Chapter 40 Legg-Calve-Perthes Disease: How Should It Be Treated?
The necessity for evidenced-based investigation is nowhere better illustrated than in the case of the treatment of Legg–Calve–Perthes disease. In the United States, as well as around the world, an amazing variety of treatment methods are used for this condition. These vary from long-term relief from weight bearing, to months and months of abduction cast treatment, to combined femoral and pelvic surgical procedures, to ignoring the disease altogether. Even more striking is the degree with which orthopedists defend their chosen method.
Some years ago, I critically reviewed the literature up to 1994.1 Although much has been written since that date, some principles of importance came out of that review that apply specifically to Legg–Perthes disease.
STUDIES THAT REACH LEVEL I OR II
In 1993, Fulford, Lunn, and Macnicol’s2 comparison of 2 groups of patients randomized by source of referral was published. The children treated at Royal Hospital for Sick Children were compared with those treated at the Princess Margaret Rose Orthopaedic hospital. The children at the first hospital were treated with an ischial-bearing patten-ended caliper. Those at the second hospital had a varus, derotational proximal femoral osteotomy. This study can be considered a controlled, prospective study. The authors identified no differences in outcome between the groups. Outcome in their study was found to correlate with femoral head shape at presentation and the age at onset. They note that of the heads with severe deformity at the initial arthrogram, only 4 of 25 hips improved to have a good result, and all were younger than 5 years at onset. Two of these patients were receiving brace therapy, and two had surgery. Compared with historical control subjects, the authors believe that both methods are effective. Because of the wide variation in reporting of historical control subjects, I do not believe that such comparisons are useful in this disorder.
Harrison and Bassett3 performed a double-blind trial of pulsed electromagnetic field treatment in patients also being treated with a non–weight-bearing Birmingham orthosis. This study shows no discernible effect of the electromagnetic field treatment. The effectiveness of the orthosis was not elucidated by this study because the study did not include a control or comparative group.
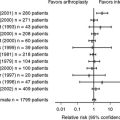
Herring and colleagues4 report on the results of a long-term, controlled study performed by the Legg Perthes Study Group. Thirty-nine pediatric orthopedists from North America and New Zealand agreed to a “best-effort” study in lieu of randomization. In this paradigm, each surgeon agreed to apply a single treatment method to each patient who met the study criteria. The presumption of this type of study is that so large a sample will likely override local selection factors and provide comparable treatment groups. The treatment groups were no treatment, range of motion treatment in which the patient did exercises once a day, Atlanta brace treatment, femoral varus osteotomy, and Salter innominate osteotomy. Within each treatment group, except the no treatment group, Petrie casts could be used up to two times to overcome hip stiffness.
Part one of the study provides detailed classifications that were tested in interobserver and intraobserver trials that showed good reliability5. The classifications evaluated were the lateral pillar classification in the early stages of disease and the Stulberg classification at skeletal maturity. The outcomes were analyzed relative to age at onset and severity of disease. Patients were managed to skeletal maturity and assessed independently by an observer not involved in patient treatment.
STUDIES WITH LESSER LEVELS OF EVIDENCE
Varus Osteotomy or Salter Osteotomy
Aksoy and colleagues6 retrospectively compared 23 patients receiving therapy with 26 hips not treated with braces or surgery. The patients’ ages were similar. No difference in outcome was found between the 2 groups, suggesting that brace treatment did not alter outcome. In this series, the braced group had 30% lateral pillar C hips compared with 18% in the nonbraced group. The authors found that the lateral pillar classification was useful in predicting outcome. The small numbers of patients in this study did not allow the authors to consider age at onset in the analysis. These issues limit the strength of the conclusions.
Aksoy and colleagues7 also evaluated the results of femoral varus osteotomy in 26 lateral pillar group C patients. Group C hips in patients older than 9 all had outcomes in Stulberg III, IV, and V categories. Six of 14 treated before age 9 had Stulberg II results. Their conclusion was that this surgery did not improve results for hips with lateral pillar group C involvement, especially if older than 9 when treated.
Friedlander and Weiner8 reviewed 116 hips treated with varus osteotomy without a control group. They found that those patients with lateral pillar B involvement had Stulberg I and II results in 86% when they were younger than 9 years at onset. Those older than 9 years with lateral pillar class B had Stulberg I and II results in 67% of cases. The hips of patients older than 9 years with lateral pillar C involvement had Stulberg II results in only 30% of cases. These results mirror those of Herring and colleagues4 but with better results for the group C hips in patients older than 9.
Grzegorzewski and colleagues9 retrospectively compared hips among five treatment groups, which included traction with abduction, Petrie casting, abduction bracing, pelvic osteotomy, and femoral osteotomy. They found that lateral pillar C hips fared less well than the others. They found no difference in outcome related to the treatment groups. They conclude that containment treatment was effective by any of the methods studied. The lack of a control group renders that conclusion unwarranted.
