CHAPTER 83 Leg
This chapter describes the shafts of the tibia and fibula, the soft tissues that surround them and the interosseous membrane between them. The superior (proximal) and inferior (distal) tibiofibular joints are described in Chapters 82 and 84 respectively.
SKIN AND SOFT TISSUE
SKIN
Vascular supply and lymphatic drainage
The cutaneous arterial supply is derived from branches of the popliteal, anterior tibial, posterior tibial and fibular vessels (see Fig. 79.5). Multiple fasciocutaneous perforators from each vessel pass along intermuscular septa to reach the skin; musculocutaneous perforators traverse muscles before reaching the skin. In some areas there is an additional direct cutaneous supply from vessels that accompany cutaneous nerves, e.g. the descending genicular artery (saphenous artery) and superficial sural arteries. Fasciocutaneous and direct cutaneous branches have a longitudinal orientation in the skin, whereas the musculocutaneous branches are more radially oriented. For further details consult Cormack & Lamberty (1994).
SOFT TISSUE
Deep fascia
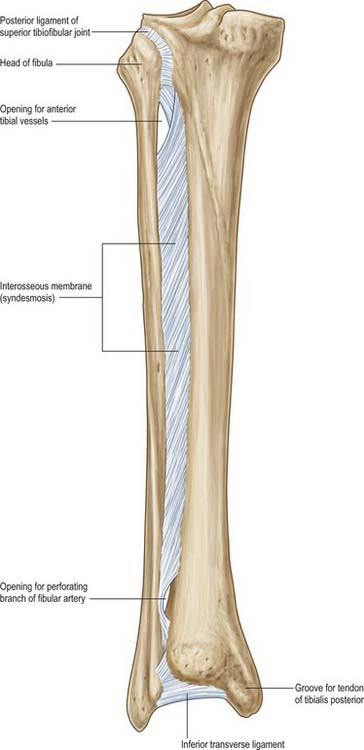
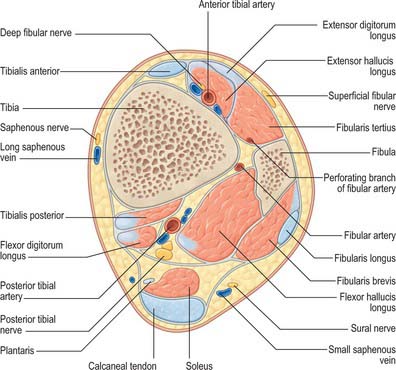
Interosseous membrane
The interosseous membrane connects the interosseous borders of the tibia and fibula (Fig. 83.1). It is interposed between the anterior and posterior groups of crural muscles; some members of each group are attached to the corresponding surface of the interosseous membrane. The anterior tibial artery passes forwards through a large oval opening near the proximal end of the membrane, and the perforating branch of the fibular artery pierces it distally. Its fibres are predominantly oblique and most descend laterally; those which descend medially include a bundle at the proximal border of the proximal opening. The membrane is continuous distally with the interosseous ligament of the distal tibiofibular joint. Tibialis anterior, extensor digitorum longus, extensor hallucis longus, fibularis tertius, the anterior tibial vessels and deep fibular nerve are all anterior to the membrane, and tibialis posterior and flexor hallucis longus are posterior.
Trauma and soft tissues of the leg
The relative paucity of soft tissue in the shin region and the subcutaneous position of the medial surface of the tibia means that even trivial soft tissue injury may lead to serious problems such as ulceration and osteomyelitis. In the elderly these soft tissues are often especially thin and unhealthy, reflecting the effects of ageing and venous stasis (see below). Tibial fractures are common in the young and, partly as a result of poor soft tissue coverage, they are often open injuries. Diminished blood supply to the bone, caused by traumatic stripping of attached soft tissues, and the risk of contamination add greatly to the risk of non-union and infection of the fracture. Healing of fractures at the junction of the middle and lower thirds of the tibia is compromised by the relatively poor blood supply to this region.
BONE
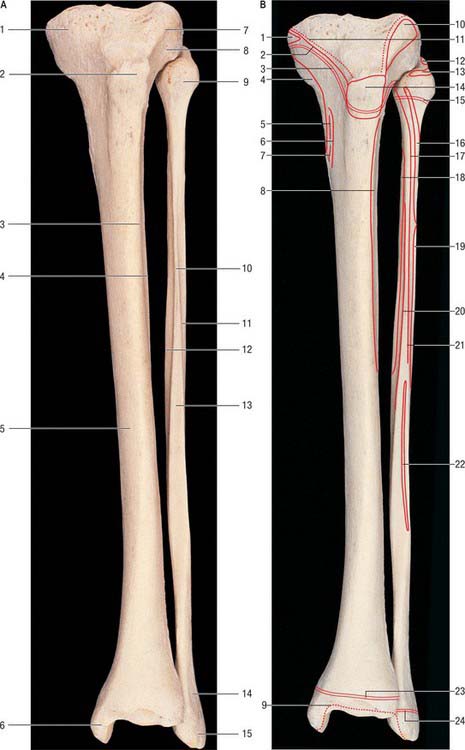
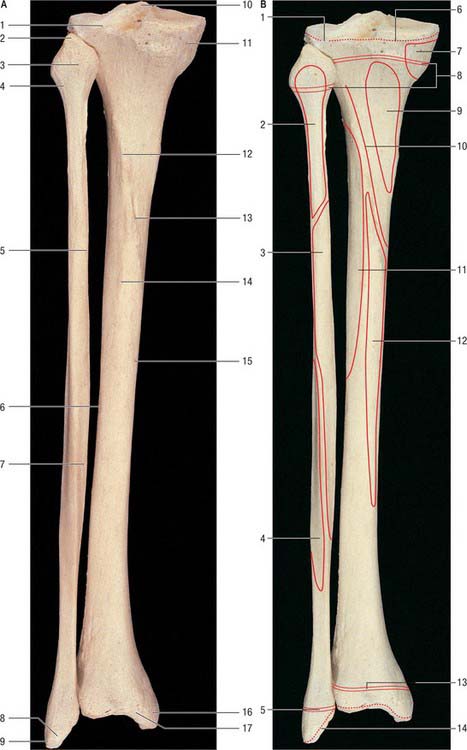
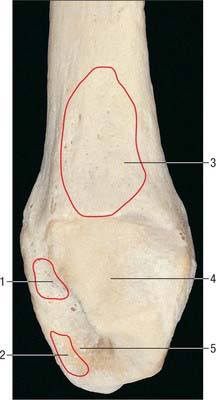
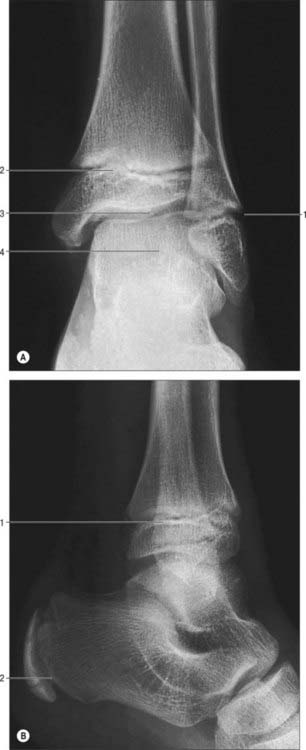
TIBIA
The tibia lies medial to the fibula and is exceeded in length only by the femur (Figs 83.2, 83.3). Its shaft is triangular in section and has expanded ends; a strong medial malleolus projects distally from the smaller distal end. The anterior border of the shaft is sharp and curves medially towards the medial malleolus. Together with the medial and lateral borders it defines the three surfaces of the bone. The exact shape and orientation of these surfaces show individual and racial variations.
Proximal end
The anterior condylar surfaces are continuous with a large triangular area whose apex is distal and formed by the tibial tuberosity. The lateral edge is a sharp ridge between the lateral condyle and lateral surface of the shaft. The condyles, their articular surfaces and the intercondylar area are described in Chapter 82.
