Chapter 2 Lateral, Posterior, and Cruciate Knee Anatomy
INTRODUCTION
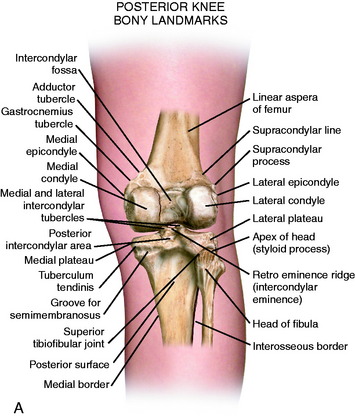
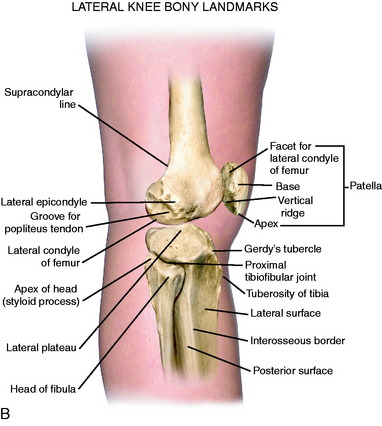
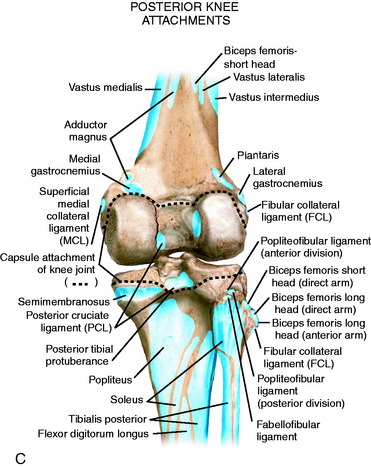
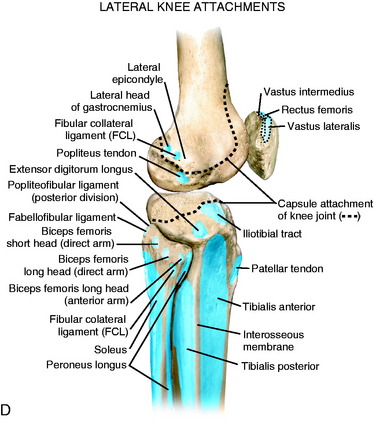
The posterior and lateral anatomy of the knee joint presents a challenge to even the most experienced knee surgeon. Knowledge of the bony topography will result in a greater number of anatomic ligament reconstructions (Fig. 2-1). A lack of familiarity leads to hesitancy when performing approaches in these areas of the knee. The inherent anatomic complexity of this region is further complicated by variations in terminology found in the orthopaedic literature. Work by LaPrade and coworkers23,24,26 and others have attempted to clarify the nomenclature used to describe these structures, allowing for better communication among surgeons. These advances also facilitate more accurate biomechanical studies.
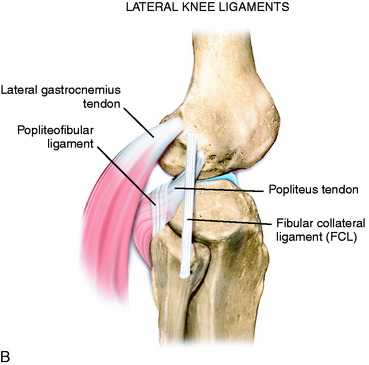
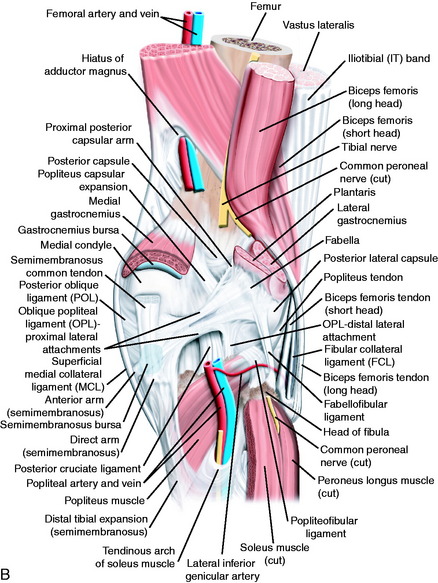
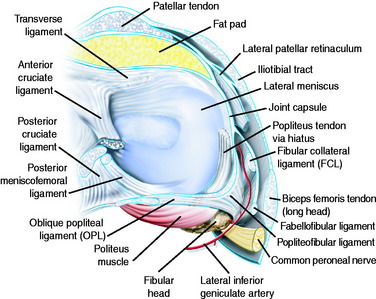
In posterolateral reconstructive procedures, the anatomic relationships of the fibular collateral ligament (FCL), popliteus muscle-tendon-ligament complex (PMTL), popliteofibular ligament (PFL), and the posterolateral capsule are particularly important. These structures function together to resist lateral joint opening, posterior subluxation of the lateral tibial plateau with tibial rotation, knee hyperextension, and varus recurvatum (see Chapter 20, Function of the Posterior Cruciate Ligament and Posterolateral Ligament Structures).11,45,47
ILIOTIBIAL BAND
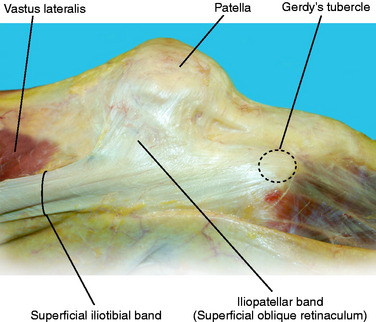
The iliotibial band (ITB) is a large fascial expansion that originates on the anterior superior iliac spine, covering the tensor fascia lata muscle proximally and extending along the lateral aspect of the thigh. Distally, the ITB has been divided into three separate layers: superficial, deep, and the capsulo-osseous layer.50,64 A portion of the superficial layer, called the iliopatellar band, extends anteriorly to the lateral aspect of the patella (Fig. 2-2).62 This band is important for proper patellofemoral tracking by resisting abnormal medial patella translation (medial glide).23 The majority of the superficial layer continues distally to insert on Gerdy’s tubercle. The deep layer connects the medial portion of the superficial layer to the lateral intermuscular septum of the distal femur. The most distal fibers of the deep layer continue to attach to the posterior aspect of the lateral femoral condyle (Fig. 2-3).64 The capsulo-osseous layer extends more medial and distal to the deep layer to merge with fibers from the short head of the biceps to form the biceps–capsulo-osseous iliotibial tract confluens.63 The capsulo-osseous layer continues distally, creating a sling posterior to the lateral femoral condyle to attach posterior and proximal to Gerdy’s tubercle.
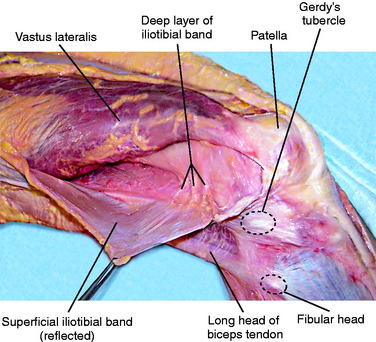
FIGURE 2-3 Deep fibers of the ITB are exposed as the superficial ITB is split and retracted posteriorly.
In knee extension, the ITB is anterior to the axis of rotation and helps maintain extension. When the knee is flexed to 90°, the ITB moves posterior to the axis of rotation. The anteroposterior (AP) position of the ITB with knee flexion contributes to the pivot shift phenomena with an anterior cruciate ligament (ACL) rupture.16 The posterior portion of the ITB tibiofemoral attachment is re-created in the lateral extra-articular ACL reconstruction.23,50 During flexion, the ITB moves posteriorly, exerting an external rotational and posteriorly directed force on the lateral tibia, contributing to the reduction in the pivot shift test. The ITB and lateral capsule are important structures that resist internal tibia rotation (see Chapter 3, The Scientific Basis for Examination and Classification of Knee Ligament Injuries). In extension, the ITB acts as a secondary restraint to varus stress.3 In severe lateral knee ligament injuries, the ITB may become abnormally lengthened, and at the time of surgery, distal advancement at Gerdy’s tubercle is indicated. A bursa between the ITB and the lateral femoral epicondylar region may become inflamed and produce pain. The lateral retinacular nerve courses just posterior to the bursa and may also become symptomatic.