Ishida and colleagues10 reviewed results in 37 hips treated with Salter osteotomy without a control group. The younger patients fared better than the older patients. Those patients older than 7 years at onset had 3 Stulberg I or II, 10 Stulberg III, and 5 Stulberg IV results, but these were not stratified by lateral pillar classification.
Kim and coworkers11 report on a large, multicenter study of patients in Japan. They compared 6 treatment methods and found no difference in outcome among the groups. The lateral pillar classification and age at onset were the most important predictors of outcome. The overall outcome was similar to other studies in the Western literature.
Studies of Augmented Acetabuloplasty
Domzalski and colleagues demonstrated the occurrence of acetabular growth stimulation after a modified shelf arthroplasty in a Level III study.12 These hips were compared with hips treated with varus osteotomy. The authors hypothesize that the increase in acetabular depth will prevent hip subluxation and encourage acetabular growth. The stage of disease in which the operation was performed is not stated in the study. This study does not report or compare the Stulberg outcome between the 2 treatment groups. This omission leaves the clinical efficacy of this operation unproven.
Bursal and Erkula13 reviewed 19 hips without a control group and showed that acetabulum–head index and center-edge angles were improved. This finding, which is a direct effect of acetabular augmentation, appears in all studies of this operation. The clinical effectiveness of this change has not been demonstrated.
Jacobs and colleagues14 report on 43 hips treated with shelf acetabuloplasty. They show increased acetabular depth, but no comparative outcome data were presented.
Kuwajima and colleagues15 compare the Salter procedure with and without acetabular augmentation. Acetabular depth was improved, but outcome was similar between the 2 groups.
Studies of Valgus Osteotomy for Late Cases with Hinge Abduction
Bankes and colleagues16 found mixed results after valgus, extension osteotomy for hips with hinge abduction. Of 52 hips, 4 had total hip replacement and 1 had arthrodesis. Twelve had favorable remodeling. Younger hips, those in earlier stages of the disease, and those with open triradiate cartilages had better outcomes. No control data were presented.
Raney and colleagues17 also studied hips treated with valgus osteotomy for hinge abduction and pain. Twenty-one of 31 hips had Iowa hip scores averaging 93 points, but 10 failed to return for follow-up. No comparative group was studied.
Yoo and colleagues18 varied the extension and valgus of their osteotomy depending on the morphology of the involved hip. They report an improvement in the Iowa hip score from 66 before surgery to 92 after surgery. No control data were presented.
OTHER STUDIES
Fabry and colleagues19 report 36 hips in patients younger than 5 years at onset. They found that one third of patients had a poor result, and that the lateral pillar classification was useful in predicting outcome. Treatment methods were not related to outcome.
Rowe and colleagues20 studied the effect of cheilectomy in patients with Legg–Perthes disease over a 25-year follow-up. In this series, the extruded portion of the femoral head was excised in patients who had collapse of the femoral head and hinge abduction. Patients were between 9 and 11 years of age at onset. Early results showed improvement in range of motion and a decrease in symptoms. The 25-year follow-up showed 3 hips with poor results, 1 with fair results, and 1 with good outcome. All hips showed degenerative changes radiographically and patients were mildly symptomatic. This study is timely because femoral head reshaping procedures, usually done with surgical dislocation, are being done in a number of centers. The absence of a control group makes conclusions difficult. To the optimist, these hips responded better than they would have without treatment, whereas the pessimist concludes that they are still facing progressive degenerative arthropathy.
Maxwell and colleagues21 studied arthrodiastasis of the hip and compared the treated hips with a historical control group. The distraction treatment was done in the early phase of disease, before any collapse, in boys older than 8 and girls older than 7 years. One of 15 treated hips showed collapse, whereas 9 of 30 control hips collapsed. Pretreatment classification for severity was not done, and final outcome data were not available. Other studies of distraction treatment have focused on hips that have already had collapse with or without hinge abduction. In these patients, the operation is considered as salvage for severe disease.
SUMMARY
Studies with lesser levels of evidence have suggested benefit from acetabular augmentation surgery in early stages of disease. In later stages, benefit has been suggested for femoral valgus osteotomy and for joint distraction. Cheilectomy may provide short-term benefit, but long-term benefit is unproven. Table 40-1 provides a summary of recommendations.
TABLE 40-1 Summary of Recommendations for the Treatment of Legg–Calve–Perthes Disease
| STATEMENT | LEVEL OF EVIDENCE/GRADE OF RECOMMENDATION | REFERENCES |
|---|---|---|
1 Herring JA. The treatment of Legg-Calve-Perthes disease. A critical review of the literature. J Bone Joint Surg Am. 1994;76:448-458.
