3 Laser treatment of pigmented lesions and tattoos
Summary and Key Features
• Just as placement of tattoos has gained popularity, so has the number of people interested in their removal
• Black and blue tattoos are the easiest to fade with the most predictable results, whereas multicolored tattoos are the most difficult
• Of the various benign pigmented lesions that can be treated with laser, the easiest to treat are lentigines while the most difficult are the nevi of Ota, Ito, and Hori
• Pigment-specific lasers such as the quality-switched (QS) ruby (694 nm), QS alexandrite (755 nm), and QS Nd : YAG (532 nm and 1064 nm) continue to be the workhorse systems for both tattoo and pigmented lesion removal
• QS lasers remove tattoo pigment through photoacoustic injury, breaking up the ink particles and making them more available for macrophage phagocytosis and removal
• Fractional photothermolysis has provided expanded options for pigmented lesion removal in the last decade, though generally more treatment sessions are required and the cost is higher
• In general, patients with Fitzpatrick skin phototypes I–III have a better response than those with skin phototypes IV–VI as the lasers used for pigment removal can also damage epidermal pigment
• Topical anesthesia is helpful when treating dermal pigmented lesions and tattoos
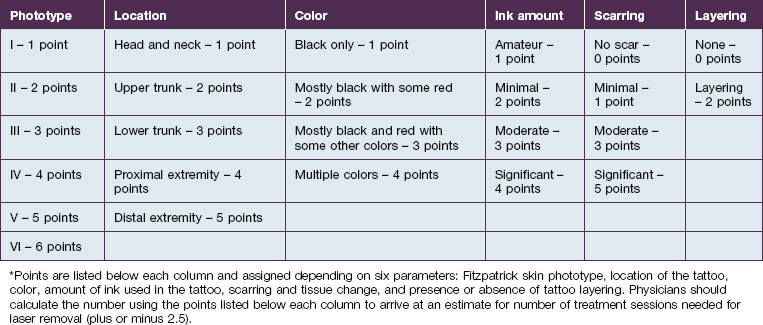
• Factors to consider prior to estimating the number of treatment sessions a patient will need for tattoo removal include: Fitzpatrick skin phototype, location, color, amount of ink used in the tattoo, scarring or tissue change, and ink layering
• As with any procedure, patient selection and preparation are important to success and photographs of the lesions should be taken prior to each treatment session
• Side effects of laser treatment for pigmented lesions include textural change, scarring, pruritus, hypo- or hyperpigmentation, and immediate pigment change
• Tattoos with white or red ink carry an increased risk of paradoxical darkening after laser treatment, which is why test spots should be carried out prior to the first treatment session
• Caution should be exercised prior to treatment of a tattoo with an allergic reaction as the dispersed ink particles can elicit a systemic response
• For pigmented lesions such as melasma and postinflammatory hyperpigmentation, pre- and postoperative treatment should include hydroquinone and topical retinoids
• Postoperative care includes gentle cleansing and a bland emollient while the skin heals
Pigment removal principles
QS lasers used for pigmented lesions include the QS ruby (694 nm), the QS alexandrite (755 nm) and the QS Nd : YAG (532 and 1064 nm) though it is also possible to use the long-pulsed ruby, alexandrite and diode lasers, or intense pulsed light (see Ch. 5). Within the last decade, fractional photothermolysis (‘FP’) has gained popularity for its ability to treat pigmented conditions such as melasma, solar lentigines, nevus of Ota, and postinflammatory hyperpigmentation (see Ch. 6).
Lesion selection
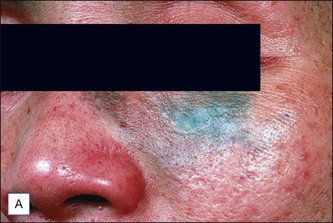
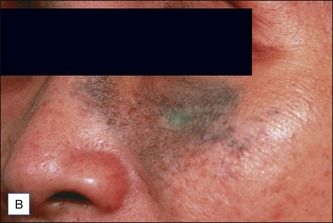
Just as important as patient selection is evaluation of the lesion itself. Tattoos can be divided into amateur, professional, cosmetic, medical, and traumatic categories. In amateur tattoos, a steel needle is used to deposit ink, which may be at various depths of the skin, whereas in professional tattoos, a hollow needle is used to inject ink into the dermal layer of skin. Amateur tattoos typically contain pigment of unknown sources such as ash, coal, or India ink (Fig. 3.1). On the other hand, professional tattoo artists often combine ink pigments to achieve novel colors and shading. Cosmetic tattoos using skin-colored tones are important to distinguish, as are medical tattoos such as those used as radiation markers. For traumatic tattoos, it is important to understand the nature of the injury that caused it so as to be aware of the type of material implanted in the skin prior to treatment.