The tibial tuberosity is the truncated apex of a triangular area where the anterior condylar surfaces merge. It projects only a little, and is divided into a distal rough and a proximal smooth region. The distal region is palpable and is separated from skin by the subcutaneous infrapatellar bursa. A line across the tibial tuberosity marks the distal limit of the proximal tibial growth plate (Fig. 83.2). The patellar tendon is attached to the smooth bone proximal to this, its superficial fibres reaching a rough area distal to the line. The deep infrapatellar bursa and fibroadipose tissue intervene between the bone and tendon proximal to its site of attachment. The latter may be marked distally by a somewhat oblique ridge, onto which the lateral fibres of the patellar tendon are inserted more distally than the medial fibres. (This knowledge is necessary to avoid damaging the tendon when sawing the tibia transversely just above the tibial tuberosity in a lateral to medial direction, e.g. in performing an osteotomy.) In habitual squatters a vertical groove on the anterior surface of the lateral condyle is occupied by the lateral edge of the patellar tendon in full flexion of the knee.
Shaft
The anteromedial surface, between the anterior and medial borders, is broad, smooth and almost entirely subcutaneous. The lateral surface, between the anterior and interosseous borders, is also broad and smooth. It faces laterally in its proximal three-fourths and is transversely concave. Its distal fourth swerves to face anterolaterally, on account of the medial deviation of the anterior and distal interosseous borders. This part of the surface is somewhat convex. The posterior surface, between the interosseous and medial borders, is widest above, where it is crossed distally and medially by an oblique, rough soleal line. A faint vertical line descends from the centre of the soleal line for a short distance before becoming indistinct. A large vascular groove adjoins the end of the line and descends distally into a nutrient foramen. Deep fascia and, proximal to the medial malleolus, the medial end of the superior extensor retinaculum, are attached to the anterior border. Posterior fibres of the medial collateral ligament and slips of semimembranosus and the popliteal fascia are attached to the medial border proximal to the soleal line, and some fibres of soleus and the fascia covering the deep calf muscles are attached distal to the line. The distal medial border runs into the medial lip of a groove for the tendon of tibialis posterior. The interosseous membrane is attached to the lateral border, except at either end of this border. It is indistinct proximally where a large gap in the membrane transmits the anterior tibial vessels. Distally the border is continuous with the anterior margin of the fibular notch, to which the anterior tibiofibular ligament is attached.
Distal end
The slightly expanded distal end of the tibia has anterior, medial, posterior, lateral and distal surfaces. It projects inferomedially as the medial malleolus. The distal end of the tibia, when compared to the proximal end, is laterally rotated (tibial torsion). The torsion begins to develop in utero and progresses throughout childhood and adolescence till skeletal maturity is attained. Tibial torsion is approximately 30° in Caucasian and Asian populations, but is significantly greater in people of African origin (Eckhoff et al 1994). Some of the femoral neck anteversion seen in the newborn may persist in adult females: this causes the femoral shaft and knee to be internally rotated, and the tibia may develop a compensatory external torsion to counteract the tendency of the feet to turn inwards.