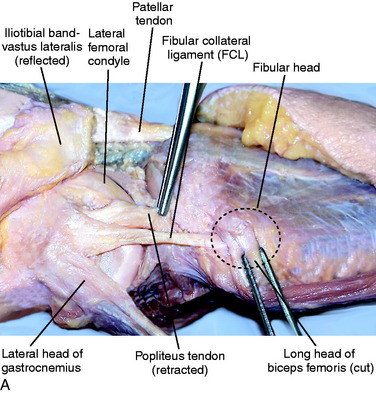
FCL
For this chapter, the term fibular collateral ligament has been selected instead of lateral collateral ligament because it represents the term most commonly used in anatomy textbooks23,55 and several studies.22,26,28,58,68,70 The FCL is a cordlike ligament that runs from the lateral femoral epicondyle to the fibular head (Fig. 2-4). When performing an anatomic FCL reconstruction, it is imperative that the surgeon understands the relationship of the FCL to its surrounding structures. On the femur, the FCL originates approximately 14 mm anterior26 and slightly distal to the attachment of the lateral gastrocnemius tendon. This tendon is a key landmark during FCL reconstruction because it is frequently spared during a posterolateral corner knee injury.64 In addition, the FCL attaches proximal and posterior to the popliteus femoral insertion. Distally, it attaches to the lateral aspect of the fibular head just medial to the anterior arm of the long head of the biceps tendon.
In 2003, LaPrade and associates26 published a quantitative anatomic study that described the FCL and its relationship to osseous landmarks and other posterolateral structures of the knee. These authors reported that the FCL does not originate directly off of the lateral epicondyle, but attaches approximately 1.4 mm proximal and 3.1 mm posterior to the epicondyle, residing in a small bony depression. The average distance between the FCL and the popliteus attachments on the femur was 18.5 mm. The ligament travels distally to insert 8.2 mm posterior to the anterior margin of the fibular head and 28.4 mm distal to the tip of the fibular styloid process (Fig. 2-5).26 The distal 25% of the FCL is surrounded by the FCL–biceps femoris bursa, which has been implicated as a possible source of lateral knee pain.10 The bursa is covered by the anterior arm of the long head of the biceps.24
The FCL is the primary restraint to varus loads at all degrees of flexion.11 In a cadaveric sectioning study, Grood and colleagues11 reported that the limit for varus angulation was normal as long as the FCL was intact. In addition, for large changes in external rotation to occur, the popliteus tendon, PFL, posterolateral capsule, and the FCL must all be injured.67 Thus, the FCL provides significant resistance to external rotation. The FCL is a secondary restraint to internal rotation at higher flexion angles (see Chapter 3, The Scientific Basis for Examination and Classification of Knee Ligament Injuries).
FABELLOFIBULAR LIGAMENT
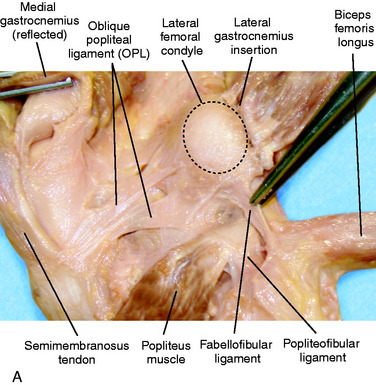
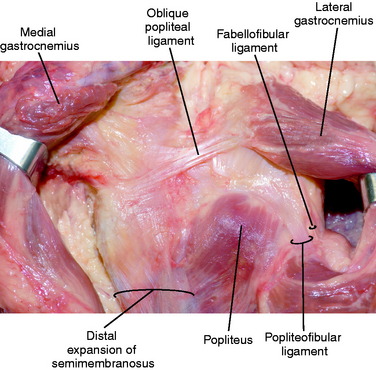
The fabellofibular ligament begins at the lateral aspect of the fabella (or posterior aspect of the supracondylar process of the lateral femur if a fabella is absent) and inserts distally on the posterolateral edge of the fibular styloid (Fig. 2-6).4 It attaches posterior and lateral to the insertion of the PFL. Proximally, the fabellofibular ligament is a continuation of the capsular arm of the short head of the biceps tendon.63,64 The fabellofibular ligament is termed the short lateral ligament in the absence of a fabella.21 Throughout this text, this structure is referred to as the fabellofibular ligament. The size of the fabellofibular ligament has been directly correlated to the presence of a bony fabella.23,36,51 When a bony fabella is present, the ligament is more robust, with the opposite being true when the fabella is cartilaginous or absent.
The fabellofibular ligament has been identified in several studies in a variable percentage of patients.4,26,51,59,65 Sudasna and Harnsiriwattanagit60 reported that the fabellofibular ligament was present in 68% percent of individuals. Minowa and coworkers36 identified a fabellofibular ligament in 51.4% of cadaver knees. Diamantopoulos and associates4 found the fabellofibular ligament in 40% of knees dissected using microsurgical techniques. In contrast, LaPrade23 believes that the fabellofibular ligament is present in all knees owing to the fact that, by definition, it is the distal extension of the capsular arm of the short head of the biceps. This was confirmed by a recent article27 describing these authors’ anatomic findings. Functionally, the fabellofibular ligament is taut in extension.65 Thus, it can be inferred that it provides resistance to knee hyperextension. However, to date, no biomechanical studies have been published that describe the function of the fabellofibular ligament.
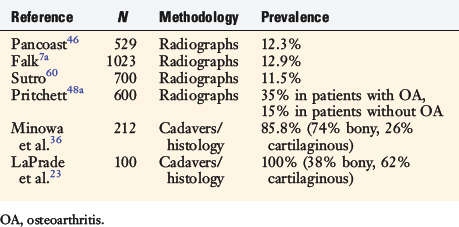
FABELLA
The fabella, or “little bean,” is a bony or cartilaginous structure nestled in the posterolateral aspect of the knee. It is generally believed to reside in the tendon of the lateral head of the gastrocnemius; however, many structures merge at the fabella (Table 2-1). The fabella ranges in size from approximately 5 mm to over 20 mm in diameter, with the majority (70%) being oval in shape.36,46 There are varying reports on the incidence of the fabella. Earlier radiographic studies appear to underestimate the true prevalence of the fabella compared with more recent cadaveric and histologic studies (Table 2-2). This structure is present bilaterally in approximately 80% of cases. The fabella has been implicated as a cause of posterior knee pain in multiple conditions including chondromalacia fabella, “fabella syndrome,” fracture of the fabella, impingement after total knee arthroplasty, and peroneal nerve irritation.8,10,29,32,33,49,66 Thus, the fabella and surrounding structures represent a rare but potential source of posterolateral knee pain.
| Capsular arm of the short head of the biceps femoris |
| Fabellofibular ligament |
| Lateral gastrocnemius tendon |
| Proximal lateral attachment of the oblique popliteal ligament |
| Posterolateral capsule |
PMTL COMPLEX
The PMTL is an intricate anatomic conglomerate made up of the popliteus muscle, the PFL, the femoral insertion of the popliteus tendon, the popliteomeniscal fascicles and soft tissue attachments to the lateral meniscus, and the proximal tibia. The crucial components for posterolateral stability include the popliteus tendon and the PFL. These structures act in concert with the FCL and posterolateral capsule to prevent excessive external rotation and varus rotation of the knee.11,45 Restoration of only a portion of these structures may result in residual instability.42 This is discussed in detail in Chapter 22, Posterolateral Ligament Injuries: Diagnosis, Operative Techniques, and Clinical Outcomes, including the anatomic reconstruction of the FCL, popliteus tendon, and PFL.38–41
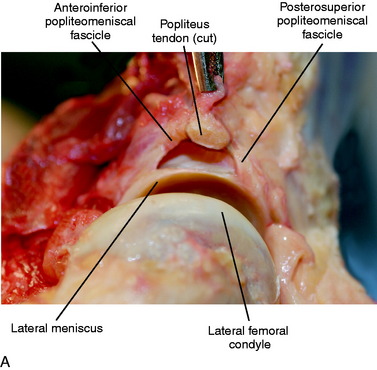
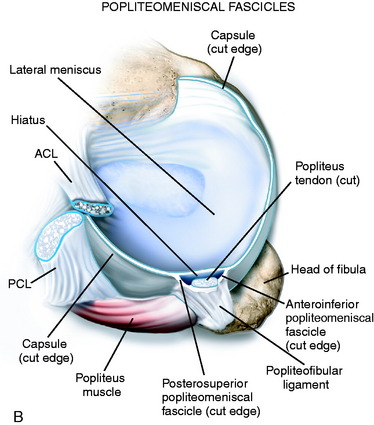
The popliteus muscle originates on the posterior tibia just proximal to the soleal line and proceeds lateral and proximal to insert on the lateral femoral condyle (see Fig. 2-6B). The popliteus tendon proceeds proximally through a hiatus in the coronary ligament of the lateral meniscus, then deep to the FCL to ultimately insert anterior and distal to the insertion of the FCL (see Fig. 2-4). As referenced earlier, LaPrade and associates26 reported that the popliteus inserted an average of 18.5 mm from the FCL on the femur. Staubli and Birrer56 further described the anatomy of the popliteus tendon at the level of the knee joint. Three attachments of the popliteus tendon to the lateral menisci (termed the popliteomeniscal fascicles) were noted that include the anteroinferior, posterosuperior, and posteroinferior fascicles (Fig. 2-7). These fascicles provide stability to the lateral meniscus and, when torn, lead to abnormal translation of the lateral meniscus.25,54 This may lead to mechanical symptoms and lateral knee pain. In Chapter 28, Meniscus Tears: Diagnosis, Repair Techniques, and Clinical Outcomes, the repair techniques for the lateral meniscus and popliteomeniscal fascicles are described.