Patient selection for tattoo removal
Though tattoos are increasingly popular, they often become a source of personal regret as up to 50% of adults older than 40 with tattoos seek their removal. It is critical that a thorough history of the tattoo be taken prior to deciding upon a treatment plan to establish appropriate patient expectations (Box 3.1). Kirby et al recently published a scale to help practitioners estimate the number of treatment sessions needed for tattoo removal to appropriately guide patients who often enter the laser removal process of their tattoos with uncertainty and misconceptions (Table 3.1). In the scale, numerical values are assigned to six parameters: (1) Fitzpatrick skin phototype, (2) location, (3) color, (4) amount of ink used in the tattoo, (5) scarring or tissue change, and (6) ink layering. The points for each parameter are combined, which results in the approximate number of treatment sessions needed to successfully remove the tattoo, plus or minus 2.5.
Box 3.1
Tattoo lesion patient history
 Is it an amateur, professional, traumatic, cosmetic, or medical tattoo?
Is it an amateur, professional, traumatic, cosmetic, or medical tattoo?
 What colors of inks / dyes were used?
What colors of inks / dyes were used?
 Were inks mixed together to make the colors?
Were inks mixed together to make the colors?
 Is there any white or skin-colored ink in the tattoo to the patient’s knowledge?
Is there any white or skin-colored ink in the tattoo to the patient’s knowledge?
 Has the patient attempted to remove or alter the tattoo previously? If so, what technique was used?
Has the patient attempted to remove or alter the tattoo previously? If so, what technique was used?
 Is the patient currently taking a retinoid?
Is the patient currently taking a retinoid?
 Is there a history of herpes infection or cold sores in the proposed treatment area?
Is there a history of herpes infection or cold sores in the proposed treatment area?
 Has the patient previously developed keloids or abnormal scars after prior surgery or injury?
Has the patient previously developed keloids or abnormal scars after prior surgery or injury?
 Does the patient currently actively pursue a tan or use a tanning bed or bronzer?
Does the patient currently actively pursue a tan or use a tanning bed or bronzer?
Patient selection for benign pigmented lesion removal
As with tattoo removal, it is important to assess the patient presenting for benign lesion removal (Box 3.2). The greater the contrast between background skin and pigmented lesion, the more likely the laser surgeon is to achieve success. At preliminary evaluation, a Wood’s lamp examination may be helpful to assess depth of pigment. Understanding whether the lesion is epidermal, present at the dermoepidermal junction, or dermal will guide laser selection and also allow the physician to set realistic expectations for removal.
Box 3.2
Pigmented lesion patient history
 How long has the lesion(s) been present?
How long has the lesion(s) been present?
 Has a biopsy of the lesion been performed?
Has a biopsy of the lesion been performed?
 Has it grown, bled without injury, or developed symptoms like itching or changed color?
Has it grown, bled without injury, or developed symptoms like itching or changed color?
 Has the patient attempted to remove or alter the lesion previously? If so, how was this attempted?
Has the patient attempted to remove or alter the lesion previously? If so, how was this attempted?
 Is the patient currently taking an oral retinoid?
Is the patient currently taking an oral retinoid?
 Is there a personal history of herpes infection or cold sores in the proposed treatment area?
Is there a personal history of herpes infection or cold sores in the proposed treatment area?
 Has the patient previously developed keloids or abnormal scars after prior surgery or injury?
Has the patient previously developed keloids or abnormal scars after prior surgery or injury?
 Does the patient currently actively pursue a tan or use a tanning bed or bronzer?
Does the patient currently actively pursue a tan or use a tanning bed or bronzer?
Treatment techniques
In general
Prior to commencing full treatment in darkly pigmented individuals, it is advisable to perform test spots on pigmented lesions or tattoos. Test spots should be evaluated at 4–6 weeks for hypo- or hyperpigmentation and efficacy. When using a QS laser, the initial desired response for epidermal and dermoepidermal pigmented lesions is immediate lesion whitening or graying, which represents cavitation. This may be more difficult to gauge if using an IPL system in which the primary endpoint in pigmented lesions is subtle darkening (see Ch. 5). Within 20–30 minutes, this gray converts to erythema. In dermal lesions, the immediate whitening is less vivid.