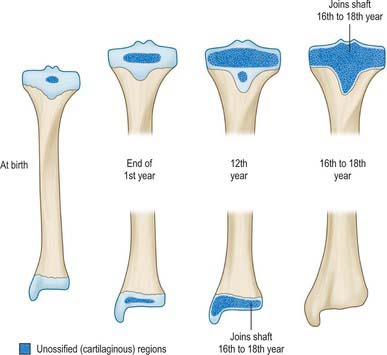
Ossification
The tibia ossifies from three centres, one in the shaft and one in each epiphysis. Ossification (Figs 83.2, 83.3, 83.4; see Fig. 82.6) begins in midshaft at about the seventh intrauterine week. The proximal epiphysial centre is usually present at birth: at approximately 10 years a thin anterior process from the centre descends to form the smooth part of the tibial tuberosity. A separate centre for the tuberosity may appear at about the twelfth year and soon fuses with the epiphysis. Distal strata of the epiphysial plate are composed of dense collagenous tissue in which the fibres are aligned with the patellar tendon. Exaggerated traction stresses may account for Osgood–Schlatter disease, where fragmentation of the epiphysis of the tuberosity occurs during adolescence and produces a painful swelling in the region of the tuberosity. Healing occurs once the growth plate fuses, leaving a bony protrusion. Prolonged periods of traction with the knee extended, both in children and adolescents, can lead to growth arrest of the anterior part of the proximal epiphysis, which results in bowing of the proximal tibia as the posterior tibia continues to grow. The proximal epiphysis fuses in the 16th year in females and the 18th in males. The distal epiphysial centre appears early in the first year and joins the shaft at about the 15th year in females and the 17th in males. The medial malleolus is an extension from the distal epiphysis and starts to ossify in the seventh year: it may have its own separate ossification centre. In 47% of females and 17% of males, an accessory ossification centre appears at the tip of the medial malleolus which fuses during the eighth year in females and the ninth in males: it should not be confused with an os subtibiale, which is a rare accessory bone found on the posterior aspect of the medial malleolus.
FIBULA
The fibula (Figs 83.2, 83.3) is much more slender than the tibia and is not directly involved in transmission of weight. It has a proximal head, a narrow neck, a long shaft and a distal lateral malleolus. The shaft varies in form, being variably moulded by attached muscles: these variations may be confusing.
Shaft
The lateral surface, between the anterior and posterior borders and associated with the fibular muscles, faces laterally in its proximal three-fourths. The distal quarter spirals posterolaterally to become continuous with the posterior groove of the lateral malleolus. The anteromedial (sometimes simply termed anterior, or medial) surface, between the anterior and interosseous borders, usually faces anteromedially but often directly anteriorly. It is associated with the extensor muscles. Though wide distally, it narrows in its proximal half and may become a mere ridge. The posterior surface, between the interosseous and posterior borders, is the largest and is associated with the flexor muscles. Its proximal two-thirds is divided by a longitudinal medial crest, separated from the interosseous border by a grooved surface that is directed medially. The remaining surface faces posteriorly in its proximal half; its distal half curves onto the medial aspect. Distally this area occupies the fibular notch of the tibia, which is roughened by the attachment of the principal interosseous tibiofibular ligament. The triangular area proximal to the lateral surface of the lateral malleolus is subcutaneous; muscles cover the rest of the shaft.
Lateral malleolus
The distal end forms the lateral malleolus which projects distally and posteriorly (Figs 83.2, 83.3, 83.5). Its lateral aspect is subcutaneous while its posterior aspect has a broad groove with a prominent lateral border. Its anterior aspect is rough, round and continuous with the tibial inferior border. The medial surface has a triangular articular facet, vertically convex, its apex distal, which articulates with the lateral talar surface. Behind this facet is a rough malleolar fossa pitted by vascular foramina. The posterior tibiofibular ligament and, more distally, the posterior talofibular ligament, are attached in the fossa. The anterior talofibular ligament is attached to the anterior surface of the lateral malleolus; the calcaneofibular ligament is attached to the notch anterior to its apex. The tendons of fibularis brevis and longus groove its posterior aspect: the latter is superficial and covered by the superior fibular retinaculum.
Muscle attachments
Muscle attachments to the posterior surface, which is divided longitudinally by the medial crest, are complex. Between the crest and interosseous border the posterior surface is concave. Tibialis posterior is attached throughout most (the proximal three-fourths) of this area; an intramuscular tendon may ridge the bone obliquely. Soleus is attached between the crest and the posterior border on the proximal fourth of the posterior surface; its tendinous arch is attached to the surface proximally. Flexor hallucis longus is attached distal to soleus on the posterior surface and almost reaches the distal end of the shaft.
Ossification
The fibula ossifies from three centres, one each for the shaft and the extremities (Fig. 83.6). The process begins in the shaft at about the eighth intrauterine week, in the distal end in the first year, and in the proximal end at about the third year in females and the fourth in males. The distal epiphysis unites with the shaft at about the 15th year in females and the 17th in males, whereas the proximal epiphysis does not unite until about the 17th year in females and the 19th in males‥ An os subfibulare is an occasional and separate entity and lies posterior to the tip of the fibula, whereas the distal fibular apophysis lies anteriorly. An os retinaculi is rarely encountered; if present, it overlies the bursa of the distal fibula within the fibular retinaculum.
MUSCLES
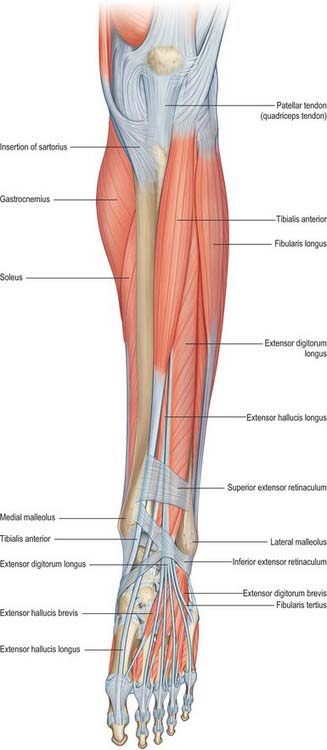
ANTERIOR OR EXTENSOR COMPARTMENT
The anterior compartment contains muscles that dorsiflex the ankle when acting from above (Figs 83.7, 83.8, 83.9). When acting from below they pull the body forward on the fixed foot during walking. Two of the muscles, extensor digitorum longus and extensor hallucis longus, also extend the toes, and two muscles, tibialis anterior and fibularis tertius, have the additional actions of inversion and eversion respectively.
