CHAPTER 22 Left colon resection (medial to lateral approach)
Step 1. Surgical anatomy
♦ The left colon receives arterial input via the inferior mesenteric artery (IMA). Soon after its takeoff from the abdominal aorta, the IMA branches into a left (descending) colic branch and the superior hemorrhoidal artery (SHA). The SHA continues down to the rectum, along the way giving off sigmoidal branches.
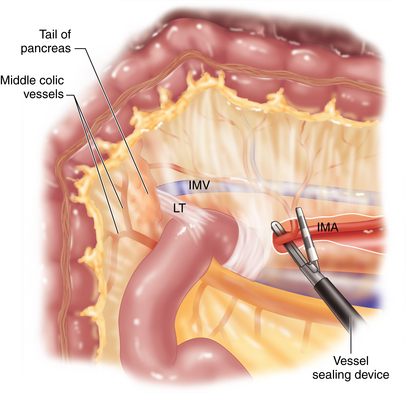
♦ The venous drainage of the left colon is into the inferior mesenteric vein (IMV), which passes posterolateral to the IMA, parallel to the aorta in a cephalad direction, to pass under the tail of the pancreas where it joins the splenic vein.
♦ The lymphatic drainage follows the arteries.
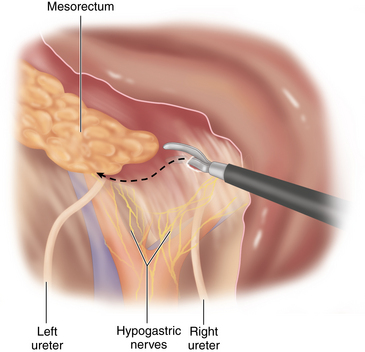
♦ The sympathetic plexus interdigitates around the aorta at the base of the IMA, then it coalesces into the left and right hypogastric nerves as they course over the common iliacs and into the pelvis.
♦ The left ureter and gonadal vessels lie in the retroperitoneum posterior to the left colon mesentery.
Step 2. Preoperative considerations
Room setup and patient positioning
♦ Following induction of general endotracheal anesthesia, the patient is placed in a neutral lithotomy position on a well-padded electric operating room table.
♦ Shoulders, hips and knees should be in the same plane. Arms are carefully padded and tucked at the sides using an oversized beanbag or tucked with sheets. Chest straps or tapes may be placed for added security.
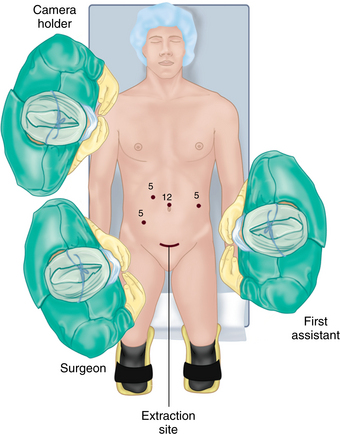
♦ The surgeon and camera operator stand on the patient’s right, assistant on the left (Figure 22-1).
Step 3. Operative steps
Access and port placement
♦ Following port placement, laparoscopic exploration and any necessary adhesiolysis, the patient is placed in a steep Trendelenburg position with the right side tilted down.
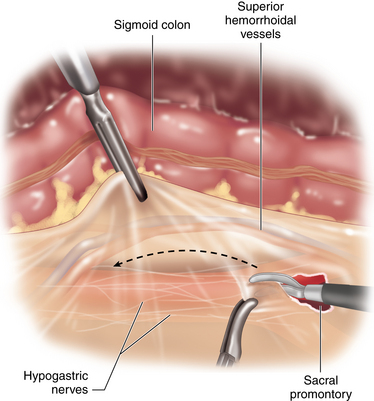
Establish plane between the superior hemorrhoidal artery and the sacral promontory:
♦ The small bowel is swept up out of the pelvis and off to the right upper quadrant. The base of the medial (right side of the sigmoid) mesentery over the sacral promontory is exposed by placing the sigmoid mesocolon on anterolateral traction toward the left. The peritoneum over the root of the sigmoid mesentery is scored parallel to and just posterior to the arc of the superior hemorrhoidal artery as it courses over the sacral promontory. This is extended from the sacral hollow up to the root of the IMA (Figure 22-2).
♦ With a gentle blunt anterior to posterior sweeping motion, the areolar, avascular retroperitoneal plane is created. The hypogastric nerves are identified and preserved posteriorly.
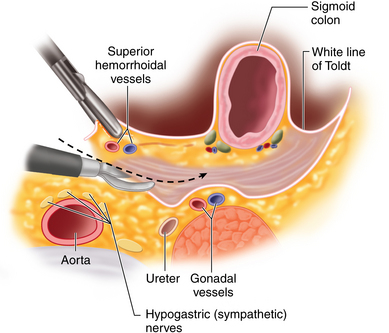
♦ Once established, the purplish areolar plane between the sigmoid colon mesentery and the retroperitoneal structures is swept down. This creates a “cave,” which will be deepened up and out to the lateral abdominal sidewall. The left ureter should be identified just lateral to the aorta then coursing down over the left iliac vessels. If it is not visible, the dissection plane may have been too posterior, resulting in the ureter inadvertently being swept anteriorly with the mesosigmoid. If so, the ureter must be identified, freed, then swept posteriorly (Figure 22-3).
Identification and ligation of the inferior mesenteric artery and vein:
♦ With the retroperitoneal plane established, the ureter and gonadal vessels preserved, and the dissection complete out to the white line of Toldt, the next step is to continue the plane cranially and medially to identify the inferior mesenteric artery (IMA).
