75 Lateral popliteal nerve palsy, L4, L5 (common peroneal nerve palsy)
Salient features
History
• History of trauma to the nerve particularly when it winds around the neck of the fibula where it is protected by only skin and fascia
• Whether the symptoms occur after sitting crossed leg for prolonged periods
• Recent weight loss, particularly in those who have been confined to bed rest (nerve more vulnerable because the protective fat and muscle is lost)
• History of diabetes, polyarteritis nodosa, collagen vascular diseases (all causes of mononeuritis multiplex, p. 226).
Examination
• Wasting of the muscles on the lateral aspect of the leg, namely the peronei and tibialis anterior muscle
• Weakness of dorsiflexion and eversion of the foot
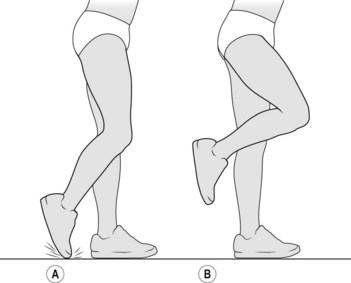
• High steppage gait (Fig. 75.1B)
• Loss of sensation on the lateral aspect of the leg and dorsum of the foot. If the deep peroneal branch is affected, the sensory loss may be limited to the dorsum of the web between the first and second toes.
Questions
Mention a few causes
• Compression resulting from application of a tourniquet or plaster of Paris casts. The nerve is vulnerable at the head of the fibula, where it lies on the surface of the hard bone with a covering of only skin
• Leprosy (commonest cause worldwide)
• Ganglion arising from the superior tibiofibular joint may compress the nerve
• Compression of the nerve by the tendinous edge of the peroneus longus.
Advanced-level questions
How would you manage such a patient?
• Nerve conduction studies: there may be a local conduction block or slowing in the region of the head of the fibula. There may denervation in the tibialis anterior and extensor digitorum profundus.
• If the intact nerve is severed: surgery.
• If the nerve is intact and concussed: 90 degree splint at night, calliper shoes with a 90 degree stop, and galvanic or faradic stimulation to maintain the bulk of the muscle until the nerve recovers.