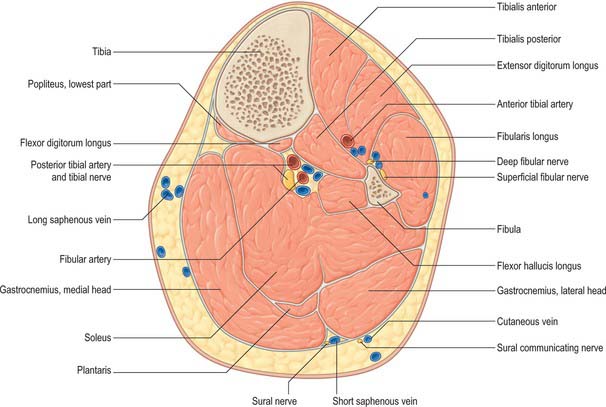
Fig. 83.8 Transverse (axial) section through the left leg, approximately 10 cm distal to the knee joint.
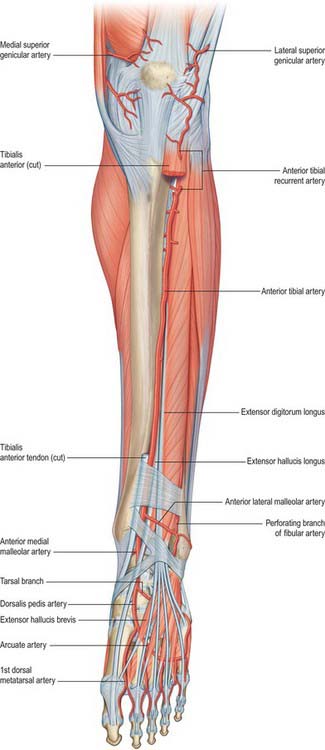
Fig. 83.9 The left anterior tibial and dorsalis pedis arteries. To expose the anterior tibial artery a large part of tibialis anterior has been excised and extensor hallucis longus is retracted laterally. Compare with Fig. 83.7.
Tibialis anterior
Tibialis anterior is a dorsiflexor of the ankle joint and invertor of the foot. It is most active when both movements are combined, as in walking. Its tendon can be seen through the skin lateral to the anterior border of the tibia and can be traced downwards and medially across the front of the ankle to the medial side of the foot. Tibialis anterior elevates the first metatarsal base and medial cuneiform and rotates their dorsal aspects laterally.
Extensor digitorum longus
Extensor digitorum longus arises from the inferior surface of the lateral condyle of the tibia, proximal three-quarters of the medial surface of the fibula, adjacent anterior surface of the interosseous membrane, deep surface of the deep fascia, anterior crural intermuscular septum, and from the fascial septum between itself and tibialis anterior. These origins form the walls of an osseo-aponeurotic tunnel. Extensor digitorum longus becomes tendinous at about the same level as tibialis anterior, and the tendon passes deep to the superior extensor retinaculum and within a loop of the inferior extensor retinaculum with fibularis tertius (see Figs 83.7, 84.2). It divides into four slips which run forward on the dorsum of the foot and are attached in the same way as the tendons of extensor digitorum in the hand. At the metatarsophalangeal joints the tendons to the second, third and fourth toes are each joined on the lateral side by a tendon of extensor digitorum brevis. The dorsal digital expansions thus formed on the dorsal aspects of the proximal phalanges, as in the fingers, receive contributions from the appropriate lumbrical and interosseous muscles. The expansion narrows as it approaches a proximal interphalangeal joint, and divides into three slips. These are a central (axial) slip, attached to the base of the middle phalanx, and two collateral (coaxial) slips, which reunite on the dorsum of the middle phalanx and are attached to the base of the distal phalanx.
Fibularis tertius
Fibularis tertius (peroneus tertius) is a muscle unique to humans. It often appears to be part of extensor digitorum longus, and might be described as its ‘fifth tendon’. The muscle fibres of fibularis tertius arise from the distal third or more of the medial surface of the fibula, the adjoining anterior surface of the interosseous membrane, and the anterior crural intermuscular septum. The tendon passes deep to the superior extensor retinaculum and within the loop of the inferior extensor retinaculum alongside the extensor digitorum longus (see Figs 83.7, 84.2). It is inserted into the medial part of the dorsal surface of the base of the fifth metatarsal bone; a thin expansion usually extends forwards along the medial border of the shaft of the bone.
Electromyographic studies show that during the swing phase of gait (see Fig. 84.26), fibularis tertius acts with extensor digitorum longus and tibialis anterior to produce dorsiflexion of the foot, and with fibularis longus and fibularis brevis to effect eversion of the foot (Jungers et al 1993). This levels the foot and helps the toes to clear the ground, an action that improves the efficiency and enhances the economy of bipedal locomotion. Fibularis tertius is not active during the stance phase, a finding that is at variance with the suggestion that the muscle acts primarily to support the lateral longitudinal arch and to transfer the centre of pressure of the foot medially.
LATERAL (FIBULAR OR PERONEAL) COMPARTMENT
The lateral compartment contains fibularis (peroneus) longus and fibularis (peroneus) brevis (Figs 83.7, 83.8). Both muscles evert the foot and are plantar flexors of the ankle, and both probably play a part in balancing the leg on the foot in standing and walking.