2 Fulford GE, Lunn PG, Macnicol MF. A prospective study of nonoperative and operative management for Perthes’ disease. J Pediatr Orthop. 1993;13:281-285.
3 Harrison MH, Bassett CA. The results of a double-blind trial of pulsed electromagnetic frequency in the treatment of Perthes’ disease. J Pediatr Orthop. 1997;17:264-265.
4 Herring JA, Kim HT, Browne R. Legg-Calve-Perthes disease. Part II: Prospective multicenter study of the effect of treatment on outcome. In: J Bone Joint Surg Am. 2004;86-A:2121-2134.
5 Herring J, Kim H, Browne R. Legg–Calve–Perthes disease: Part 1. Classification of radiographs with use of the modified lateral pillar and stulbereg classification. J Bone Joint Surg Am. 2004;26:2103.
6 Aksoy MC, Caglar O, Yazici M, Alpaslan AM. Comparison between braced and non-braced Legg-Calve-Perthes-disease patients: A radiological outcome study. J Pediatr Orthop B. 2004;13:153-157.
7 Aksoy MC, Cankus MC, Alanay A, et al. Radiological outcome of proximal femoral varus osteotomy for the treatment of lateral pillar group-C Legg-Calvé-Perthes disease. J Pediatr Orthop B. 2005;14:88-91.
8 Friedlander JK, Weiner DS. Radiographic results of proximal femoral varus osteotomy in Legg-Calve-Perthes disease. J Pediatr Orthop. 2000;20:566-571.
9 Grzegorzewski A, Bowen J, Guille J, Glutting J. Treatment of the collapsed femoral head by containment in Legg-Calve-Perthes disease. J Pediatr Orthop. 2003;23:15-19.
10 Ishida A, Kuwajima SS, Laredo Filho J, Milani C. Salter innominate osteotomy in the treatment of severe Legg-Calve-Perthes disease: Clinical and radiographic results in 32 patients (37 hips) at skeletal maturity. J Pediatr Orthop. 2004;24:257-264.
11 Kim WC, Hiroshima K, Imaeda T. Multicenter study for Legg-Calve-Perthes disease in Japan. J Orthop Sci. 2006;11:333-341.
12 Domzalski ME, Glutting J, Bowen JR, Littleton AG. Lateral acetabular growth stimulation following a labral support procedure in Legg-Calve-Perthes disease. J Bone Joint Surg Am. 2006;88:1458-1466.
13 Bursal A, Erkula G. Lateral shelf acetabuloplasty in the treatment of Legg-Calvé-Perthes disease. J Pediatr Orthop B. 2004;13:150-152.
14 Jacobs R, Moens P, Fabry G. Lateral shelf acetabuloplasty in the early stage of Legg-Calve-Perthes disease with special emphasis on the remaining growth of the acetabulum: A preliminary report. J Pediatr Orthop B. 2004;13:21-28.
15 Kuwajima SS, Crawford AH, Ishida A, et al. Comparison between Salter’s innominate osteotomy and augmented acetabuloplasty in the treatment of patients with severe Legg-Calve-Perthes disease. Analysis of 90 hips with special reference to roentgenographic sphericity and coverage of the femoral head. J Pediatr Orthop B. 2002;11:15-28.
16 Bankes MJ, Catterall A, Hashemi-Nejad A. Valgus extension osteotomy for ‘hinge abduction’ in Perthes’ disease. Results at maturity and factors influencing the radiological outcome. J Bone Joint Surg Br. 2000;82:548-554.
17 Raney EM, Grogan DP, Hurley ME, Ogden JA. The role of proximal femoral valgus osteotomy in Legg-Calve-Perthes disease. Orthopedics. 2002;25:513-517.
18 Yoo WJ, Choi IH, Chung CY, et al. Valgus femoral osteotomy for hinge abduction in Perthes’ disease. Decision-making and outcomes. J Bone Joint Surg Br. 2004;86:726-730.
19 Fabry K, Fabry G, Moens P. Legg-Calve-Perthes disease in patients under 5 years of age does not always result in a good outcome. Personal experience and meta-analysis of the literature. J Pediatr Orthop B. 2003;12:222-227.
20 Rowe SM, Jung ST, Cheon SY, et al. Outcome of cheilectomy in Legg-Calve-Perthes disease: Minimum 25-year follow-up of five patients. J Pediatr Orthop. 2006;26:204-210.
21 Maxwell SL, Lappin KJ, Kealey WD, et al. Arthrodiastasis in Perthes’ disease. Preliminary results. J Bone Joint Surg Br. 2004;86:244-250.