LaPrade and colleagues27 described a thickening of the posterior joint capsule that extends from the medial aspect of the popliteus musculotendinous junction to the posteromedial aspect of the intercondylar notch of the femur, termed the proximal popliteus capsular expansion (see Fig. 2-6B). The study reported this structure to be present in all dissections, and the authors of this chapter have also found it to be a constant structure. This structure may provide an additional restraint to knee external tibial rotation and hyperextension.
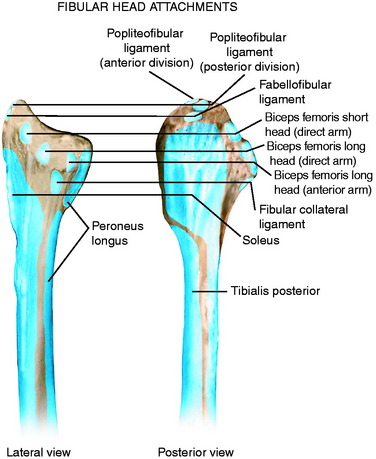
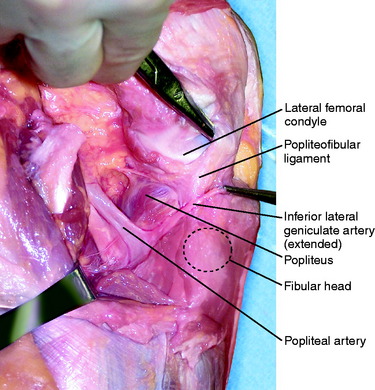
The PFL originates at the musculotendinous junction of the popliteus and attaches to the medial aspect of the fibular head (Fig. 2-8), where it lies deep to the fabellofibular ligament. Of clinical significance, the inferior lateral geniculate artery courses between these two structures. The artery is frequently encountered during exposure of the posterolateral corner of the knee, especially during the approach for an inside-out lateral meniscus repair (Fig. 2-9). The artery is protected, if possible, and, if injured, requires cauterization to prevent postoperative hematoma formation. The PFL consists of two divisions, an anterior and a posterior division.26 LaPrade and associates26 found that the average width of the anterior division’s attachment at the fibular styloid was 2.6 mm, and the posterior division’s width at the fibular styloid attachment was 5.8 mm. Thus, the posterior division may contribute more significantly than the anterior division to stability of the posterolateral aspect of the knee.
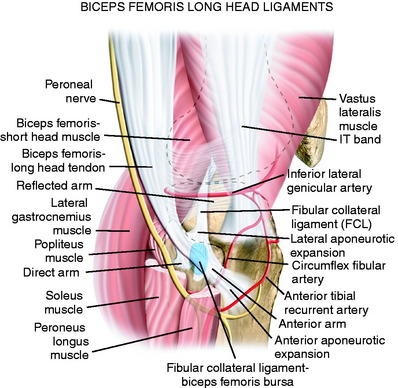
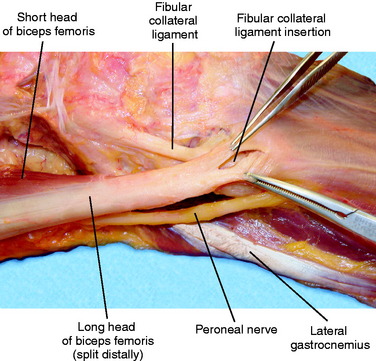
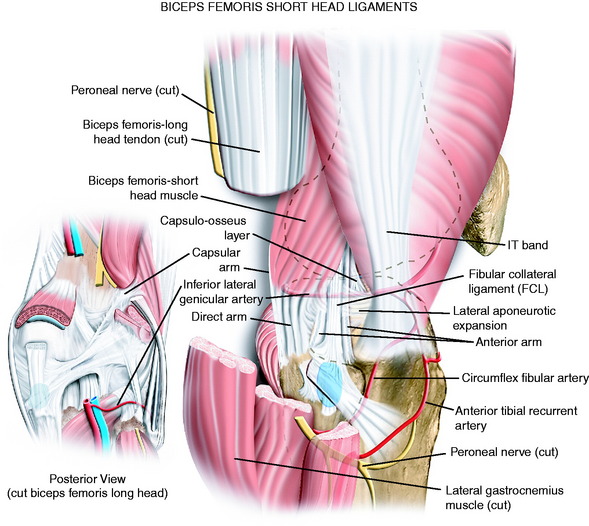
BICEPS FEMORIS
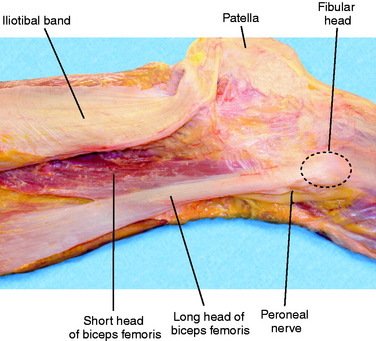
The biceps femoris is a fusiform muscle comprising two heads: long and short. The long head originates from the ischial tuberosity and is innervated by the tibial division of the sciatic nerve. The short head originates from the lateral aspect of the linea aspera of the femur and is innervated by the peroneal division of the sciatic nerve.50 Distally, the two heads of the biceps lie just posterior to the ITB (Fig. 2-10). Both heads of the biceps have complex attachments to the posterolateral aspect of the knee. These distinct attachments are described and shown in Tables 2-3 and 2-4. In the authors’ experience (in cadaveric dissections and at surgery), many of the attachments blend together distally and are difficult to identify as separate structures. The peroneal nerve lies just distal and posterior to the biceps, curving around the fibular neck. The biceps flexes the knee and also externally rotates the leg when the knee is flexed.51
TABLE 2-3 Five Components of the Long Head of the Biceps Femoris
| Component | Attachment |
|---|---|
| Reflected arm | Posterior edge of ITB |
| Direct arm | Posterolateral edge of the fibula |
| Anterior arm | Lateral fibular head, FCL, anterior aponeurotic expansion |
| Lateral aponeurotic expansion | FCL |
| Anterior aponeurotic expansion | Anterior compartment of the leg |
FCL, fibular collateral ligament; ITB, iliotibial band.
TABLE 2-4 Six Components of the Short Head of the Biceps Femoris
| Component | Attachment |
|---|---|
| Proximal muscular attachment | Anteromedial aspect of the long head |
| Capsular arm | Posterolateral knee capsule |
| Capsulo-osseus layer | Proximolateral tibia |
| Direct arm | Fibular head |
| Anterior arm | Proximolateral tibia |
| Lateral aponeurotic expansion | FCL |
FCL, fibular collateral ligament.
There are varying descriptions of the anatomy of the biceps and the number of attachments.19,20,34,51,63 Terry and LaPrade63 described five attachments of the long head of the biceps, including two tendinous and three fascial components (Fig. 2-11; see also Table 2-3). The two tendinous components (direct and anterior arms) and one of the fascial components (lateral aponeurotic expansion) make up the key portion of the long head anatomy. The other fascial components are the reflected arm and the anterior aponeurotic expansion.
The most proximal component is the reflected arm. It originates just proximal to the fibular head and ascends anteriorly to insert on the posterior edge of the ITB. The direct arm inserts onto the posterolateral edge of the fibula just distal to the tip of the styloid (see Fig. 2-5).23 The anterior arm has a more complex attachment and some important anatomic points. A portion of the anterior arm inserts onto the lateral aspect of the fibular head, and the rest continues distally just lateral to the FCL. Just proximal and at this fibular insertion, portions of the anterior arm ascend anteriorly to form the lateral aponeurotic expansion that attaches to the posterior and lateral aspect of the FCL. Here, a small bursa separates the anterior arm from the distal fourth of the FCL. The anterior arm thus forms the lateral wall of this bursa.63 This is an important surgical landmark because a small horizontal incision can be made here, 1 cm proximal to the fibular head, to enter this bursa and locate the insertion of the FCL into the fibular head (Fig. 2-12).23 The anterior arm then continues distally over the FCL, forming the anterior aponeurosis, which covers the anterior compartment of the leg.
The short head of the biceps courses just deep (or medial) and anterior to the long head tendon, sending a majority of its proximal muscular fibers to the long head tendon itself.63 It has six distal attachments (Fig. 2-13; see also Table 2-4). The most important attachments are that of the direct arm, the anterior arm, and the capsular arm.