Fibularis longus
Fibularis longus is the more superficial of the two muscles of the lateral compartment. It arises from the head and proximal two-thirds of the lateral surface of the fibula, the deep surface of the deep fascia, the anterior and posterior crural intermuscular septa, and occasionally by a few fibres from the lateral condyle of the tibia. The muscle belly ends in a long tendon that runs distally behind the lateral malleolus in a groove it shares with the tendon of fibularis brevis. The groove is converted into a canal by the superior fibular retinaculum, so that the tendon of fibularis longus, and that of fibularis brevis which lies in front of the longus tendon, are contained in a common synovial sheath. If the fibular retinaculum is ruptured by injury and fails to heal, the tendons can dislocate from the groove. The fibularis longus tendon runs obliquely forwards on the lateral side of the calcaneus, below the fibular trochlea and the tendon of fibularis brevis, and deep to the inferior fibular retinaculum. It crosses the lateral side of the cuboid and then runs under the cuboid in a groove that is converted into a canal by the long plantar ligament (see Fig. 84.19). It crosses the sole of the foot obliquely and is attached by two slips, one to the lateral side of the base of the first metatarsal bone and one to the lateral aspect of the medial cuneiform; occasionally a third slip is attached to the base of the second metatarsal bone. The tendon changes direction below the lateral malleolus and on the cuboid bone. At both sites it is thickened and at the second a sesamoid fibrocartilage (sometimes a bone, the os peroneum) is usually present. A second synovial sheath invests the tendon as it crosses the sole of the foot.
Vascular supply of lateral compartment
Usually the predominant supply of the lateral compartment muscles is derived from superior and inferior branches of the anterior tibial artery; the superior is commonly the larger. There is also a lesser, variable, contribution from the fibular artery in the distal part of the leg. A fibular branch may replace the inferior branch of the anterior tibial artery; less commonly the fibular artery provides the main supply to the whole compartment. The upper part of fibularis longus is also supplied by the circumflex fibular artery, which is usually a branch of the anterior tibial artery. The companion artery to the common fibular nerve, a branch of the popliteal artery, provides a minor contribution proximally. Distally the tendons are supplied by the fibular perforating, anterior lateral malleolar, lateral calcaneal, lateral tarsal, arcuate, lateral and medial plantar arteries (see Fig. 84.9).
Fibularis brevis
Anteriorly lie extensor digitorum longus and fibularis tertius. Fibularis longus and flexor hallucis longus are posterior. On the lateral surface of the calcaneus the tendons of fibularis longus and fibularis brevis occupy separate osteofascial canals formed by the calcaneus and the inferior fibular retinaculum; each tendon is enveloped in a separate distal prolongation of the common synovial sheath (see Fig. 84.2).
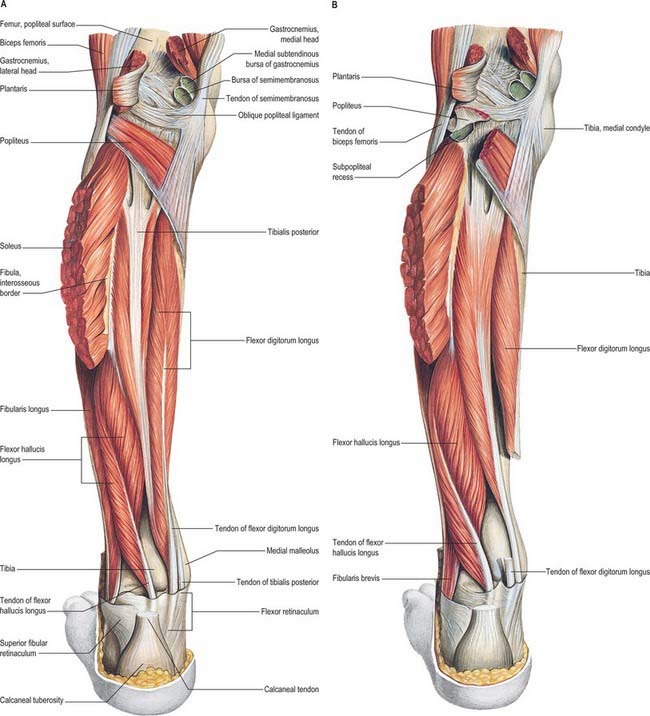
POSTERIOR (FLEXOR) COMPARTMENT
Superficial flexor group
The superficial flexors gastrocnemius, plantaris and soleus (Figs 83.8, 83.10; see Figs 82.2, 80.25) form the bulk of the calf. Gastrocnemius and soleus, collectively known as the triceps surae, constitute a powerful muscular mass whose main function is plantar flexion of the foot, although soleus in particular has an important postural role (see below). Their large size is a defining human characteristic, and is related to the upright stance and bipedal locomotion of the human. Gastrocnemius and plantaris act both on the knee and ankle joints; soleus on the latter alone.
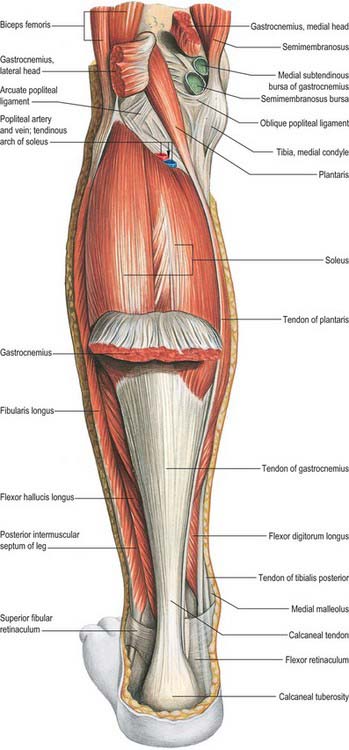
Fig. 83.10 Muscles of the left leg, posterior aspect. Gastrocnemius partially removed.