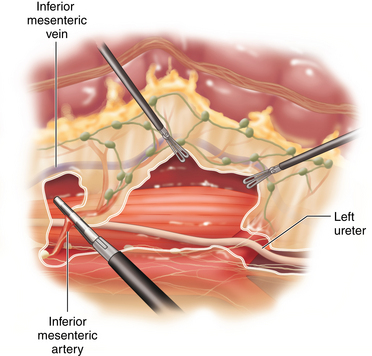
♦ The inferior mesenteric vein (IMV) runs posterolateral then cephalad to the IMA, continuing parallel to the aorta before passing behind the ligament of Treitz and the tail of the pancreas.
♦ An avascular window exists between the IMV and aorta between the IMA and the ligament of Treitz (Figure 22-4).
♦ For colorectal cancer, where a high vascular ligation is preferred, this window can be entered to isolate and divide the root of the IMA.
♦ For diverticular disease, vascular ligation may be performed distal to the left colic artery. Our preference for vascular control is to utilize a laparoscopic 5-mm vessel-sealing device (Figure 22-5).
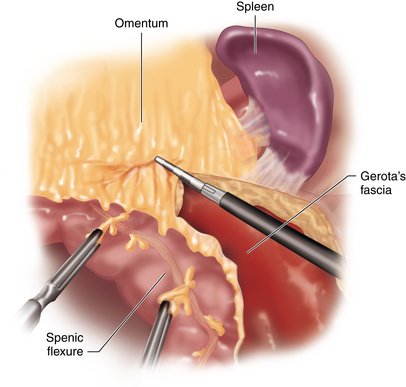
♦ The IMV is then isolated and divided in a similar fashion. The descending colon mesentery can now be elevated and dissected off of Gerota’s fascia out to the lateral attachments and up behind the splenic flexure. The cephalad extent of retroperitoneal dissection is to the inferior edge of the pancreas.
Division of the lateral attachments and splenic flexure:
♦ The sigmoid colon is retracted medially and the white line of Toldt divided starting at the sigmoid colon and progressing proximally.
♦ Splenic flexure mobilization can be facilitated by repositioning the patient in reverse Trendelenburg and by using a vessel-sealing device to maintain hemostasis. The plane of dissection is maintained between the colonic wall and the greater omentum. The proximal extent of the dissection should be into the lesser sac up to the level of the midtransverse colon (Figure 22-6).
♦ Omental attachments to the superior aspect of the splenic flexure mesentery are likewise released. This should provide an adequate length of colon for most pelvic anastomoses.
Division of the mesorectum and rectum:
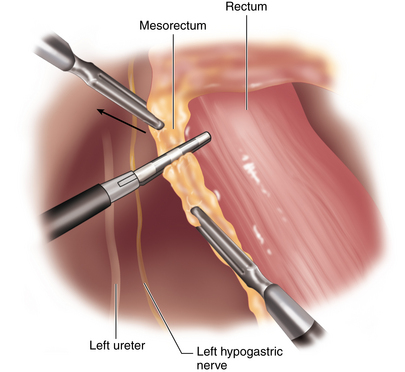
♦ The patient is repositioned back into steep Trendelenburg and attention directed back into the pelvis. Distal dissection is continued posterior to the rectum along the previously established planes between the fascia propria of the mesorectum and the presacral fascia (Figure 22-7).
♦ Left lateral peritoneal attachments of the rectosigmoid colon are released down to the distal resection margin.
♦ The mesorectum is divided using a vessel-sealing device (Figure 22-8).
♦ The rectum is divided using an endoscopic stapler.
♦ Alternatively, these last steps can be performed with open techniques via an extraction incision in the lower abdomen.
Specimen exteriorization, resection, and colorectal anastomosis:
♦ A 6- to 8-cm Pfannenstiel or lower midline extraction incision is created and a wound protector placed.
♦ The left colon is delivered. Its mesentery is divided just proximal to the IMA transection site. The bowel is divided. An end-to-end anastomosis (EEA) anvil is secured in the end of healthy descending colon. The fashioning of a transanal EEA anastomosis is monitored directly through the extraction site or alternatively the extraction site is closed, pneumoperitoneum reestablished, and the anastomosis monitored through laparoscopic techniques.
♦ An anastomotic air leak test is performed, followed by an inspection of the dissection planes for hemostasis.
♦ Trocars and extraction sites are closed using absorbable sutures.
Step 5. Pearls and pitfalls
♦ Recent research has called into question the need for routine cathartic bowel preparation for elective colon surgery. Our practice has likewise moved away from routine bowel preparation with some exceptions. These include when intraoperative colonoscopy for tumor localization, anastomosis with covering ostomy, and total mesorectal excision are planned, or when the patient has such a heavy fecal load that it will overwhelm the delicate laparoscopic instruments (i.e., total colectomy for chronic constipation).
♦ Laparoscopic surgery does not afford the surgeon the ability to use his or her hand to palpate and locate small polyps or tumors. Therefore, when operating for these indications, preoperative colonoscopy with three-quadrant submucosal injection of tattooing substance just distal to the lesion is the preferred technique. The availability of intraoperative colonoscopy is also ideal when the patient is bowel prepped and the lesion cannot be identified using laparoscopic techniques.
♦ The splenic flexure mobilization is usually approached in a retrograde fashion as described earlier. A compliment to this approach is to mobilize laterally just up to the flexure then move to the midtransverse colon. The omentum can be elevated cephalad and a plane between the omentum and transverse colon created up into the lesser sac. Once the lesser sac is opened, this plane is continued distally along the colon and mesocolon to complete the splenic flexure mobilization.