The capsular arm originates just prior to the short head reaching the fibula. It then continues deep to the FCL to insert onto the posterolateral knee capsule and fabella. Here, the fibers of the capsular arm continue distally as the fabellofibular ligament.63 Just distal to the capsular arm, a capsulo-osseous layer forms a fascial confluence with the ITB (the biceps–capsulo-osseous–iliotibial tract confluens). The direct arm of the short head inserts onto the fibular head just posterior and proximal to the direct arm of the long head tendon. The anterior arm then continues medial or deep to the FCL, partially blends with the anterior tibiofibular ligament, and inserts onto the tibia 1 cm posterior to Gerdy’s tubercle. This site is also the attachment of the mid-third lateral knee capsule.63 It is important clinically because an avulsion fracture can be seen here in ACL injuries, known as a Segond fracture.52,63 Finally, the lateral aponeurotic expansion of the short head inserts onto the medial aspect of the FCL (versus this expansion of the long head that inserts onto the posterior aspect of the FCL).63
THE FIBULAR HEAD
The fibular head is a key anatomic and structural component to the posterolateral knee. It is easily palpable in most patients and is thus an excellent anatomic reference point. In the literature, incomplete descriptions of the anatomy and insertion of structures of the proximal fibula exist. Six key structures attach to the fibular head: three tendons and three ligaments (Table 2-5; see also Fig. 2-5). The PFL attaches to the tip of the fibular styloid. Just distal and lateral, the fabellofibular ligament attaches on the slope of the styloid. The FCL, as mentioned previously, attaches proximally 28 mm distal to the styloid and 8 mm from the anterior cortex of the fibula, depending of course on specimen size variations.26 A portion of the anterior arm of the long head of the biceps attaches to the lateral aspect of the fibular head. The direct arms of the long and short heads of the biceps attach to the posterior aspect of the fibular head, the long head being just lateral to that of the short head.
| Structure | Location on Fibular Head |
|---|---|
| LH biceps, direct arm | Posterolateral edge (lateral and distal to the styloid) |
| LH biceps, anterior arm | Posterolateral edge (slightly distal and lateral to the direct arm of the LH) |
| SH biceps, direct arm | Posterior edge (lateral to the styloid, medial to the direct arm of the LH) |
| Popliteofibular ligament | Medial aspect of the styloid |
| Fibular collateral ligament | Anterolateral edge (28 mm distal to the styloid, 8 mm posterior to the anterior edge of the fibula) |
| Fabellofibular ligament | Lateral to the tip of the styloid |
LH, long head; SH, short head.
THE KNEE CAPSULE
The knee capsule envelopes the joint, extending from the articular margin of the femur to the tibia (see Fig. 2-1C and D). On the tibia, it inserts 4 to 14 mm below the articular surface. The most distal attachment at the tibia is located at the posteromedial and posterolateral aspect.2 Some authors50 have identified a thickening of the capsule laterally, naming this the mid-third lateral capsular ligament. This ligament is divided into two components. The meniscofemoral component and meniscotibial component extend from the femur and tibia, respectively, to attach to the lateral meniscus.50 The lateral retinacular nerve, a branch of the sciatic nerve, courses along the surface of the lateral capsule (Fig. 2-14).
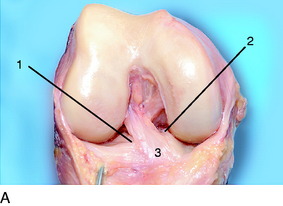
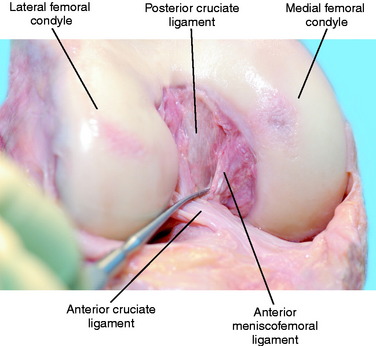
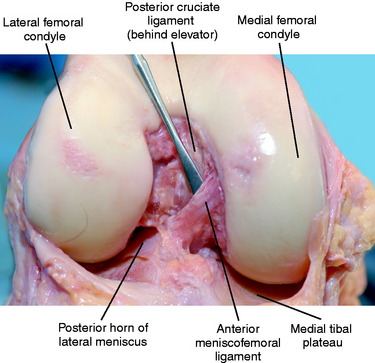
ACL
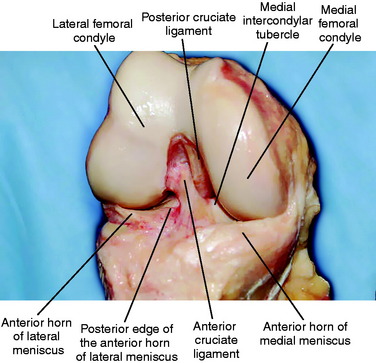
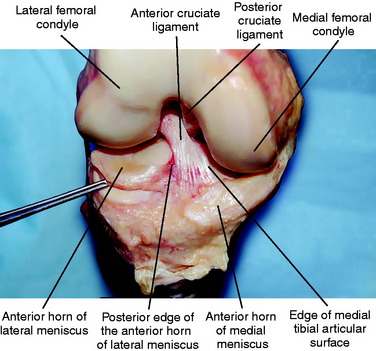
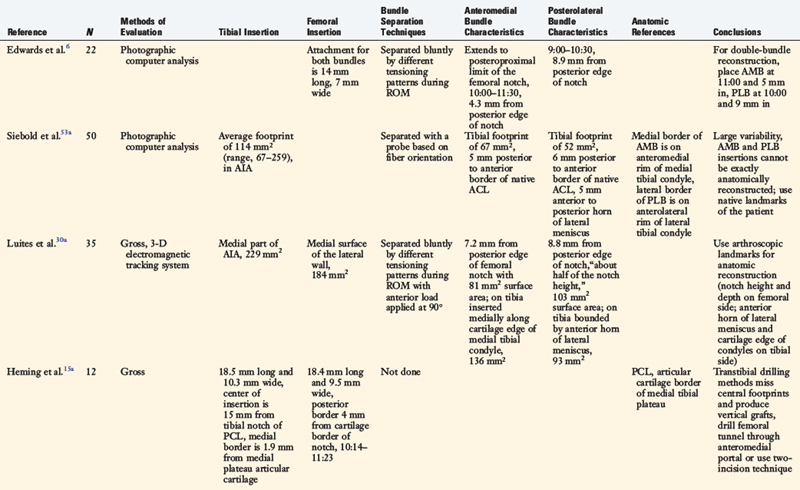
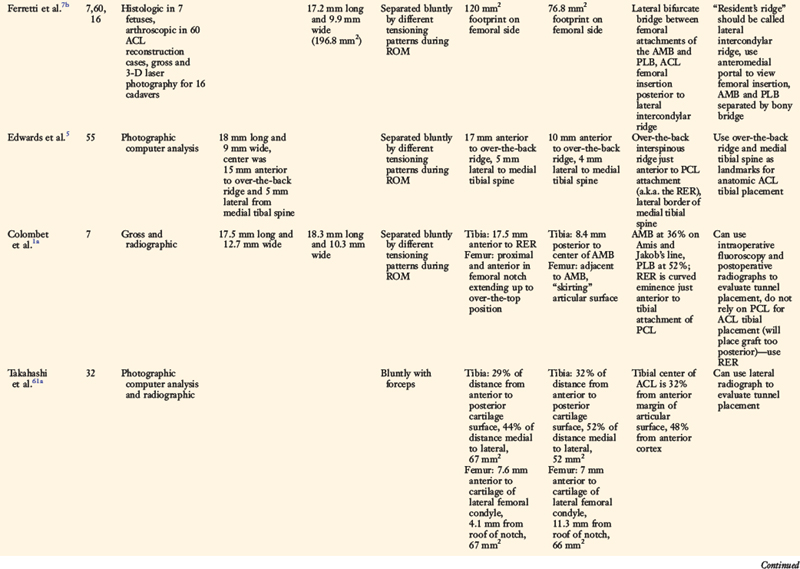
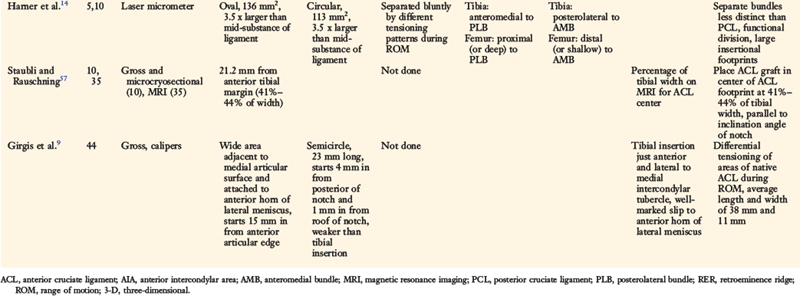
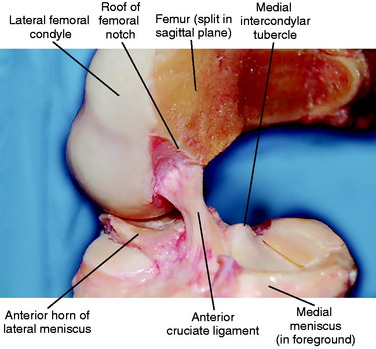
The ACL (Figs. 2-15 and 2-16) is the primary restraint to anterior translation of the tibia at all degrees of flexion.44 It also limits coupled internal rotation and anterior translation of the tibia, measured by the pivot shift and/or flexion-rotation drawer tests.43,44 Various descriptions, nomenclature, and anatomic reference points of the ACL are present in the literature. Early descriptions date back to the 1800s.69 Since then, numerous studies describing ACL anatomy have been published (Table 2-6). The average length of the ACL is 38 mm, and the average width is 11 mm. The ACL has a larger attachment site than its central dimensions. Although some authors describe a separate anteromedial and posterolateral bundle, the authors of this chapter do not believe an anatomic separation exists. Some authors such as Edwards and coworkers5,6 (see Table 2-6) divide the ACL into two functional bundles. However, as discussed in Chapter 7, Anterior Cruciate Ligament Primary and Revision Reconstruction: Diagnosis, Operative Techniques, and Clinical Outcomes, this represents an oversimplification of fiber function. The ACL, like the posterior cruciate ligament (PCL), is a continuum of fibers of different lengths and attachment characteristics.