(From Sobotta 2006.)
Gastrocnemius
Gastrocnemius is the most superficial muscle of the group and forms the ‘belly’ of the calf. It arises by two heads, connected to the condyles of the femur by strong, flat tendons. The medial, larger, head is attached to a depression at the upper and posterior part of the medial condyle behind the adductor tubercle, and to a slightly raised area on the popliteal surface of the femur just above the medial condyle. The lateral head is attached to a recognizable area on the lateral surface of the lateral condyle and to the lower part of the corresponding supracondylar line. Both heads also arise from subjacent areas of the capsule of the knee joint. The tendinous attachments expand to cover the posterior surface of each head with an aponeurosis, from the anterior surface of which the muscle fibres arise. The fleshy part of the muscle extends to about midcalf. The muscle fibres of the larger medial head extend lower than those of the lateral head. As the muscle descends, the muscle fibres begin to insert into a broad aponeurosis that develops on its anterior surface; up to this point the muscular masses of the two heads remain separate. The aponeurosis gradually narrows and receives the tendon of soleus on its deep surface to form the calcaneal tendon (for a detailed description of the calcaneal tendon see Ch. 84).
Each head of gastrocnemius is supplied by its own sural artery. These arteries are branches of the popliteal artery, and arise at variable levels, usually at the level of the tibiofemoral joint line. The medial sural artery almost always arises more proximally than the lateral: the medial may arise proximal to the joint line, the lateral sometimes distal to the line. Each sural artery enters the corresponding muscle head with its nerve of supply, the pedicle entering the muscle near its axial border at the level of the middle of the popliteal fossa. Medial or lateral gastrocnemius musculocutaneous flaps may be raised, each based on its neurovascular pedicle. Minor accessory sural arteries arise from the popliteal or from the superior genicular vessels.
The blood supply to the calcaneal tendon is described in Chapter 84.
Actions of triceps surae
Gastrocnemius and soleus are the chief plantar flexors of the foot; gastrocnemius is also a flexor of the knee. The muscles are usually large and correspondingly powerful. Gastrocnemius provides force for propulsion in walking, running and leaping. Soleus, acting from below, is said to be more concerned with steadying the leg on the foot in standing. This postural role is also suggested by its high content of slow, fatigue-resistant (type 1) muscle fibres. In many adult mammals the proportion of this type of fibre in soleus approaches 100%. However, such a rigid separation of functional roles seems unlikely in man: soleus probably participates in locomotion, and gastrocnemius in posture. Nevertheless, the ankle joint is loose-packed in the erect posture, and since the weight of the body acts through a vertical line that passes anterior to the joint, a strong brace is required behind the joint to maintain stability. Electromyography shows that these forces are supplied mainly by soleus: during symmetrical standing, soleus is continuously active, whereas gastrocnemius is recruited only intermittently. The relative contributions of soleus and gastrocnemius to phasic activity of the triceps surae in walking have yet to be satisfactorily analysed.
Deep flexor group
The deep flexor group (Fig. 83.8, Fig. 83.11), lies beneath (anterior to) the deep transverse fascia, and consists of popliteus, which acts on the knee joint, and flexor digitorum longus, flexor hallucis longus and tibialis posterior, which all produce plantar flexion at the ankle in addition to their specific actions on joints of the foot and digits.
Flexor digitorum longus
Flexor digitorum longus is thin and tapered proximally, but widens gradually as it descends. It arises from the posterior surface of the tibia medial to tibialis posterior from just below the soleal line to within 7 or 8 cm of the distal end of the bone; it also arises from the fascia covering tibialis posterior. The muscle ends in a tendon that extends along almost the whole of its posterior surface. The tendon gradually crosses tibialis posterior on its superficial aspect and passes behind the medial malleolus where it shares a groove with tibialis posterior, from which it is separated by a fibrous septum, i.e. each tendon occupies its own compartment lined by a synovial sheath. The tendon of flexor digitorum longus then curves obliquely forwards and laterally, in contact with the medial side of the sustentaculum tali, passes deep to the flexor retinaculum, and enters the sole of the foot on the medial side of the tendon of flexor hallucis longus (see Fig. 84.18). It crosses superficial to that tendon and receives a strong slip from it (and may also send a slip to it). The tendon of flexor digitorum longus then passes forward as four separate tendons, one each for the second to fifth toes, deep to the tendons of flexor digitorum brevis. After giving off the lumbricals, it passes through the fibrous sheaths of the lateral four toes. The tendons of flexor accessorius insert into the long flexor tendons of the second, third and fourth digits; flexor hallucis longus makes a variable contribution through the connecting slip mentioned above. The long flexor tendons of the lateral four digits are attached to the plantar surfaces of the bases of their distal phalanges; each passes between the slips of the corresponding tendon of flexor digitorum brevis at the base of the proximal phalanx.
