10 Laser treatment of ethnic skin
Summary and Key Features
• The use of lasers and lights can be safe and effective in ethnic skin
• Sun protection pre- and post-treatment, together with the use of bleaching agents, is important in reducing the risks of post inflammatory hyperpigmentation
• Q-switched and long pulsed lasers are both useful in the treatment of epidermal pigmentation; however, in ethnic skin, long-pulsed lasers are preferred as they have similar efficacy with less side effects
• Using a small spot size avoids inadvertent treatment of surrounding normal skin, which can increase the risk of hyperpigmentation when the contrast between lesional and non-lesional skin is low
• Diascopy during treatment of pigmented lesions reduces the risk of vascular damage
• Longer wavelength lasers allow for dermal pigmentation to be treated
• Q-switched 1064 nm Nd : YAG laser, in conjunction with 1550 nm fractional resurfacing, can achieve optimal results in the treatment of nevus of Ota
• Hori’s macules can be resistant to treatment, requiring multiple treatments. There is also a risk of initial darkening of pigmentation before subsequent lightening with further treatments
• Melasma is a common pigmentary condition in ethnic skin and a challenge to treat. Topical bleaching agents should be used before laser therapy is considered
• Non-ablative fractional resurfacing using lower densities but increasing the number of treatment sessions is recommended for ethnic skin
Treatment of epidermal pigmentation
Freckles and lentigines
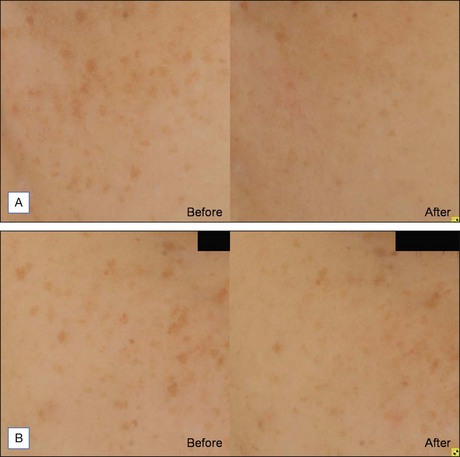
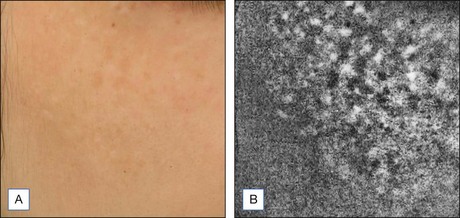
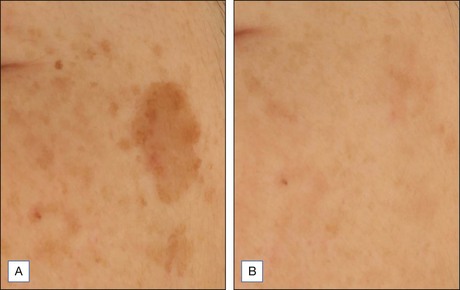
As melanin has a broad absorption spectrum ranging from 250 to 1200 nm, various lasers have been used to target cutaneous pigmentation, usually with excellent results. Anderson et al were the first to demonstrate the effectiveness of Q-switched (QS) lasers in the treatment of cutaneous pigmentation. Frequency-doubled QS neodymium : yttrium-aluminum-garnet (Nd : YAG), QS ruby, and QS alexandrite lasers with respective wavelengths of 532 nm, 694 nm, and 755 nm, have all been used with good results in lighter-skinned patients but PIH risk of 10–25% has been reported when used on ethnic skin. Chan et al compared 532 nm frequency-doubled Nd : YAG lasers with different pulse durations in the treatment of facial lentigines in Chinese patients, and found similar efficacy between QS 532 nm Nd : YAG and long pulsed (LP) 532 nm Nd : YAG, but a higher risk of postoperative hyperpigmentation with the QS device. A recent study by our group comparing QS and LP alexandrite for the treatment of freckles and lentigines in 20 Chinese patients showed similar results (Fig. 10.1). There was significant improvement in pigmentation in both groups, with no difference between the groups. However, the risk of PIH was 22% in the QS group, compared with 6% in the LP group. Patients also complained of more severe pain, erythema, and edema with the QS device. These findings were further validated in a retrospective study due to be published, comparing treatment of lentigines in 40 Chinese patients with four different devices; 595 nm long pulsed dye laser (LPDL), 755 nm alexandrite laser, 532 nm QS Nd : YAG, and 532 nm LP potassium-titanyl-phosphate (KTP) laser (Fig. 10.2). The results showed that a long pulse laser and small spot size appear to reduce the risk of PIH in darker skin types (see Case study 1 at end of chapter).