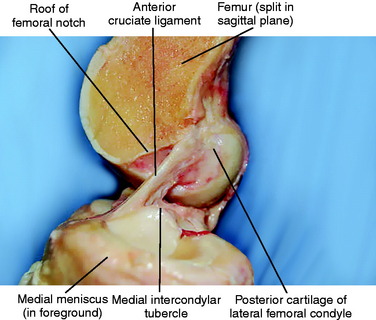
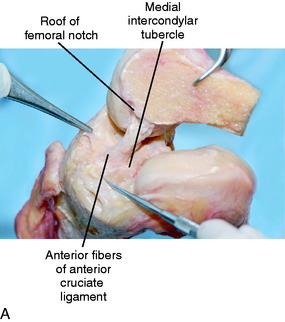
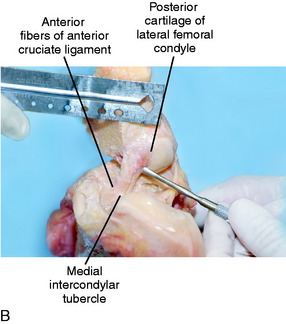
The ACL originates on the medial aspect of the lateral femoral condyle (Figs. 2-17 and 2-18). The origin has been described as an oval or a semicircle, approximately 18 mm long and 10 mm wide, lying just behind a bony ridge known as resident’s ridge.17 It is anterior to the posterior cartilage of the lateral femoral condyle (Fig. 2-19A). Multiple referencing systems have been used to describe the ACL femoral attachment including clock systems, quadrant or grid systems, and measurements based on the posterior articular cartilage (see Chapter 7, Anterior Cruciate Ligament Primary and Revision Reconstruction: Diagnosis, Operative Techniques, and Clinical Outcomes).
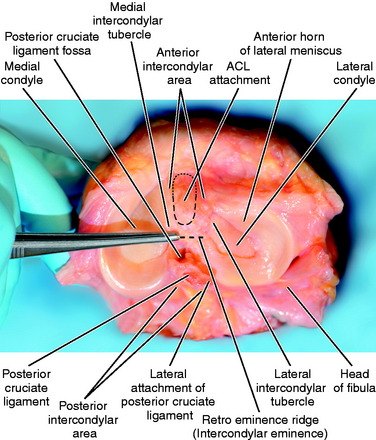
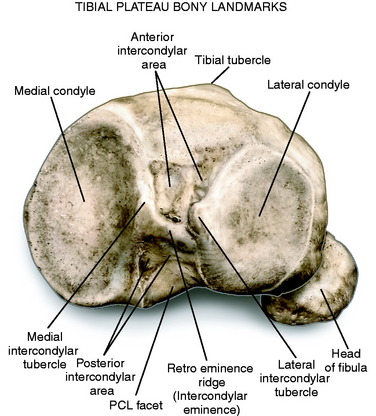
The ACL inserts onto the tibia in the anterior intercondylar area (AIA) in a roughly oval to triangular pattern. The insertion fans out, especially anteriorly, at the tibial insertion and has been described as a “duck’s foot” (see Fig. 2-19B).48 The AP dimension of the insertion is approximately 18 mm, and the mediolateral dimension is 10 mm. The anterior border of the ACL is approximately 22 mm from the anterior cortex of the tibia and 15 mm from the anterior edge of the articular surface. Its center is approximately 15 to 18 mm anterior to the retroeminence ridge (RER) (Fig. 2-20). Edwards and coworkers5 described the RER (a.k.a. the over-the-back interspinous ridge) as a transverse ridge on the apex of the posterior slope of the tibial plateau, just anterior to the PCL. Different terms are used for the bony topography of the proximal tibia (Fig. 2-21). The term retroeminence ridge is referred to as the intercondylar eminence in gross anatomy texts.1,55 The medial and lateral tibial spines are referred to as the medial and lateral intercondylar tubercles.1 The ACL insertion is just lateral to the tip of the medial intercondylar tubercle, and therefore, it inserts not on the tip of the medial intercondylar tubercle, but on the lateral slope. The anterior horn of the lateral meniscus is a useful landmark during an arthroscopic ACL reconstruction. Over 50% of the ACL inserts anterior to the posterior edge of the anterior horn of the lateral meniscus (Fig. 2-22). Using radiography and magnetic resonance imaging (MRI), Staubli and Rauschning57 showed that the center of the insertion is 44% of the width from anterior to posterior of the proximal tibia. For ACL reconstruction, we recommend placing the graft at the tibial and femoral attachment sites, as discussed in Chapter 7, Anterior Cruciate Ligament Primary and Revision Reconstruction: Diagnosis, Operative Techniques, and Clinical Outcomes.
PCL
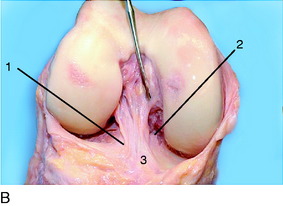
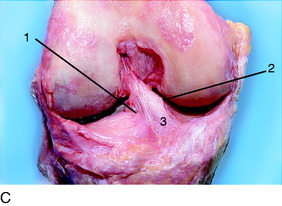
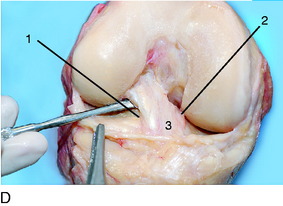
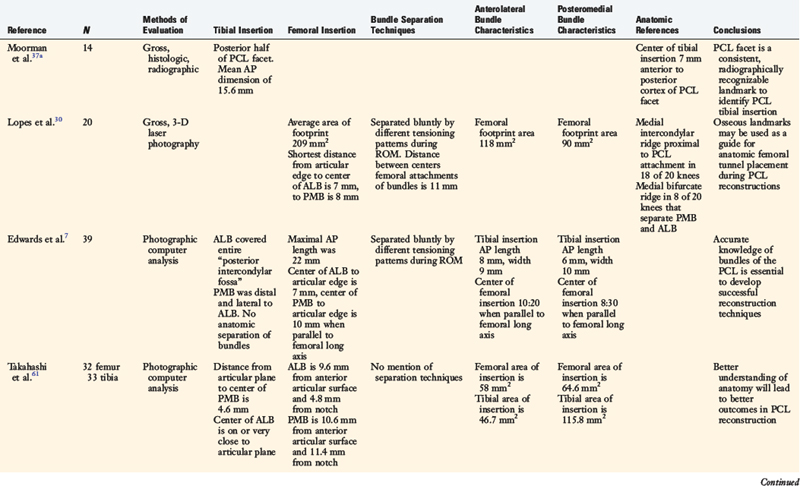
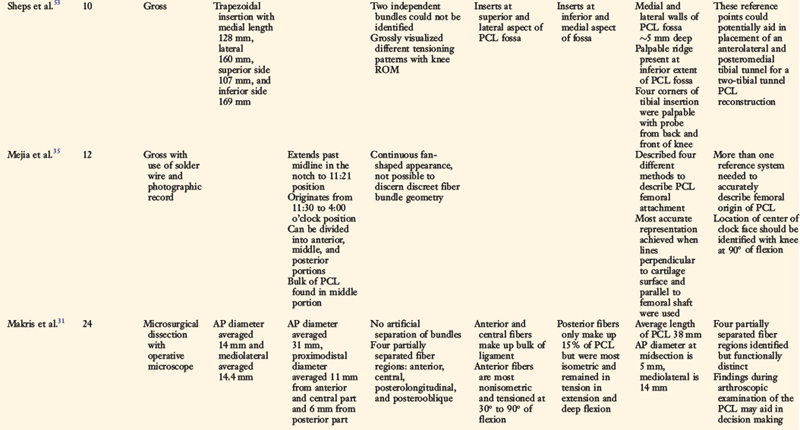
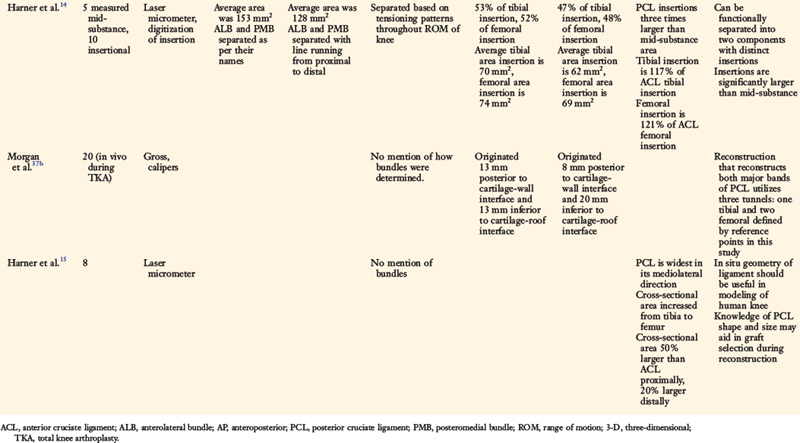
The PCL is the primary restraint to posterior translation of the tibia at all degrees of flexion. Numerous studies describing PCL anatomy have been published (Table 2-7). Various descriptions, nomenclature, and anatomic reference points are present in the literature. One of the first anatomic studies was conducted in 1975 by Girgis and associates.9 Earlier studies focused on femoral and tibial attachment sites as well as cross-sectional area and length of the PCL. The PCL is a large ligament with fan-shaped insertion sites. The average length of the PCL is 38 mm, and the average width is 13 mm.9 The insertion sites are three times the cross-sectional area than its mid-substance area.14 The PCL’s insertion sites are larger than the corresponding insertion sites of the ACL.15
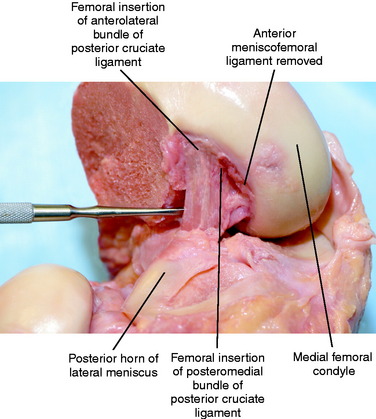