Case Study 1
Uneven tissue response in a black tattoo
AR is a 39-year-old man with an amateur tattoo on the hand. The tattoo appears black and the patient reports that his ‘friend put it there’. The patient does not have a tan. After icing the area for 15 minutes, the tattoo is treated with the QS Nd : YAG laser at a fluence of 3.0 J/cm2. The tattoo responds immediately and turns white and then erythematous. Unlike the rest of the tattoo, the central portion develops an erosion immediately upon treatment. This occurred because, in amateur tattoos, pigment is not placed at a uniform depth or in a uniform concentration. The tattoo was treated from the periphery to the center. While the periphery responded well, it was too much energy for the center, which led to immediate epidermal sloughing and pinpoint bleeding (Figs 3.1 and 3.2).
Patients and equipment for dark-blue or black tattoo treatment
Fitzpatrick skin phototypes I–III
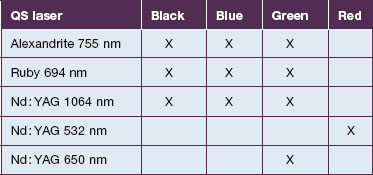
In lighter-skinned patients (in the absence of a tan or bronzer), the practitioner has several options (Table 3.2). The QS alexandrite (755 nm), the QS ruby (694 nm), and the QS Nd : YAG (1064 nm) lasers are all effective for dark-blue and black tattoos (Fig. 3.3). In the case of traumatic tattoos that appear black, it is important to know the origin of the trauma since such tattoos may react with a small explosion (e.g. gun powder tattoo) after laser treatment.
Patients and equipment for red tattoo treatment
The optimal laser wavelength for removing red tattoo ink is 532 nm (QS frequency-doubled Nd : YAG). This wavelength can cause both hyperpigmentation and hypopigmentation in darker-skinned patients so treatment should be limited to phototype I–III patients. It should be noted that red tattoo ink is often the culprit for allergic reactions after tattoo placement and granulomatous reactions in the tattoo itself (Fig. 3.4). Laser removal of the red ink can cause greater dispersion of the antigen resulting in urticaria or a systemic allergic reaction. In these cases, an ablative CO2 or Er : YAG laser can be employed to vaporize the tattoo (Fig. 3.5). If a QS-laser is employed, the patient should be covered with systemic corticosteroids and antihistamines and the laser surgeon should proceed with caution (Case study 2).
Case Study 2
When laser removal is not an option
TV is a 53-year-old woman who decided to have a red daisy on a green stem placed on her ankle 1 year ago. Approximately 3 months after getting the tattoo, she complained of itching in the area and noticed a gradual thickening of the skin. She had not experienced this with her other tattoos and has one on the dorsal foot of the same lower extremity that was normal in appearance. She tried clobetasol cream to the area, which initially helped and then failed and then she used flurandrenolide (Cordran®) tape, which worked to alleviate the itch but not the size of the reaction in the area. On exam, the patient is skin phototype V with a thick plaque on the ankle in which one can begin to make out individual flower petals. No visible red ink remained but the green stem was still present. Given her background skin tone and history of red ink, the decision was made to forgo laser therapy of the area in favor of surgical excision. The pathology showed a pseudolymphoma resulting from a granulomatous reaction to the red ink. In this case, QS laser therapy would have been of minimal benefit and surgical therapy became the mainstay of treatment (Fig. 3.6).
Patients and equipment for epidermal lesions
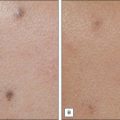
Solar lentigines, lentigo simplex, and ephelides
Pigment that is in the epidermis accounts for lesions such as solar lentigines, lentigo simplex, and ephelides. Any laser system that damages the epidermis will therefore result in improvement in 1–2 treatment sessions (Fig. 3.7). Conversely, if the epidermal damage is part of a deeper destruction, there may be scarring or dyspigmentation afterward. Fractional photothermolysis can be considered for these conditions especially if the lesions are widespread (see Ch. 6), but the mainstay lasers are the QS alexandrite, QS Nd : YAG (532 nm), and QS ruby lasers. Long-pulsed lasers and IPL can also be effective (see Ch. 5).
Labial melanotic macules
Melanotic macules on the lip vermilion are a feature of several entities including physiological racial pigmentation, Laugier-Hunziker syndrome, and Peutz-Jeghers syndrome. These can be treated using the QS ruby or QS alexandrite or frequency-doubled QS Nd : YAG lasers. In the case of the syndromes, patients should be made aware that new macules will develop over time (Fig. 3.8).
