Chapter 37 Lateral Interbody Fusion Using the Xlif System
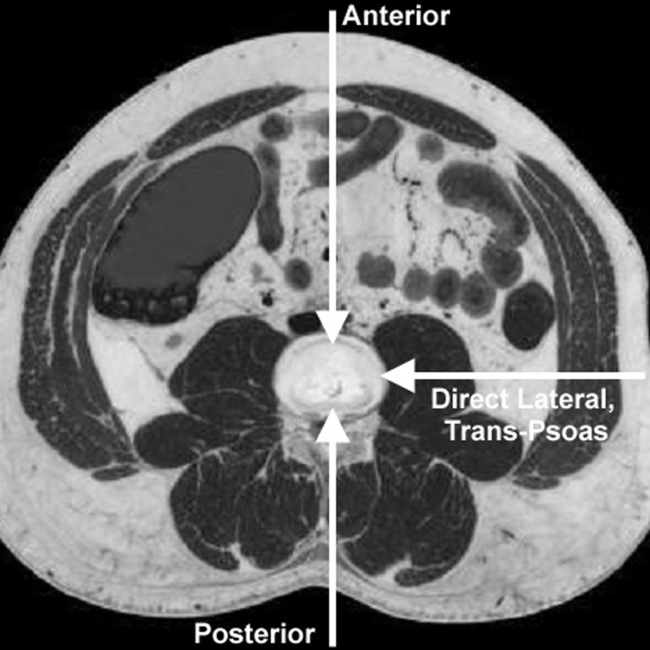
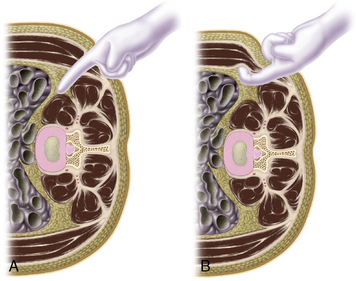
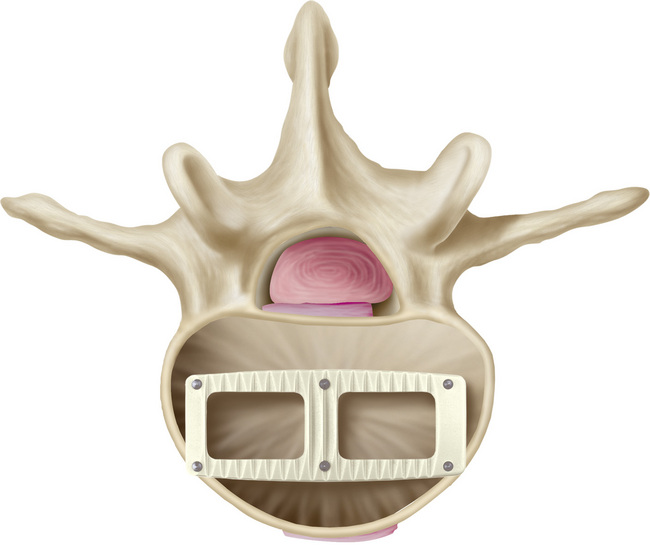
Building on the concept and technique of minimally invasive spinal approaches [1], we have developed the eXtreme Lateral Interbody Fusion (XLIF, NuVasive, Inc., San Diego, CA) approach to the lumbar spine. In contrast to the more traditional anterior lumbar interbody fusion (ALIF) method of approaching the disc anteriorly through the abdomen for implantation of cages and other devices, we have developed the XLIF technique, which accesses the disc laterally through the psoas muscle (Fig. 37-1). This approach offers adequate access to the disc space with the added benefit of reduced iatrogenic injury to abdominal vascular structures (aorta and vena cava), the sympathetic plexus (reducing incidence of retrograde ejaculation), and neural structures (namely, the spinal nerves that cross the posterior aspect of the psoas muscle). The technique employs muscle dilation through the fibers of the psoas muscle in an area approximately 3 cm in diameter.
Indications
Indications for the XLIF technique are the same as those for any interbody fusion, with the limitation of access only at disc levels above L5. Such patients typically suffer discogenic pain due to segmental instability, disc degeneration, degenerative scoliosis, and/or grade I or II spondylolisthesis [2–7]. It may also be applied to patients in whom prior decompressive surgery (i.e., discectomy and/or laminectomy) have failed and who therefore require interbody fusion, and in cases of adjacent-level disease after prior fusion surgery, because in these revision cases, scarring may limit the ability to safely perform a more traditional fusion approach. Revisions of failed interbody fusions and failed lumbar total disc replacements have also been treated with the XLIF approach for retrieval and revision.
