Life-Threatening Emergencies (Rescue Breathing/CPR/Choking)
Basic Resuscitation
Adult
1. Check the patient for unresponsiveness. If the person is not responsive and not breathing or not breathing normally, call for help and return to the patient.
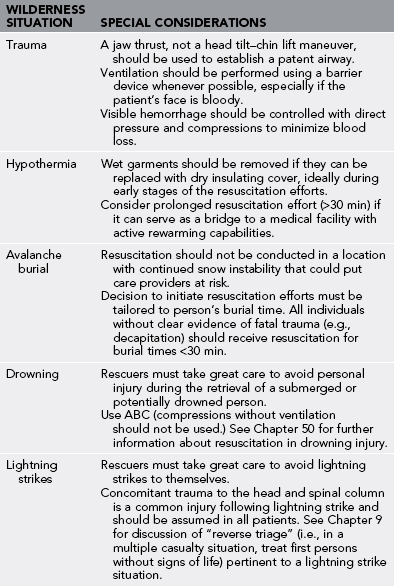
2. C: If the patient is still not breathing normally, coughing, or moving, check for a carotid pulse for no longer than 10 seconds. If no pulse is detected in 10 seconds, begin chest compressions. Push down in the center of the chest a distance of 5 cm (2 inches) 30 times. Pump hard and fast at the rate of at least 100 pumps per minute, faster than once per second (Figs. 25-1 and 25-2).
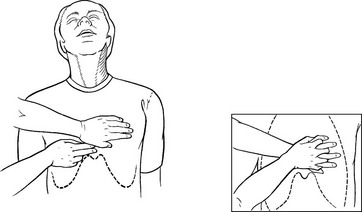
FIGURE 25-1 Hand position for chest compressions in CPR.

FIGURE 25-2 Chest compressions: adult.
3. A: Tilt the head back, and lift the chin.
4. B: Pinch nose and cover the mouth with yours, and blow until you see the chest rise. Give two breaths. Each breath should take 1 second. An improvised CPR barrier may be crafted from a glove (Fig. 25-3).
5. Continue with 30 pumps and two breaths until help arrives, then the rescuers should switch roles every five cycles, continuing at a ratio of 30 : 2 to minimize fatigue. A brief resuscitation pause to assess for the presence of spontaneous pulses should be performed every 2 minutes.
Child and Infant
The guidelines are the same as for an adult with the following exceptions:
1. Chest compressions should attempt a depth of one-third of the depth of the chest (about 4 cm [ inches]).
inches]).
2. See hand placement for children (Fig. 25-4) and infants (Fig. 25-5).

FIGURE 25-4 Chest compressions: child.

FIGURE 25-5 Chest compressions: infant
3. See rescue breathing for infants (Fig. 25-6).

FIGURE 25-6 Rescue breathing: infant.
1. A situation in which resuscitation efforts would put rescuers at risk for significant morbidity or mortality
2. A patient with a core body temperature of less than 15° C (59° F)
3. A patient with a frozen chest wall
4. A patient who has been submersed in cold water for more than 60 minutes
5. A patient with an obvious lethal injury such as decapitation
6. A situation in which resuscitation would significantly delay evacuation of a hypothermic patient to controlled rewarming
When to Stop CPR
1. It is well established that after 15 to 30 minutes of CPR, if a patient does not respond, he or she probably never will. The exceptions have been patients who were profoundly hypothermic.
2. If CPR is not successful in resuscitating a patient after 30 minutes, and the patient is not profoundly hypothermic, then it is usually reasonable to discontinue CPR.
3. Current resuscitation guidelines provide recommendations for specific wilderness situations (Table 25-1).
Choking/Obstructed Airway
Treatment
1. For a choking adult or child, perform the Heimlich maneuver:
a. Stand behind the patient, and wrap your arms around the patient’s waist.
b. Make a fist with one of your hands, and place it just above the patient’s navel and below the rib cage, with the thumb side against the abdomen.
c. Grasp your fist with the other hand, and pull your hands forcefully toward you, into the patient’s abdomen and slightly upward with a quick thrust.
d. If unsuccessful, repeat the procedure to achieve a total of four or five thrusts (Fig. 25-7).
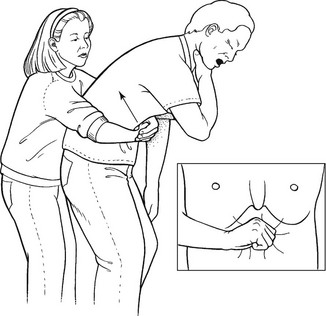
FIGURE 25-7 Heimlich maneuver: standing.
2. If the adult or child becomes unconscious, do the following:
a. Lay the patient on his or her back, and attempt rescue breathing.
b. If rescue breathing is unsuccessful because of an airway obstruction, perform the Heimlich maneuver while kneeling down and straddling the patient’s thighs. Use the heel of the hand instead of a fist (Fig. 25-8).

FIGURE 25-8 Heimlich maneuver: supine.
c. If still unsuccessful, sweep the mouth with one or two fingers to try to remove any foreign material.
d. Continue to perform the Heimlich maneuver, and periodically attempt rescue breathing.
e. If multiple attempts at clearing the airway and ventilating the patient are unsuccessful, perform a cricothyrotomy.
3. For a choking infant (younger than 1 year), do the following:
a. If the infant is coughing and appears to be getting sufficient air, do not interfere with his or her attempts to cough the obstruction out of the airway.
b. If the infant cannot cough, cry, or get sufficient air, lay him or her face down, supported by and straddling your forearm, while resting your forearm on your thigh. Support the infant’s head by grasping under the chin and holding onto the jaw. Make sure the infant’s head is lower than the rest of the body.
c. Using the heel of your free hand, give up to five firm back blows between the infant’s shoulder blades.
d. If the obstruction is not cleared, place your free hand on the infant’s back, holding the back and head so that they are sandwiched between both of your arms.
e. Carefully support the trunk and head while flipping the infant over to a supine position. Support the infant on your thigh, keeping the infant’s head lower than the rest of the body. Give five quick, downward chest thrusts with two fingertips positioned over the infant’s lower breastbone 1.3 cm ( inch) below the nipples.
inch) below the nipples.
f. Look into the infant’s mouth for a foreign object, and try to remove it.
g. If the infant becomes unconscious, try mouth-to-mouth rescue breathing. If you are unsuccessful at getting air into the infant’s lungs, repeat steps a through e until you have removed the object or the child has started to breathe on his or her own.