Café au lait macules and nevus spilus
Café-au-lait macules (‘CALM’) vary in color, size, and shape but histologically the excess pigment is found at the basal layer. When darker macules exist with the CALM, it is referred to as a nevus spilus. Before treating CALMS, one should always take a careful history to rule out neurofibromatosis (if multiple macules exist). Lasers that are usually used to treat these lesions include the QS Nd : YAG, QS ruby, and QS alexandrite lasers. Patients with darker skin are at risk for hyperpigmentation and hypopigmentation. Light-skinned patients are the ideal candidates for CALM removal, but recurrences, residual hyperpigmentation, and incomplete pigment removal are common. Treatment sessions are spaced at least 8 weeks apart and clearance requires at least 2–4 treatment sessions (Fig. 3.9).
Patients and equipment for dermoepidermal lesions
Becker’s nevus
The hyperpigmented areas of a Becker’s nevus have shown improvement when treated with the QS ruby, QS Nd : YAG, and 1550 nm fractional erbium-doped fiber laser. Of the QS lasers, the ruby is slightly more effective than the Nd : YAG. Treatment sessions should be spaced 8–12 weeks apart and 3–5 treatment sessions are usually necessary. With any of these methods, fading is generally incomplete and patchy. The terminal hairs can be removed with hair removal lasers (see Ch. 4).
Postinflammatory hyperpigmentation
PIH occurs due to hemosiderin and / or melanin deposition. Because this condition arises due to inflammation, it is important to use low fluences and ensure that the patient does not develop significant post-treatment erythema to provoke additional PIH. For this reason, test spots are encouraged prior to treating large areas. The laser system currently used most often for PIH is the fractional photothermolysis system, even though treatment with this laser has been reported to induce PIH itself (see Ch. 6). PIH can occur on the face, but can also be a result of hemosiderin deposition after sclerotherapy. For post-sclerotherapy hyperpigmentation, the QS ruby or IPL (see Ch. 5) can be used (Fig. 3.10). All patients being treated for PIH on the face should use topical hydroquinone 4% cream along with a broad-spectrum sunscreen before and after treatment. Before using a laser for facial PIH, we recommend a trial of topical retinoids and a series of chemical peels to try to improve the discoloration with laser as the final step. Recurrence is frequently seen, especially after sun exposure.
Patients and equipment for dermal lesions
Nevi of Ota, Ito, and Hori
Nevus of Ota presents on the face as a blue-black, brown, or gray patch that develops after birth or in adolescence with a unilateral distribution that may involve the sclera. Nevus of Ito is similar, but its location is usually on the shoulder. Hori’s nevus is typically bilateral and located in the malar region. In darker-skinned (type IV–VI) patients, the QS Nd : YAG laser at 1064 nm is usually the safest laser to lighten a nevus of Ota, Ito or Hori. In lighter-skinned patients, QS ruby laser at 694 nm and QS alexandrite laser at 755 nm can also be used (Fig. 3.11). Recently, a fractionated 1440 nm Nd : YAG laser has been reported to clear nevus of Ota. Treatments are usually spaced 3–4 months apart with up to 10 treatment sessions needed for clearance with QS lasers, and 2–3 treatment sessions with the fractionated laser. Nevus of Ota patients should be made aware that the sclera component of the lesion is not amenable to treatment with current technology.
Postoperative care
If an IPL system was used for treatment, typically only erythema is seen postoperatively and dressings are not generally required (see Ch. 5). After fractional photothermolysis, broad-spectrum sunscreen and non-comedogenic moisturizer should be applied for at least 1 week (see Ch. 6).
Side effects and complications
Special situations
Multicolored tattoos
When treating a tattoo of multiple colors, especially black, red, or green, more than one laser may be required to maximize the degree of improvement. In these situations, the black outline of the tattoo is usually first treated with infrared light from the QS Nd : YAG laser operated at 1064 nm. Once that portion of the treatment has been completed, the green light from the frequency-doubled QS Nd : YAG laser operated at 532 nm is used to treat the red portions of the tattoo. If green tattoo ink is also present, red light from the Q-switched ruby or alexandrite lasers is used. Alternatively, the QS Nd : YAG with a 650 nm wavelength dye-containing handpiece can be used as well. Care should be taken to avoid overlapping the treatment pulses as much as possible by matching the size of the laser beam to the amount of the tattoo color being treated. By using this technique, it is often possible to treat the entire tattoo at one time resulting in more rapid resolution of the different colors than if they were treated individually at different visits. Other colors respond unpredictably to specific wavelengths with the treatment done mostly by trial and error. If prominent immediate whitening in the tattoo ink is noted, that laser wavelength will tend to achieve fading of that color (Table 3.3).