Instrumentation
The instruments necessary for performing the XLIF procedure are as follows:
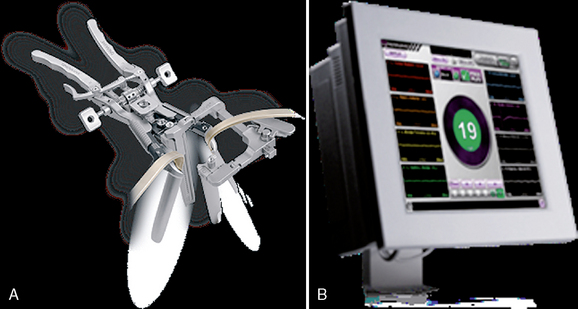
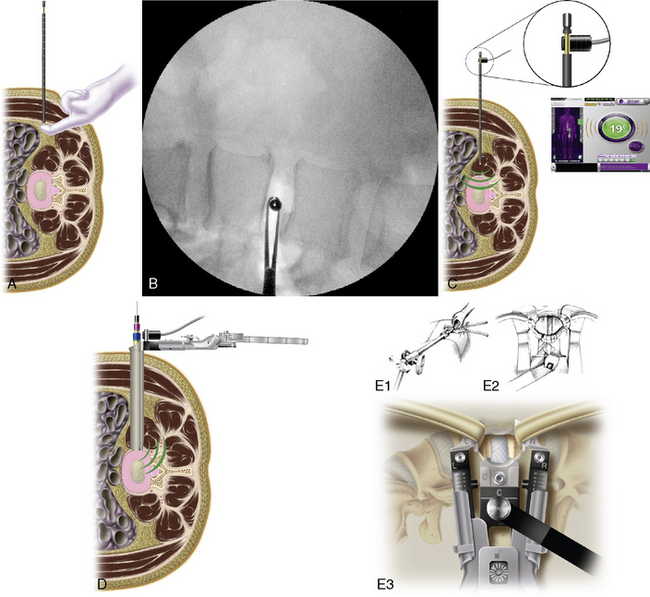
 MaXcess System of dilators and split-blade retractor (Fig. 37-2A; NuVasive, Inc.). Consists of bifurcated light cable, articulating arm, retractor system with various length blades, and blade-extension shims.
MaXcess System of dilators and split-blade retractor (Fig. 37-2A; NuVasive, Inc.). Consists of bifurcated light cable, articulating arm, retractor system with various length blades, and blade-extension shims. NeuroVision System for MaXcess-compatible stimulated and continuous electromyography (EMG) monitoring of nearby nerves (Fig. 37-2B; NuVasive, Inc.).
NeuroVision System for MaXcess-compatible stimulated and continuous electromyography (EMG) monitoring of nearby nerves (Fig. 37-2B; NuVasive, Inc.). Set of interbody instruments, such as curettes, Kerrison rongeurs, and dissectors of different sizes (available within XLIF and General Instrument Sets, NuVasive, Inc.).
Set of interbody instruments, such as curettes, Kerrison rongeurs, and dissectors of different sizes (available within XLIF and General Instrument Sets, NuVasive, Inc.).Surgical technique
Patient Preparation
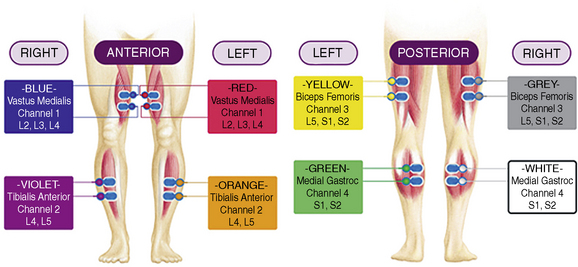
In the preoperative waiting area, the patient is prepared for NeuroVision EMG monitoring; four muscle groups per side can be monitored using the NeuroVision System. These four muscles are easily palpated and represent spinal nerve distributions from L2-S2: the vastus medialis, the anterior tibialis, the biceps femoris, and the medial gastrocnemius (Fig. 37-3). A reference electrode is also placed on the upper lateral thigh, and an anode return electrode is placed superior to the operative site, such as on the latissimus dorsi muscle.
