Philadelphia: Saunders; 1965.
10 James LR, Lajoie G, Prajapati D, et al. Calciphylaxis precipitated by ultraviolet light in a patient with end-stage renal disease secondary to systemic lupus erythematosus. Am J Kidney Dis. 1999;34(5):932-936.
11 Bolognia JC, Jarizzo JL, Rapini RP. Dermatology. Edinburgh, Scotland: Mosby, 2003.
12 Matsumura Y, Ananthaswamy HN. Toxic effects of ultraviolet radiation on the skin. Toxicol Appl Pharmacol. 2004;195(3):298-308.
13 Burns F. Cancer risk associated with therapeutic irradiation of skin. Arch Dermatol. 1989;125:979-981.
14 Kraemer KH, Lee MM, Scotto J. Xeroderma pigmentosum: Cutaneous, ocular, and neurologic abnormalities in 830 published cases. Arch Dermatol. 1987;123:241-250.
15 Taylor HR. The biological effects of ultraviolet-B on the eye. Photochem Photobiol. 1989;50(4):489-492.
16 Hightower K, McCready J. Physiological effects of UVB irradiation on cultured rabbit lens. Invest Ophthalmol Vis Sci. 1992;33(5):1783-1787.
17 Goodman CC, Snyder TEK. Problems affecting multiple systems. In Goodman CC, Boissonnault WG, Fuller KS, editors: Pathology: implications for the physical therapist, ed 2, Philadelphia: Saunders, 2003.
18 Arledge RL. Prevention of electric shock hazards in physical therapy. Phys Ther. 1978;58(10):1215-1217.