CHAPTER 29 Lateral cutaneous nerve of thigh block
Clinical anatomy
The lateral cutaneous nerve of the thigh (L2, 3) (LCNT) is a purely sensory nerve. It emerges from the psoas muscle along its lateral border. It runs deep to the iliac fascia on the iliacus muscle, emerging immediately inferior and medial to the anterior superior iliac spine. After crossing under the inguinal ligament, it passes through the origin of the sartorius muscle and travels beneath the fascia lata, before dividing into a large descending branch and a smaller posterior branch, a variable distance below the inguinal ligament (Fig. 29.1). The branches pierce the fascia lata separately. The descending branch innervates the anterolateral thigh as far as the knee; the posterior branch innervates the lateral aspect of the thigh to mid-thigh level.
Surface anatomy
Important anatomic landmarks for block of the lateral cutaneous nerve of thigh include the anterior superior iliac spine and the inguinal ligament. The needle insertion site is located 2 cm medial and 2 cm inferior to the anterior superior iliac spine (Fig. 29.2). This should be below the inguinal ligament, unlike the needle insertion site for the ilioinguinal nerve block.
Sonoanatomy
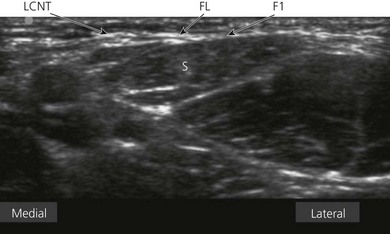
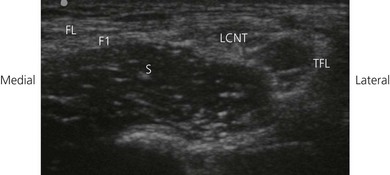
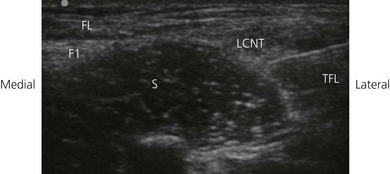
The LCNT nerve is found below the ASIS between the fascia lata and iliaca. These fascial layers are seen as hyperechoic lines. The appearance of the LCNT on ultrasound is as a round or oval hypoechoic (dark) area. Both branches of the LCNT cross the sartorius superficially. Due to the small size of the nerve and anatomical variability, a scanning routine is paramount. Scan initially with a transverse orientation in the medial thigh to identify the femoral vessels and nerve. With continued transverse scanning, move the transducer lateral and cephalad to identify the sartorius (triangular shape on transverse scan) insertion to the ASIS. Move the transducer caudally from here to the proximal third of the thigh (Fig. 29.3). The LCNT can be seen crossing the sartorius superficially or, alternatively, locate both fascial layers (fascia lata and iliaca) medial or lateral to the sartorius (Fig. 29.4). Injection of 5% dextrose between both fascial layers will help nerve visualization (Fig. 29.5). If the nerve is difficult to identify initially, a good focus point is the space between the sartorius and the more lateral tensor fascia lata. A sagittal oblique transducer orientation obtained by moving the medial aspect of the transducer to a slightly caudal position, parallel to the course of the nerve, can help identify the deep circumflex iliac artery (Fig. 29.6). This can be further identified with Doppler. This artery is crossed by the nerve, and can facilitate its identification (Fig. 29.6).
Technique
Ultrasound-guided approach
The operator stands on the side to be blocked, and with the patient in a supine position and the ipsilateral hip neutrally rotated (Fig. 29.7). The skin is disinfected with antiseptic solution and draped. A sterile sheath (CIVCO Medical Instruments, Kalona, IA, USA) is applied over the ultrasound transducer with sterile ultrasound gel (Aquasonic, Parker Laboratories, Fairfield, NJ, USA). Another layer of sterile gel is placed between the sterile sheath and the skin. The infrainguinal region is scanned with a 6–13 MHz linear transducer SonoSite MicroMaxx unit (SonoSite, Micromaxx, Bothwell, WA, USA). The ultrasound screen should be made to look like the scanning field. That is, the right side of the screen represents the right side of the field. Adjustable ultrasound variables such as scanning mode, depth of field, and gain are optimized.
A transverse image of the LCNT is obtained (Fig. 29.4). The LCNT nerve is kept in the center of the field of view. The needle entry site is at the lateral-most end of the transducer. A 23-gauge needle is inserted parallel to the axis of the beam of the ultrasound transducer, with the bevel facing the transducer (Fig. 29.8). It is important not to advance the needle without good visualization (Fig. 29.9). This may require needle or ultrasound adjustment.
Adverse effects
Brown TCK, Dickens DRV. A new approach to lateral cutaneous nerve of thigh block. Anaesth Intensive Care. 1986;14:126-127.
Damarey B, Demondion X, Boutry N, et al. Sonographic assessment of the lateral femoral cutaneous nerve. J Clin Ultrasound. 2009;37(2):89-95.
Dias Filho LC, Valença MM, Guimarães Filho FA, et al. Lateral femoral cutaneous neuralgia: an anatomical insight. Clin Anat. 2003;16(4):309-316.
Hurdle MF, Weingarten TN, Crisostomo RA, et al. Ultrasound-guided blockade of the lateral femoral cutaneous nerve: technical description and review of 10 cases. Arch Phys Med Rehabil. 2007;88(10):1362-1364.
Hopkins PM, Ellis FR, Halsall PJ. Evaluation of local anesthetic blockade of the lateral femoral cutaneous nerve. Anesthesia. 1991;46:95-96.
Ng I, Vaghadia H, Choi PT, Helmy N. Ultrasound imaging accurately identifies the lateral femoral cutaneous nerve. Anesth Analg. 2008;107(3):1070-1074.
Shannon J, Lang SA, Yip RW, Gerard M. Lateral femoral cutaneous nerve block revisited. A nerve stimulator technique. Reg Anesth. 1995;20(2):100-104.