A treatment algorithm for epidermal pigmentation is as follows:
1. IPL can be recommended for patients who are intolerant of any PIH risk, and are amenable to having several treatment sessions.
2. LP lasers are effective, yet require fewer treatments than IPL, and carry a low PIH risk.
3. The more aggressive approach using QS lasers only requires one to two sessions, but carries the highest risk of PIH and downtime of a week. This should be reserved for patients with time and cost constraints.
Treatment of dermal pigmentation
Nevus of Ota
Nevus of Ota is an oculodermal melanocytosis affecting approximately 0.6% of the Asian population at birth or developing in their teens. Clinically, it presents as a bluish-black hyperpigmentation along the ophthalmic or maxillary branches of the trigeminal nerve. QS lasers, including QS ruby, QS alexandrite, and QS 1064 nm Nd : YAG, have all been used to achieve good therapeutic results.Watanabe and Takahashi looked at 114 nevus of Ota patients treated with QS Ruby and reported a good to excellent degree of lightening after three or more sessions. Kono et al confirmed the findings when he reviewed 101 nevus of Ota patients treated with QS Ruby and reported 56% achieving 75% improvement, and 36% achieving complete clearing. Hypopigmentation was seen in 17% of patients and hyperpigmentation in 6%. Studies comparing the use of QS alexandrite and QS 1064 nm Nd : YAG found the former better tolerated but the latter more effective after three or more treatment sessions. The longer wavelength of the QS Nd : YAG targets dermal pigment effectively with minimal epidermal damage in darker skinned individuals (Fig. 10.3). More recently, fractionated laser technology has been added to the currently available options. Near-complete clearance of a case of nevus of Ota after serial therapy using 1064 nm QS Nd : YAG, followed by 1550 nm non-ablative fractionated erbium-doped fiber laser treatments at 2-month intervals; and a further case achieving complete clearance with sequential same day therapy with the same devices have been reported. Treatment of nevus of Ota at a younger age requires fewer treatment sessions and is associated with fewer complications compared with older patients, and early treatment is therefore recommended (see Case study 2). It is important to note that the risk of recurrence is estimated to be between 0.6% and 1.2%8, which has important implications particularly when counseling pediatric patients.