With the advent of the two-bundle description of PCL anatomy, more recent studies have attempted to arbitrarily separate two functional bundles based on differing tensioning patterns throughout the range of motion of the knee.7,14,30,61 However, some studies have been unable to identify discreet geometric bundles.31,35,53 These descriptions have focused on separate anterolateral (AL) and posteromedial (PM) bundles in hopes to more accurately reconstruct the PCL; however, the authors of this chapter believe that the two-bundle representation of the PCL oversimplifies PCL fiber function. The PCL is a continuum of fibers of different lengths and attachment characteristics that are more accurately described in Chapter 20, Function of the Posterior Cruciate and Posterolateral Ligament Structures. Inconsistency in the size and description of the two bundles exists in the literature owing to the fact that these are not distinct anatomic structures. The bundle nomenclature is used to reference other publications that have used this terminology.
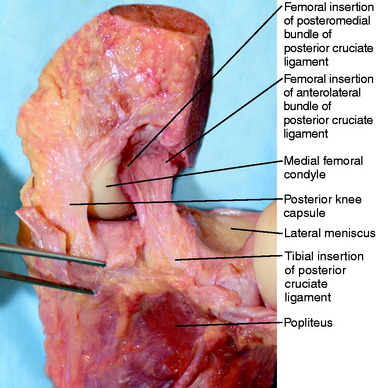
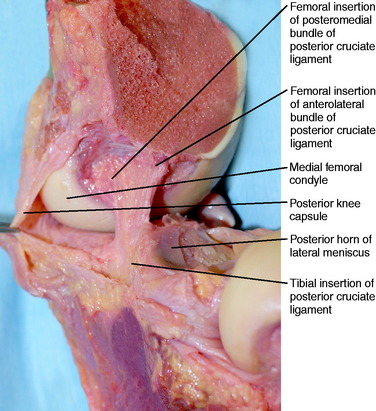
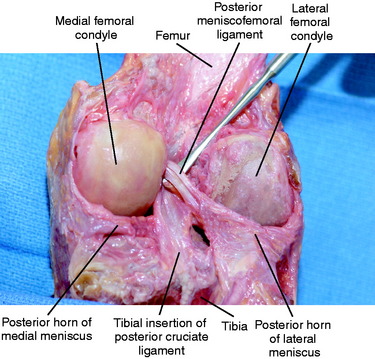
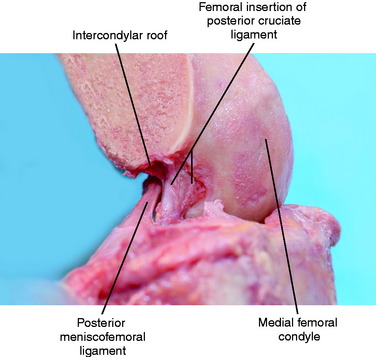
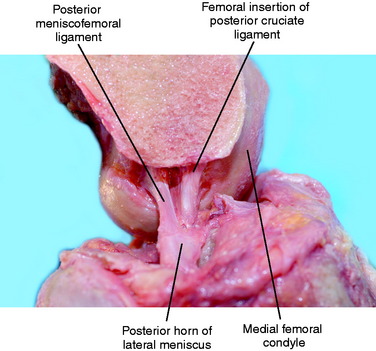
The PCL inserts on the tibia up to 1 cm distal to the posterior articular cartilage surface in the midportion of the tibia in the coronal plane (Figs. 2-23 and 2-24). Its insertion is rectangular or trapezoidal. One published study37 described the PCL attaching to the “PCL facet” of the posterior proximal tibia. This insertion area has also been termed the posterior intercondylar fossa or the PCL fossa.7 The AP dimension of the tibial insertion is approximately 15 mm (14–16 mm) in length. The mediolateral dimension is approximately 10 to 16 mm in width. The inferior base is wider, contributing to its trapezoidal shape. The center of the PCL tibial attachment lies 7 mm anterior to the posterior cortex of the PCL fossa. Sheps and colleagues53 described palpable landmarks of the four corners of the PCL fossa as well as a ridge present at the inferior extent of the tibial insertion. Harner and coworkers14 believe that the AL and PM bundles contribute equally to the tibial insertion area of the PCL. However, Takahashi and associates61 found the majority of the tibial insertion to be made up of the PM bundle (115.8 mm2 vs. 46.7 mm2). The medial meniscal root lies anterior and along the medial aspect of the PCL fossa and must be protected during PCL reconstruction.18 The capsule attachment at the distal aspect of the PCL fossa (see Fig. 2-1C) is an important anatomic landmark because PCL graft reconstructions are placed at the most distal aspect of the fossa. Through dissections, the authors of this chapter have noted a coalescence of fibers with the posterior horn of the lateral meniscus that is distinct from the meniscofemoral ligaments (MFLs).
The femoral insertion of the PCL is highly variable. It attaches to the medial intercondylar wall in a half-moon– or bullet-shaped fashion (Figs. 2-25 to 2-27). Multiple reference points have been used to describe this insertion, including clock positions perpendicular to the cartilage surface, clock measurements parallel to the femoral shaft, clock measurements parallel to the intercondylar roof, and radial measurements from the intercondylar roof.7,35 More than one measurement should be used to describe the PCL femoral insertion accurately.35 Edwards and colleagues7 used a grid measurement scale to describe the femoral attachment. The area of femoral insertion varies widely from approximately 125 mm2 to over 200 mm2.14,30 The AL bundle attaches “higher” onto the wall with a portion of its fibers crossing the midline. Edwards and colleagues7 found the AL bundle’s femoral insertion centered at the 10:20 position when referenced parallel to the femoral shaft. The PM center corresponded to the 8:30 position. The AL bundle is generally closer to the articular cartilage of the medial femoral condyle, with its center 7 mm from the edge, and the center of the PM bundle is approximately 8 to 11 mm from the edge of the cartilage. Harner and coworkers14 found equal distributions of the AL and PM bundles to the femoral insertion area. However, Lopes and coworkers30 found the AL bundle contributes 118 mm2 compared with the PM bundle’s contribution of 90 mm2. These investigators also described a medial bifurcate ridge (present in 8 of 20 cadavers) that separates the AL and PM bundles’ femoral insertions. The variation between studies reflects the lack of a true anatomic separation of the PCL into bundles, which does not accurately describe PCL fiber function (see Chapter 20, Function of the Posterior Cruciate and Posterolateral Ligament Structures).
