44
Lichen sclerosus

Primary lesion: ivory white, flat-topped papule which, on skin, will develop a keratotic follicular surface plug (delling).

Papules coalesce into atrophic plaques with a dull or glistening, smooth or wrinkled surface. Focal hemorrhage may occur in the plaque.
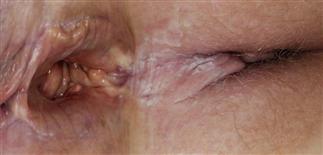
Painful vaginal mucosal lesions are atrophic and fragile. Lesions often hemorrhage, erode, and scar.

Penile lesions favor the glans and coronal sulcus but may extend to the shaft. Fragile atrophic lesions develop hemorrhages and erosions.
DESCRIPTION
Uncommon, chronic disease of unknown etiology that causes focal atrophy of skin, penis, and vagina.
HISTORY
• Skin lesions are rare and usually asymptomatic. • Most cases involve vulva or penis (balanitis xerotica obliterans). Genital disease occurs in young girls and uncircumcised boys, and in women over 60 and older uncircumcised men. • Women have itching, pain with intercourse and urination. Men have inflammation of the foreskin, which if untreated leads to narrowing of the foreskin. Irritation and infection occur because the foreskin cannot be retracted. • Squamous cell carcinoma develops in 3% of mucosal lesions.
PHYSICAL FINDINGS
• Skin lesions begin as white papules with keratotic follicular surface plugs (delling). They coalesce into dull white, atrophic plaques with a fragile wrinkled surface. Focal hemorrhage may occur. • Mucosal surfaces are white, fragile, atrophic. Minor trauma causes erosions, bleeding, and leads to scarring. • Penile lesions occur on the glans and may extend into the urethral meatus and to the shaft. • The white atrophic changes of the vulva may extend to and surround the anus. • Focal purpura and erosions are common. Tissues shrink, scar, and distort normal structures.
TREATMENT
• Protect mucosal surfaces with heavy lubricants (e.g. Aquaphor). • Initial treatment: group V topical steroid ointment or cream b.i.d. for 2 weeks. • Group I topical steroid creams or ointments (clobetasol) used for resistant vulvar disease, b.i.d. for up to 1 month then intermittently as needed. This superpotent steroid must be used with caution. • The non-steroidal anti-inflammatory agent tacrolimus ointment (Protopic) 0.1% may control vaginal and penile disease. It may be used for extended periods. • Acitretin (20–30 mg q.d. for 16 weeks) effective for severe vulvar disease.