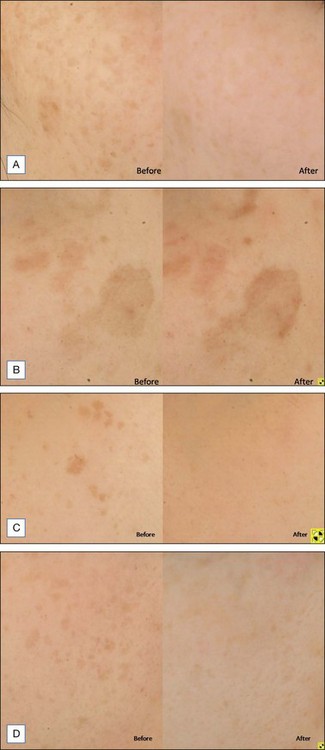
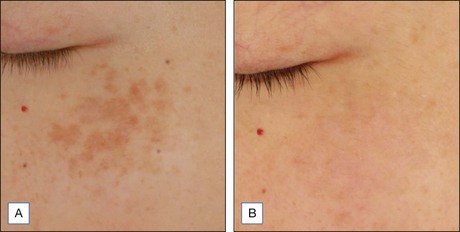
Hori’s macules or acquired bilateral nevus of Ota-like macules
Hori’s macules (ABNOM) affect 0.8% of the Asian population and presents in late adulthood as bluish brown dermal hyperpigmentation typically affecting the bilateral malar regions, forehead and temples of middle aged women, without any mucosal involvement. QS lasers such as QS ruby, QS alexandrite and QS 1064 nm Nd : YAG have been found to be effective in the treatment of Hori’s macules. More recent studies also support these results. Kagami et al reported the efficacy of QS alexandrite in 24 Japanese patients, with 45.8% reporting greater than 50% improvement. Cho et al also evaluated the use of 1064 nm QS Nd : YAG at low fluences in 15 patients, 80% of whom had greater than 50% improvement. From our experience, Hori’s macules tend to be more resistant to treatment than nevus of Ota. Shorter treatment intervals every 4 weeks tend to yield better results. Combination treatment with QS 532 nm Nd : YAG, followed by QS 1064 nm Nd : YAG has also been found to be more effective than the 1064 nm wavelength alone. Transient PIH is a common adverse event, occurring in the majority of treated patients (Fig. 10.4). Permanent hypopigmentation has been reported after QS ruby treatment. In order to reduce the risk of PIH, all patients should be given pre and post-treatment bleaching agents (see Case study 3).
Treatment of dermo-epidermal pigmentation
Becker’s nevus
Becker’s nevus commonly presents as a brown irregular patch accompanied by dark, coarse hair. It usually appears in adolescence and in males. Histologically, increased melanin is seen in the basal cells, and melanophages may be present in the papillary dermis. It is a benign condition with no reports of malignant transformation. Previously, lasers such as QS ruby and QS Nd : YAG have been shown to improve such lesions. A comparative study of the two devices showed mean clearance of at least 43% after a single treatment with either laser. Trelles et al later compared the use of Er : YAG laser and QS 1064 nm Nd : YAG in 22 patients. At 2 years’ follow-up, 54% of patients (n = 6) achieved complete clearance after a single treatment with Er : YAG, compared with just 1 out of 11 patients reporting clearance after three treatment sessions of Nd : YAG laser. Although clinically effective, ablative laser carries a high risk of adverse effects, especially in darker skin types. QS lasers rarely achieve complete clearance, and multiple treatments are necessary. More recently, fractional resurfacing has been suggested by Glaich and colleagues as a promising new treatment modality, with two cases reporting at least 75% pigment reduction after five to six treatments with 1550 nm erbium-doped fiber laser at 4-week intervals. Long-pulsed pigment lasers have also been employed successfully to target both pigment and hair in Becker’s nevus. In our experience, LP alexandrite (20–35 J/cm2, 10 mm spot size, pulse duration 1.5 ms) gives a 50% success rate after four to eight treatments. Possible side effects include scarring and hypopigmentation. Long-pulsed pigment laser together with non-ablative fractional resurfacing with 1927 nm thulium fiber laser can lead to an optimal outcome (see Case study 4).