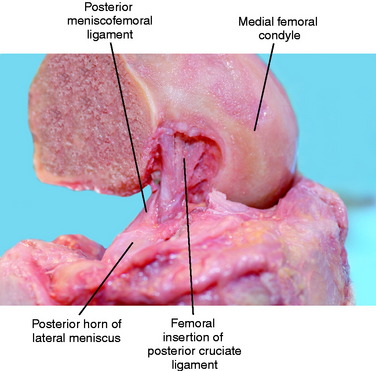
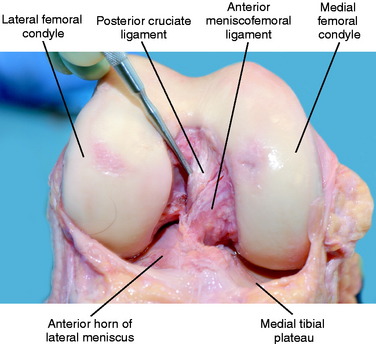
Besides the contribution of the PCL to knee stability, the MFLs contribute as secondary restraints to resist posterior tibial translation. Two MFLs may exist: the anterior meniscofemoral ligament of Humphrey (aMFL) and/or the posterior meniscofemoral ligament of Wrisberg (pMFL) (Figs. 2-28 to 2-32). The aMFL originates from the posterior horn of the lateral meniscus and travels anterior to the PCL, attaching close to the articular cartilage of the medial femoral condyle. The pMFL travels posterior to the PCL and attaches near the intercondylar roof. Gupte and associates12 described three main anatomic clues to distinguish the MFLs from the PCL. These include the insertional anatomy of the femur, the increased obliquity of the fibers of the MFLs compared with the PCL fibers, and a cleavage plane between the MFLs and the PCL. Gupte and colleagues13 found the aMFL to be present in 74% of cadaveric knees and the pMFL in 69% of knees. Ninety-three percent of specimens were found to have at least one MFL. In a separate report, Gupte and associates12 described an arthroscopic “meniscal tug test” to distinguish the MFLs from the PCL, thus avoiding the misdiagnosis of partial versus complete PCL rupture.
CONCLUSION
The posterior and lateral aspects of the knee are difficult anatomic areas for the orthopaedic surgeon owing, in part, to the varied nomenclature in the literature. This chapter has attempted to clarify these terms based on the most recent references. Illustrations have been used as needed to point out the key structures. An axial view of the proximal tibia summarizes the nomenclature and anatomy (see Fig. 2-14).
1 Clemente C.D., editor. Anatomy: A Regional Atlas of the Human Body. Baltimore: Lippincott, Williams & Wilkins, 2007.
1a Colombet P., Robinson J., Christel P., et al. Morphology of anterior cruciate ligament attachments for anatomic reconstruction: a cadaveric dissection and radiographic study. Arthroscopy. 2006;22:984-992.
2 DeCoster T.A., Crawford M.K., Kraut M.A. Safe extracapsular placement of proximal tibia transfixation pins. J Orthop Trauma. 2004;18(8 suppl):S43-S47.
3 DeLee J.C., Drez D., Noyes F.R., et al. The role of high tibial osteotomy in the anterior cruciate-deficient knee with varus alignment. In: DeLee J.C., Drez D., Miller M.D., editors. Orthopaedic Sports Medicine: Principles and Practice. Philadelphia: W. B. Saunders; 2003:1900.
4 Diamantopoulos A., Tokis A., Tzurbakis M., et al. The posterolateral corner of the knee: evaluation under microsurgical dissection. Arthroscopy. 2005;21:826-833.
5 Edwards A., Bull A.M., Amis A.A. The attachments of the anteromedial and posterolateral fibre bundles of the anterior cruciate ligament: part 1: tibial attachment. Knee Surg Sports Traumatol Arthrosc. 2007;15:1414-1421.
6 Edwards A., Bull A.M., Amis A.A. The attachments of the anteromedial and posterolateral fibre bundles of the anterior cruciate ligament: part 2: femoral attachment. Knee Surg Sports Traumatol Arthrosc. 2008;16:29-36.
7 Edwards A., Bull A.M., Amis A.A. The attachments of the fiber bundles of the posterior cruciate ligament: an anatomic study. Arthroscopy. 2007;23:284-290.
7a Falk G.D. Radiographic observations on the incidence of fabella. Bull Hosp Joint Dis. 1963;24:127-129.
7b Ferretti M., Ekdahl M., Shen W., Fu F.H. Osseous landmarks of the femoral attachment of the anterior cruciate ligament: an anatomic study. Arthroscopy. 2007;23:1218-1225.
8 Frey C., Bjorkengen A., Sartoris D., Resnick D. Knee dysfunction secondary to dislocation of the fabella. Clin Orthop Relat Res. 1987;222:223-227.
9 Girgis F.G., Marshall J.L., Monajem A.L. The cruciate ligaments of the knee joint. Anatomical, functional and experimental analysis. Clin Orthop. 1975;106:216-231.
10 Goldenberg R.R., Wild E.L. Chondromalacia fabellae. J Bone Joint Surg Am. 1952;24:688-690.
11 Grood E.S., Stowers S.F., Noyes F.R. Limits of movement in the human knee. Effect of sectioning the posterior cruciate ligament and posterolateral structures. J Bone Joint Surg Am. 1988;70:88-97.
12 Gupte C.M., Bull A.M., Atkinson H.D., et al. Arthroscopic appearances of the meniscofemoral ligaments: introducing the “meniscal tug test. Knee Surg Sports Traumatol Arthrosc. 2006;14:1259-1265.
13 Gupte C.M., Smith A., McDermott I.D., et al. Meniscofemoral ligaments revisited. Anatomical study, age correlation and clinical implications. J Bone Joint Surg Br. 2002;84:846-851.
14 Harner C.D., Baek G.H., Vogrin T.M., et al. Quantitative analysis of human cruciate ligament insertions. Arthroscopy. 1999;15:741-749.
15 Harner C.D., Livesay G.A., Kashiwaguchi S., et al. Comparative study of the size and shape of human anterior and posterior cruciate ligaments. J Orthop Res. 1995;13:429-434.
15a Heming J.F., Rand J., Steiner M.E. Anatomical limitations of transtibial drilling in anterior cruciate ligament reconstruction. Am J Sports Med. 2007;35:1708-1715.
16 Hoppenfeld S. The knee. In: Hoppenfeld S., deBoer P., editors. Surgical Exposures in Orthopedics: The Anatomic Approach. Philadelphia: J. B. Lippincott; 1994:455-478.
17 Hutchinson M.R., Ash S.A. Resident’s ridge: assessing the cortical thickness of the lateral wall and roof of the intercondylar notch. Arthroscopy. 2003;19:931-935.
18 Kantaras A.T., Johnson D.L. The medial meniscal root as a landmark for tibial tunnel position in posterior cruciate ligament reconstruction. Arthroscopy. 2002;18:99-101.
19 Kaplan E.B. Comparative anatomy of the extensor digitorum longus in relation to the knee joint. Anat Rec. 1958;131:129-149.
20 Kaplan E.B. Surgical approach to the lateral (peroneal) side of the knee joint. Surg Gynecol Obstet. 1957;104:346-356.
21 Kaplan E.B. The fabellofibular and short lateral ligaments of the knee joint. J Bone Joint Surg Am. 1961;43:169-179.
22 LaPrade R.F. Anatomic reconstruction of the posterolateral aspect of the knee. J Knee Surg. 2005;18:167-171.
23 LaPrade R.F., editor. Posterolateral Knee Injuries. Anatomy, Evaluation, and Treatment. New York: Thieme; 2006:38. 238
24 LaPrade R.F., Hamilton C.D. The fibular collateral ligament–biceps femoris bursa. An anatomic study. Am J Sports Med. 1997;25:439-443.
25 LaPrade R.F., Konowalchuk B.K. Popliteomeniscal fascicle tears causing symptomatic lateral compartment knee pain: diagnosis by the figure-4 test and treatment by open repair. Am J Sports Med. 2005;33:1231-1236.
26 LaPrade R.F., Ly T.V., Wentorf F.A., Engebretsen L. The posterolateral attachments of the knee: a qualitative and quantitative morphologic analysis of the fibular collateral ligament, popliteus tendon, popliteofibular ligament, and lateral gastrocnemius tendon. Am J Sports Med. 2003;31:854-860.
27 LaPrade R.F., Morgan P.M., Wentorf F.A., et al. The anatomy of the posterior aspect of the knee. An anatomic study. J Bone Joint Surg Am. 2007;89:758-764.
28 LaPrade R.F., Tso A., Wentorf F.A. Force measurements on the fibular collateral ligament, popliteofibular ligament, and popliteus tendon to applied loads. Am J Sports Med. 2004;32:1695-1701.
29 Larson J.E., Becker D.A. Fabellar impingement in total knee arthroplasty. A case report. J Arthroplasty. 1993;8:95-97.
30 Lopes O.V.Jr., Ferretti M., Shen W., et al. Topography of the femoral attachment of the posterior cruciate ligament. J Bone Joint Surg Am. 2008;90:249-255.