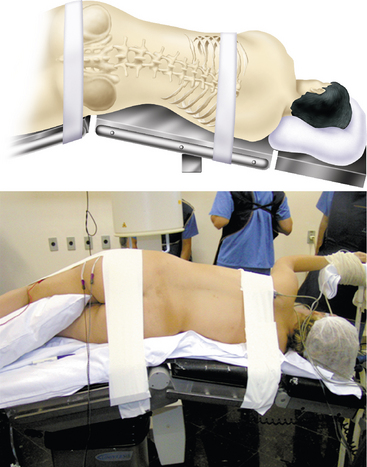
Patient Positioning
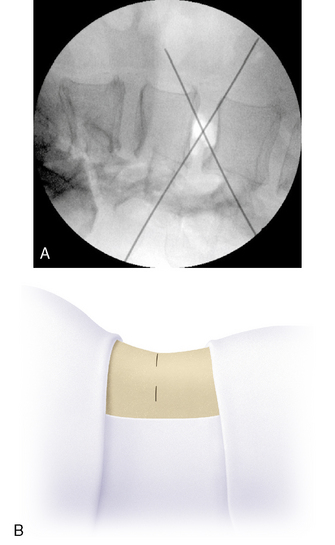
Incision Placement and Dissection
Preparing the Disc
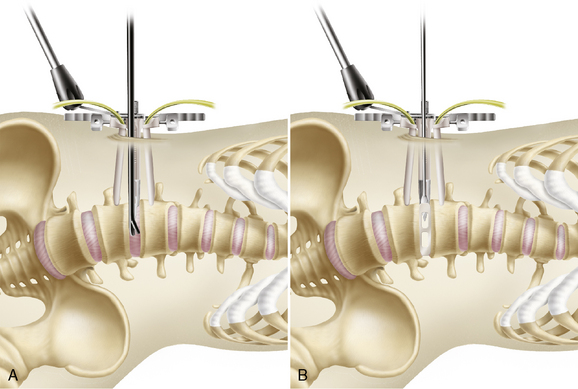
Device Implantation
The ideally placed implant is centered across the disc space from a mediolateral perspective, and between the anterior and middle thirds of the disc space from an anteroposterior perspective. Implants may be filled with cancellous bone graft from the iliac crest, bone morphogenetic protein, or any osteoinductive agent of choice (Fig. 37-10). The construct may be supplemented with the internal fixation system of choice.
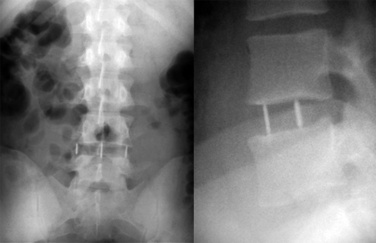
Case Series
Between July 1998 and October 2002, prior to the availability of the MaXcess and NeuroVision Systems, we implanted fusion devices in 69 patients using the technique described [8]. We accessed 74 discs spanning the levels L1-2 through L4-L5. The level most frequently operated was L4-L5 (55, 75%), followed by L3-L4 (15, 19.4%), L2-L3 (2, 2.8%), and L1-L2 (2, 2.8%). In 64 patients (92.5%), only one level was operated, and in 5 patients (7.5%),two levels were operated. Preoperative clinical evaluation revealed that 80% of the patients presented with VAS scores above 7 having lasted for more than 6 months. Postoperatively, the clinical improvement was excellent in 58.2% of patients, and good in 19.4%, rates similar to those reported in the literature [9]. Clinical improvements occurred between 6 days and 6 months after surgery, with an average of 3 months. Complications were minor and included one ureter injury that was repaired during the same procedure and a low incidence of transient psoas weakness that typically normalized after 1 week.
According to the authors, experience with this technique since that time has incorporated the specifically designed access instruments (MaXcess System) and procedure-based EMG monitoring (NeuroVision System). Anecdotal evidence shows continued success as well as improvements in surgical time, hospital stay, recuperation, and complication rates [10].
1 Burns B.H. An operation for spondylolisthesis. Lancet. 1933;224:1233-1239.
2 Fessler R.G. Minimally invasive surgery of the spine. Neurosurgery. 2000;51(Suppl.):3-4.
3 Hovorka I., Peretti F., Arcamone H., Argenson C. Five years experience of retroperitoneal lumbar and thoracolumbar surgery. Eur Spine J. 2000;9:S30-S34.
4 Iwahara T., Ikeda K., Hirabayashi K. Results of anterior spine fusion by extraperitoneal approach for spondylolisthesis. J Japan Orthop Assoc. 1963;36:1049-1067.
5 Lane L.D., Moore S.E. Transperitoneal approach to intervertebral disc in the lumbar area. Ann Surg. 1948;127:537-551.
6 Madan S.S., Boeree N.R. Comparison of instrumented anterior interbody fusion with instrumented circumferential lumbar fusion. Eur Spine J. 2003;12:567-575.
7 McAfee P.C., Regan J.R., Zdeblick T., et al. The incidence of complications in endoscopic anterior thoracolumbar spinal reconstructive surgery. Spine. 2000;20:1624-1632.
8 Pimenta L.H., Da Silva M.A. Avances Tecnológicos em Cirurgia de Coluna (workshop). São Paulo: Publicado em apostila, 2002. June
9 Tan L., Ng W., Slattery M. Outcomes Following Lumbar Spinal Fusion Surgery: A Comparison Of Preoperative And Postoperative Function. J Bone Joint Surg Br. 2008;91-B(Suppl. 3):431-432.
10 Pimenta L., Lhamby J., Gharzedine I., Coutinho E. Spine J. 2007;7(5):52S-53S.