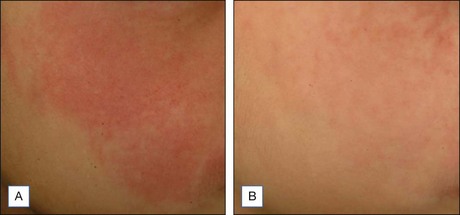
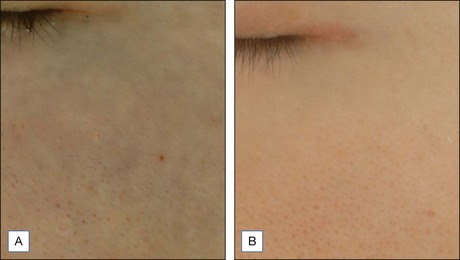
Melasma
Pigment lasers have also been used to treat melasma. Low fluence, large spot size, multiple pass QS 1064 nm Nd : YAG, sometimes referred to as laser toning or laser facial, has become increasingly popular for the treatment of melasma. Some studies have reported it to be effective and safe, while others have highlighted important complications. Zhou et al published a recent study examining 50 patients with melasma treated with 9 weekly sessions, and reported 70% with more than 50% reduction in melasma area and severity index (MASI) values, and 10% with complete clearance. However, the recurrence rate at 3 months was 64%. Promising results were similarly reported in a prospective study by Polnikorn, after 10 weekly sessions of 1064 nm Nd : YAG in 35 refractory melasma cases. Recurrence at 6 months was seen in two cases. In addition, he noted mottled hypopigmentation occurring in three patients. Facial depigmentation is an increasingly recognized phenomenon often encountered with frequent treatments with QS 1064 nm Nd : YAG (Fig. 10. 5). Chan et al reported it in 14 Chinese patients, after a variable number of such treatments. Wattanakrai et al and Cho et al also described a similar adverse effect occurring after 1 to 2 weekly treatments with this laser for melasma, with 13.6% and 8% rate of hypopigmentation reported, respectively. With risks of recurrence and punctate hypopigmentation post-laser treatment, patients need to be adequately informed of potential complications prior to embarking on such treatments for melasma. Optimal parameters from future studies will be helpful.
Post-inflammatory hyperpigmentation (PIH)
Different lasers have been used to improve PIH. Vascular lasers, such as the 595 nm LPDL, target mainly oxyhemoglobin, and can be used to treat the vascular component of the inflammatory process. When used with compression, Kono and colleagues reported that it can also be effective for pigment removal. QS lasers, such as QS Nd : YAG and QS alexandrite, have long been successfully used to treat cutaneous pigmentation. Depending on the wavelength used, epidermal and dermal pigmentation can be targeted accordingly. In recalcitrant PIH where dermal pigment may be present, 1064 nm QS Nd : YAG has been successfully used in previous reports with minimal adverse effects. More recently, our group examined the management of acne PIH in Chinese patients, and suggested the use of bleaching agents for the initial 3 months, followed by combination topical and laser therapy (LPDL and / or 1064 nm QS Nd : YAG) for recalcitrant PIH with vascular and dermal components (Fig. 10.6). Laser treatment in itself can of course be a cause of PIH in darker skin types, and strategies to reduce PIH risk include effective sun protection pre- and post-procedure, the use of long-pulsed lasers, cooling, diascopy, and small spot sizes in this group.
Melanocytic nevi
A typical treatment protocol is as follows: long-pulsed pigment laser (LP alexandrite 755 nm, 3 ms, 10 mm spot size, 15–25 J/cm2 depending on the degree of pigmentation with slight dark gray appearance being the endpoint), to be followed immediately by QS ruby laser (4 mm spot size, 3–4 J/cm2 with immediate whitening as the end point). 4–6 weeks later, the patient will be treated with non-ablative fractional resurfacing using a combination of 1550 nm and 1927 nm wavelengths (1550 nm, 4 passes, 50 mJ, treatment level 10, to be followed by 1927 nm, 4 passes, 20 mJ, treatment level 10). Such alternate treatment at 4–6 weekly intervals is performed until the nevi completely lighten (see Case study 5).
Treatment of vascular lesions
Asahina et al evaluated the use of 595 nm PDL (7 mm spot size, 10 ms pulse duration, 12 J/cm2) in the treatment of PWS in skin type IV patients, and found 67% of patients achieving good or excellent results after four treatments at 8-week intervals. Hyper and hypopigmentation were seen in up to 17% and 14% respectively. Epidermal cooling and protection enhances efficacy by allowing a higher fluence to be used to achieve the desired end point of purpura with better tolerability and less side effects in darker skin types (585 nm PDL, 7 mm spot size, 1.5 ms, 7–13 J/cm2, dynamic cooling device with 20 ms spray and 30 ms delay interval) (Fig. 10.7). However, complete blanching of PWS is rarely seen. It has been postulated that regeneration and revascularization of photocoagulated blood vessels due to angiogenesis occur as part of the skin’s normal healing process. The heterogeneity of vessels characteristic of PWS require the use of different spot sizes, fluences, pulse widths, and dynamic cooling, depending on vessel size and anatomical location. Due to a greater risk of dyspigmentation when treating lip PWS with PDL, a 1064 nm Nd : YAG is recommended. Combined 595 nm and 1064 nm laser irradiation has also been recommended for recalcitrant and hypertrophic PWS.