Flexor hallucis longus
Flexor hallucis longus arises from the distal two-thirds of the posterior surface of the fibula (except for the lowest 2.5 cm of this surface); the adjacent interosseous membrane and the posterior crural intermuscular septum; and from the fascia covering tibialis posterior, which it overlaps to a considerable extent. Its fibres pass obliquely down to a tendon that occupies nearly the whole length of the posterior aspect of the muscle. This tendon grooves the posterior surface of the lower end of the tibia, then, successively, the posterior surface of the talus and the inferior surface of the sustentaculum tali of the calcaneus (see Fig. 84.2B). Fibrous bands convert the grooves on the talus and calcaneus into a canal lined by a synovial sheath. In dancers, overuse causes thickening of the tendon in this region, and pain and even ‘triggering’ can occur (hallux saltans). In the sole of the foot, the tendon of flexor hallucis longus passes forward in the second layer (Ch. 84) like a bowstring. It crosses the tendon of flexor digitorum longus from lateral to medial, curving obliquely superior to it. At the crossing point (knot of Henry) it gives off two strong slips to the medial two divisions of the tendons of flexor digitorum longus and then crosses the lateral part of flexor hallucis brevis to reach the interval between the sesamoid bones under the head of the first metatarsal. It continues on the plantar aspect of the hallux, and runs in an osseo-aponeurotic tunnel to be attached to the plantar aspect of the base of the distal phalanx. The tendon is retained in position over the lateral part of flexor hallucis brevis by the diverging stems of the distal band of the medial intermuscular septum.
Tibialis posterior
Tibialis posterior is the most deeply placed muscle of the flexor group. At its origin it lies between flexor hallucis longus and flexor digitorum longus, and is overlapped by both, but especially by the former. Its proximal attachment consists of two tapered processes, separated by an angular interval that is traversed by the anterior tibial vessels. The medial process arises from the posterior surface of the interosseous membrane, except at its most distal part, and from a lateral area on the posterior surface of the tibia between the soleal line above and the junction of the middle and lower thirds of the shaft below. The lateral part arises from a medial strip of the posterior fibular surface in its upper two-thirds. The muscle also arises from the deep transverse fascia, and from the intermuscular septa that separate it from adjacent muscles. In the distal quarter of the leg its tendon passes deep to that of flexor digitorum longus, with which it shares a groove behind the medial malleolus, each enclosed in a separate synovial sheath. It then passes deep to the flexor retinaculum and superficial to the deltoid ligament to enter the foot. In the foot it is at first inferior to the plantar calcaneonavicular ligament, where it contains a sesamoid fibrocartilage. The tendon then divides into two. The more superficial and larger division, which is a direct continuation of the tendon, is attached to the tuberosity of the navicular, from which fibres continue to the inferior surface of the medial cuneiform. A tendinous band also passes laterally and a little proximally to the tip and distal margin of the sustentaculum tali. The deeper lateral division gives rise to the tendon of origin of the medial limb of flexor hallucis brevis, and then continues between this muscle and the navicular and medial cuneiform to end on the intermediate cuneiform and the bases of the second, third and fourth metatarsals; the slip to the fourth metatarsal is the strongest.
VASCULAR SUPPLY
ARTERIES
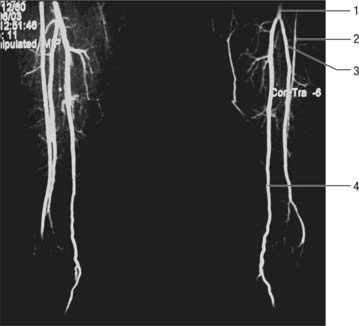
Anterior tibial artery
The anterior tibial artery arises at the distal border of popliteus (Figs 83.9, 83.12, 83.13; see Figs 82.1, 82.4, 84.9). At first in the flexor compartment, it passes between the heads of tibialis posterior and through the oval aperture in the proximal part of the interosseous membrane to reach the extensor (anterior) compartment, passing medial to the fibular neck: it is vulnerable here during tibial osteotomy. Descending on the anterior aspect of the membrane it approaches the tibia and, distally, lies anterior to it. At the ankle the anterior tibial artery is midway between the malleoli, and it continues on the dorsum of the foot as the dorsalis pedis artery.
Posterior tibial artery
The posterior tibial artery begins at the distal border of popliteus, between the tibia and fibula (Fig. 83.13; see Figs 82.1, 82.4). It descends medially in the flexor compartment and divides under abductor hallucis, midway between the medial malleolus and the medial tubercle of the calcaneus, into the medial and lateral plantar arteries. The artery may be much reduced in length or in calibre: the fibular artery then takes over its distal territory of supply and may consequently be increased in size.
Medial plantar artery
The medial plantar artery is the smaller terminal branch of the posterior tibial artery and passes distally along the medial side of the foot, medial to the medial plantar nerve (see Fig. 84.24). At first deep to abductor hallucis, it runs distally between this muscle and flexor digitorum brevis, and supplies both. Near the first metatarsal base, its size, already diminished by muscular branches, is further reduced by a superficial stem that divides to form three superficial digital branches. These accompany the digital branches of the medial plantar nerve and join the first to third plantar metatarsal arteries. The main trunk of the medial plantar artery then runs on to reach the medial border of the hallux, where it anastomoses with a branch of the first plantar metatarsal artery.
Lateral plantar artery
The lateral plantar artery is the larger terminal branch of the posterior tibial artery (see Fig. 84.24). It passes distally and laterally to the fifth metatarsal base, lateral to the lateral plantar nerve. (The medial and lateral plantar nerves lie between the corresponding plantar arteries.) Turning medially with the deep branch of the lateral plantar nerve, it reaches the interval between the first and second metatarsal bases, and unites with the dorsalis pedis artery to complete the plantar arch. As it passes laterally, it is first between the calcaneus and abductor hallucis, then between flexor digitorum brevis and flexor accessorius. Running distally to the fifth metatarsal base, it passes between flexor digitorum brevis and abductor digiti minimi and is covered by the plantar aponeurosis, superficial fascia and skin.