30a Luites J.W., Wymenga A.B., Blankevoort L., Kooloos J.G. Description of the attachment geometry of the anteromedial and posterolateral bundles of the ACL from arthroscopic perspective for anatomical tunnel placement. Knee Surg Sports Traumatol Arthrosc. 2007;15:1422-1431.
31 Makris C.A., Georgoulis A.D., Papageorgiou C.D., et al. Posterior cruciate ligament architecture: evaluation under microsurgical dissection. Arthroscopy. 2000;16:627-632.
32 Mangieri J.V. Peroneal-nerve injury from an enlarged fabella. A case report. J Bone Joint Surg Am. 1973;55:395-397.
33 Marks P.H., Cameron M., Regan W. Fracture of the fabella: a case of posterolateral knee pain. Orthopedics. 1998;21:713-714.
34 Marshall J.L., Girgis F.G., Zelko R.R. The biceps femoris tendon and its functional significance. J Bone Joint Surg Am. 1972;54:1444-1450.
35 Mejia E.A., Noyes F.R., Grood E.S. Posterior cruciate ligament femoral insertion site characteristics: importance for reconstructive procedures. Am J Sports Med. 2002;30:643-651.
36 Minowa T., Murakami G., Kura H., et al. Does the fabella contribute to the reinforcement of the posterolateral corner of the knee by inducing the development of associated ligaments? J Orthop Sci. 2004;9:59-65.
37 Moorman C.T.3rd, LaPrade R.F. Anatomy and biomechanics of the posterolateral corner of the knee. J Knee Surg. 2005;18:137-145.
37a Moorman C.T.3rd, Murphy Zane M.S., Bansai S., et al. Tibial insertion of the posterior cruciate ligament: a sagittal plane analysis using gross, histologic, and radiographic methods. Arthroscopy. 2008;24:269-275.
37b Morgan C.D., Kalman V.R., Grawl D.M. The anatomic origin of the posterior cruciate ligament: Where is it? Reference landmarks for PCL reconstruction. Arthroscopy. 1997;13:325-331.
38 Noyes F.R., Barber-Westin S.D. Posterolateral knee reconstruction with an anatomical bone–patellar tendon–bone reconstruction of the fibular collateral ligament. Am J Sports Med. 2007;35:259-273.
39 Noyes F.R., Barber-Westin S.D. Surgical reconstruction of severe chronic posterolateral complex injuries of the knee using allograft tissues. Am J Sports Med. 1995;23:2-12.
40 Noyes F.R., Barber-Westin S.D. Surgical restoration to treat chronic deficiency of the posterolateral complex and cruciate ligaments of the knee joint. Am J Sports Med. 1996;24:415-426.
41 Noyes F.R., Barber-Westin S.D. Treatment of complex injuries involving the posterior cruciate and posterolateral ligaments of the knee. Am J Knee Surg. 1996;9:200-214.
42 Noyes F.R., Barber-Westin S.D., Albright J.C. An analysis of the causes of failure in 57 consecutive posterolateral operative procedures. Am J Sports Med. 2006;34:1419-1430.
43 Noyes F.R., Grood E.S. Classification of ligament injuries: why an anterolateral laxity or anteromedial laxity is not a diagnostic entity. Instr Course Lect. 1987;36:185-200.
44 Noyes F.R., Grood E.S., Butler D.L., Malek M. Clinical laxity tests and functional stability of the knee: biomechanical concepts. Clin Orthop. 1980;146:84-89.
45 Noyes F.R., Stowers S.F., Grood E.S., et al. Posterior subluxations of the medial and lateral tibiofemoral compartments. An in vitro ligament sectioning study in cadaveric knees. Am J Sports Med. 1993;21:407-414.
46 Pancoast H.K. Radiographic statistics of the sesamoid in the tendon of the gastrocnenius. Univ Penn Med Bull. 1909;22:213.
47 Pasque C., Noyes F.R., Gibbons M., et al. The role of the popliteofibular ligament and the tendon of popliteus in providing stability in the human knee. J Bone Joint Surg Br. 2003;85:292-298.
48 Petersen W., Zantop T. Anatomy of the anterior cruciate ligament with regard to its two bundles. Clin Orthop Relat Res. 2007;454:35-47.
48a Pritchett J.W. The incidence of fabellae in osteoarthritis of the knee. J Bone Joint Surg Am. 1984;66:1379-1380.
49 Robertson A., Jones S.C., Paes R., Chakrabarty G. The fabella: a forgotten source of knee pain? Knee. 2004;11:243-245.
50 Sanchez A.R.2nd, Sugalski M.T., LaPrade R.F. Anatomy and biomechanics of the lateral side of the knee. Sports Med Arthrosc. 2006;14:2-11.
51 Seebacher J.R., Inglis A.E., Marshall J.L., et al. The structure of the posterolateral aspect of the knee. J Bone Joint Surg Am. 1982;64:536-541.
52 Segond P. Reserches cliniques et experimentales sure es epachernents sanquins de genou par entarse. Prog Med. 1879;7:297.
53 Sheps D.M., Otto D., Fernhout M. The anatomic characteristics of the tibial insertion of the posterior cruciate ligament. Arthroscopy. 2005;21:820-825.
53a Siebold R., Ellert T., Metz S., Metz J. Tibial insertions of the anteromedial and posterolateral bundles of the anterior cruciate ligament: morphometry, arthroscopic landmarks, and orientation model for bone tunnel placement. Arthroscopy. 2008;24:154-161.
54 Simonian P.T., Sussmann P.S., van Trommel M., et al. Popliteomeniscal fasciculi and lateral meniscal stability. Am J Sports Med. 1997;25:849-853.
55 Standring S., editor. Gray’s Anatomy: The Anatomical Basis of Clinical Practice. New York: Churchill Livingstone, 2005.
56 Staubli H.-U., Birrer S. The popliteus tendon and its fascicles at the popliteal hiatus: gross anatomy and functional arthroscopic evaluation with and without anterior cruciate ligament deficiency. Arthroscopy. 1990;6:209-220.
57 Staubli H.U., Rauschning W. Tibial attachment area of the anterior cruciate ligament in the extended knee position. Anatomy and cryosections in vitro complemented by magnetic resonance arthrography in vivo. Knee Surg Sports Traumatol Arthrosc. 1994;2:138-146.
58 Strauss E.J., Ishak C., Inzerillo C., et al. Effect of tibial positioning on the diagnosis of posterolateral rotatory instability in the posterior cruciate ligament–deficient knee. Br J Sports Med. 2007;41:481-485. discussion 485
59 Sudasna S., Harnsiriwattanagit K. The ligamentous structures of the posterolateral aspect of the knee. Bull Hosp Jt Dis Orthop Inst. 1990;50:35-40.
60 Sutro C.J., Sutro W.H. Two concepts. I: The third femoral condyle. Bull Hosp Jt Dis Orthop Instr. 1991;51:40-46.
61 Takahashi M., Matsubara T., Doi M., et al. Anatomical study of the femoral and tibial insertions of the anterolateral and posteromedial bundles of human posterior cruciate ligament. Knee Surg Sports Traumatol Arthrosc. 2006;14:1055-1059.
61a Takahashi M., Doi M., Abe M., et al. Anatomical study of the femoral and tibial insertions of the anteromedial and posterolateral bundles of human anterior cruciate ligament. Am J Sports Med. 2006;34:787-792.
62 Terry G.C., Hughston J.C., Norwood L.A. The anatomy of the iliopatellar band and iliotibial tract. Am J Sports Med. 1986;14:39-45.
63 Terry G.C., LaPrade R.F. The biceps femoris muscle complex at the knee. Its anatomy and injury patterns associated with acute anterolateral-anteromedial rotatory instability. Am J Sports Med. 1996;24:2-8.
64 Terry G.C., LaPrade R.F. The posterolateral aspect of the knee. Anatomy and surgical approach. Am J Sports Med. 1996;24:732-739.
65 Watanabe Y., Moriya H., Takahashi K., et al. Functional anatomy of the posterolateral structures of the knee. Arthroscopy. 1993;9:57-62.
66 Weiner D., Macnab I., Turner M. The fabella syndrome. Clin Orthop Relat Res. 1977;126:213-215.
67 Wroble R.R., Grood E.S., Cummings J.S., et al. The role of the lateral extra-articular restraints in the anterior cruciate ligament–deficient knee. Am J Sports Med. 1993;21:257-262. discussion 263
68 Yoon K.H., Bae D.K., Ha J.H., Park S.W. Anatomic reconstructive surgery for posterolateral instability of the knee. Arthroscopy. 2006;22:159-165.
69 Zantop T., Petersen W., Sekiya J.K., et al. Anterior cruciate ligament anatomy and function relating to anatomical reconstruction. Knee Surg Sports Traumatol Arthrosc. 2006;14:982-992.
70 Zhao J., He Y., Wang J. Anatomical reconstruction of knee posterolateral complex with the tendon of the long head of biceps femoris. Am J Sports Med. 2006;34:1615-1622.