Table 3.3 Tattoo pigments used to create specific tattoo colors
| Tattoo color | Source |
|---|---|
| Black | Carbon, iron oxide, India ink, lead, gunpowder |
| Red | Cinnabar (mercuric sulfide), cadmium selenide, sienna, azo dyes |
| Green | Chromium oxide, malachite green, hydrated chromium sesquioxide, lead chromate |
| Blue | Cobalt aluminum |
| Brown | Ochre |
| Yellow | Cadmium sulfide, ochre, curcumin yellow |
| Violet | Manganese violet |
| White | Titanium dioxide, zinc oxide |
Adrian RM, Griffin L. Laser tattoo removal. Clinics in Plastic Surgery. 2000;27:181–192.
Anderson RR, Geronemus R, Kilmer SL, et al. Cosmetic tattoo ink darkening. A complication of Q-switched and pulsed-laser treatment. Archives of Dermatology. 1993;129(8):1010–1014.
Anderson RR, Parrish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science. 1983;220(4596):524–527.
Armstrong ML, Roberts AE, Koch JR, et al. Motivation for contemporary tattoo removal a shift in identity. Archives of Dermatology. 2008;144:879–884.
Ashinoff R, Levine VJ, Soter NA. Allergic reactions to tattoo pigment after laser treatment. Dermatologic Surgery. 1995;21(4):291–294.
Choi JE, Kim JW, Seo SH, et al. Treatment of Becker’s nevi with a long-pulsed alexandrite laser. Dermatologic Surgery. 2009;35:1105–1108.
Duke D, Byers HR, Sober AJ. Treatment of benign and atypical nevi with the normal-mode ruby laser and the Q-switched ruby laser: clinical improvement but failure to completely eliminate nevomelanocytes. Archives of Dermatology. 1999;135:290–296.
Fitzpatrick RE, Goldman MP. Tattoo removal using the alexandrite laser. Archives of Dermatology. 1994;130(12):1508–1514.
Grevelink JM, Duke D, van Leeuwen RL, et al. Laser treatment of tattoos in darkly pigmented patients: efficacy and side effects. Journal of the American Academy of Dermatology. 1996;34(4):653–656.
Hantash BM, Bedi VP, Sudireddy V, et al. Laser-induced transepidermal elimination of dermal content by fractional photothermolysis. Journal of Biomedical Optics. 2006;11:041115.
Jeong SY, Shin JB, Yeo UC, et al. Low-fluence Q switched neodymium-doped yttrium aluminum garnet laser for melasma with pre- or post-treatment triple combination cream. Dermatologic Surgery. 2010;36:1–10.
Kagami S, Asahina A, Watanabe R, et al. Laser treatment of 26 Japanese patients with Mongolian spots. Dermatologic Surgery. 2008;34:1689–1694.
Katz TM, Goldberg LH, Firoz BF, et al. Fractional photothermolysis for the treatment of postinflammatory hyperpigmentation. Dermatologic Surgery. 2009;35:1844–1948.
Kilmer SL, Anderson RR. Clinical use of the Q-switched ruby and the Q-switched Nd:YAG (1064 nm and 532 nm) lasers for treatment of tattoos. Journal of Dermatologic Surgery and Oncology. 1993;19(4):330–338.
Kilmer SL. Laser eradication of pigmented lesions and tattoos. Dermatologic Clinics. 2002;20:37–53.
Kirby W, Desai A, Desai T, et al. The Kirby-Desai scale: a proposed scale to assess tattoo-removal treatments. Journal of Clinical and Aesthetic Dermatology. 2009;2(3):32–37.
Kono T, Nozaki M, Chan HH, et al. A retrospective study looking at the long-term complications of Q-switched ruby laser in the treatment of nevus of Ota. Lasers in Surgery and Medicine. 2001;29:156–159.
Laubach H, Tannous Z, Anderson RR, et al. Skin responses to fractional photothermolysis. Lasers in Surgery and Medicine. 2006;38:142–149.
Laumann AE, Derick AJ. Tattoos and body piercings in the United States: a national data set. Journal of the American Academy of Dermatology. 2006;55:413–421.
Polder KD, Landau JM, Vergilis-Kalner IJ, et al. Laser eradication of pigmented lesions: a review. Dermatologic Surgery. 2011;37:572–595.