Fibular artery
The fibular artery arises from the posterior tibial artery approximately 2.5 cm distal to popliteus and passes obliquely to the fibula, descending along its medial crest either in a fibrous canal between tibialis posterior and flexor hallucis longus or within flexor hallucis longus (Figs 83.9, 83.12, 83.13; see Fig. 82.4). Reaching the inferior tibiofibular syndesmosis, it divides into calcaneal branches that ramify on the lateral and posterior surfaces of the calcaneus. Proximally it is covered by soleus and the deep transverse fascia between soleus and the deep muscles of the leg, and distally it is overlapped by flexor hallucis longus.
The fibular artery may branch high from the posterior tibial artery or may even branch from the popliteal artery separately, giving a true ‘trifurcation’. It may also branch more distally from the posterior tibial artery, sometimes 7 or 8 cm distal to popliteus. Its size tends to be inversely related to the size of the other arteries of the leg. It may be reduced in size but is more often enlarged, when it may join, reinforce or even replace the posterior tibial artery in the distal leg and foot. An enlarged perforating branch may replace the dorsalis pedis artery: the dorsalis pedis pulse will then be absent.
Branches
The fibular artery has muscular, nutrient, perforating, communicating and calcaneal branches.
Perforator flaps in the knee and leg
The perforators which arise from the rich vascular anastomosis around the patella generally traverse the quadriceps tendon to supply the skin over the patella and the peri-patellar region (see Fig. 79.7). The skin flaps based on these perforators may be used as distally based or proximally based flaps to cover defects over the knee and popliteal region. The direct cutaneous branch of the popliteal artery and a superficial sural artery which accompanies the sural nerve provide additional perforators to the skin over the back of the knee. The posterior tibial artery gives out an average of ten perforators to the skin covering the anteromedial and posterior parts of the leg. In the upper third of the leg the perforating vessels are predominantly muscular and periosteocutaneous, while in the lower third, the perforating vessels are mainly direct subcutaneous types. They anastomose with the perforating branches of the anterior tibial artery anteriorly and fibular artery posteriorly. Inferiorly, the posterior tibial artery forms a rich anastomotic circle around the ankle joint with the fibular and anterior tibial arteries. Perforators from these vessels supply the calcaneal tendon and the overlying skin. The posterior tibial artery gives off three direct cutaneous perforators in the lower part of the leg: a distally based skin or adipo-fascial flap based on one of these perforators may be used to reconstruct a defect over the anterior or the posterior aspect of the lower leg. The anterior tibial artery gives off an average of six perforators which supply the antero-lateral part of the leg. They emerge in two longitudinal rows; one perforator is fairly large and accompanies the superficial fibular nerve. A small skin flap based on any one of these perforators may be used to cover small defects over the tibia and a neurocutaneous flap that includes the superficial fibular nerve may be used.
DEEP AND SUPERFICIAL VENOUS SYSTEM
Posterior tibial veins
The posterior tibial veins accompany the posterior tibial artery (see Fig. 79.8). They receive tributaries from the calf muscles (especially from the venous plexus in the soleus) and connections from superficial veins and the fibular veins.
Long and short saphenous vein
The long and short saphenous veins are described on pages 1381 and 1409.
INNERVATION
Tibial nerve
The tibial nerve, the larger component of the sciatic nerve (see Chs 79 & 80), is derived from the ventral branches (anterior divisions) of the fourth and fifth lumbar and first to third sacral ventral rami. It descends along the back of the thigh and popliteal fossa to the distal border of popliteus. It then passes anterior to the arch of soleus with the popliteal artery and continues into the leg. In the thigh it is overlapped proximally by the hamstring muscles but it becomes more superficial in the popliteal fossa, where it is lateral to the popliteal vessels. At the level of the knee the tibial nerve becomes superficial to the popliteal vessels and crosses to the medial side of the artery. In the distal popliteal fossa it is overlapped by the junction of the two heads of gastrocnemius.
Branches
The branches of the tibial nerve are articular, muscular, sural, medial calcaneal and medial and lateral plantar nerves. The medial and lateral plantar nerves are described in Chapter 84.
Common fibular nerve
Superficial fibular nerve
The superficial fibular nerve (superficial fibular nerve) begins at the bifurcation of the common fibular nerve. It lies at first deep to fibularis longus, then passes anteroinferiorly between fibularis longus and brevis and extensor digitorum longus and pierces the deep fascia in the distal third of the leg. It divides into a large medial dorsal cutaneous nerve and a smaller, more laterally placed, intermediate dorsal cutaneous nerve, usually after piercing the crural fascia, but sometimes while it is still deep to the fascia. As the nerve lies between the muscles it supplies fibularis longus, fibularis brevis and the skin of the lower leg. The deep course, i.e. the compartmental localization, and the peripheral digital distribution of the superficial fibular nerve are subject to considerable variation (see Kosinksi’s classification; Kosinski 1926; Solomon et al 2001).
Cormack GC, Lamberty BGH 1994; See Bibliography.
Eckhoff DG, Kramer RC, Watkins JJ, Burke BJ, Alongi CA, Stamm ER, van Gerven DP. Variation in tibial torsion. Clin Anat. 1994;7:76-79.
Jungers WL, Meldrum DJ, Stern JTJr. The functional and evolutionary significance of the human peroneus tertius muscle. J Hum Evol. 1993;25:377-386.
Kosinksi C. The course, mutual relations and distribution of the cutaneous nerves of the metazonal regions of the leg and foot. J Anat Physiol. 1926;60:274-297.
Solomon LB, Ferris L, Tedman R, Henneberg M. Surgical anatomy of the sural and superficial fibular nerves with an emphasis on the approach to the lateral malleolus. J Anat. 2001;199:717-723.
Michael Salmon: Anatomic Studies. In: Taylor GI, Razaboni RM. Book 1, Arteries of the Muscles of the Extremities and the Trunk. St Louis: Quality Medical Publishing, 1994.