Ablative, non-ablative, and fractional skin resurfacing
Radiofrequency has been used successfully for non-invasive skin rejuvenation. The radiofrequency device delivers an electric current that nonselectively generates heat by the tissue’s natural resistance to the flow of ions. Epidermal cooling from the cooling tip protects against melanin disruption, and radiofrequency can be safely applied to any skin type. Such delivery of energy deep into 2–4 mm of the dermis induces subtle collagen damage and subsequent healing and remodeling, resulting in immediate skin tightening, and further improvement after several months. Monopolar radiofrequency is considered the gold standard in non-invasive skin tightening but can be limited by pain issues (Fig. 10.8). Patient feedback on heat sensation is thought to be a valid and preferred method for optimal energy selection. Multiple passes at moderate energy settings have yielded good and consistent results. Newer models have incorporated a vibrating handpiece, in order to reduce the sensation of pain, in accordance with the gate theory.
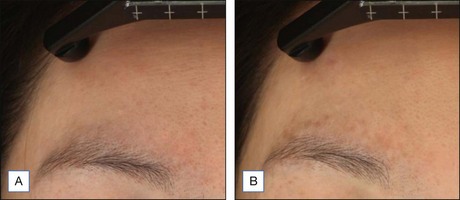
Focused ultrasound is another new technology that translates ultrasound into thermal energy; in addition, it allows imaging of the tissue before application of the focused ultrasound directly to the target area. A preliminary study on 49 Chinese patients has shown early promising results with significant improvement to the lower face and a good safety profile with only transient bruising, erythema, edema, and PIH described (Fig. 10.9).
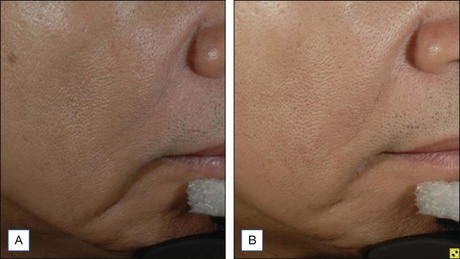
Figure 10.9 (A) Baseline and (B) 3 months after focused ultrasound treatment; treatment parameter: 1.2 J.
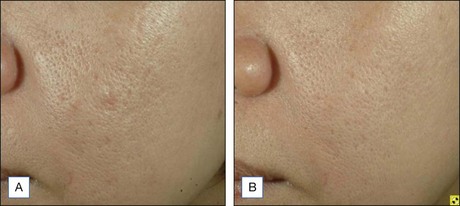
The development of fractional photothermolysis has revolutionalized skin rejuvenation and resurfacing, attempting to achieve comparable clinical results to ablative lasers, but with a safety profile more similar to non-ablative technologies. The 1550 nm erbium-doped fiber non-ablative laser is the first fractional laser approved for clinical use. By creating an array of microscopic treatment zones (MTZs) with controlled width, depth, and density, a fixed percentage of the skin is thermally coagulated in each treatment session, leaving an intact stratum corneum. Healthy tissue surrounding these MTZs allow for rapid healing and re-epithelialization within 1 day. This technology has proven to be effective in improving photoaging, dyschromia, rhytides, atrophic scarring, and poikiloderma. Non-ablative fractional resurfacing (NA FR) used for acne scarring in Asian skin carries a high risk of PIH. Studies have indicated that treatment density, rather than energy, is a stronger determining factor in the development of PIH. Further studies by Chan and colleagues have confirmed that by reducing the number of passes and the total treatment density (four rather than eight passes), but increasing the treatment sessions from three to six to compensate for the reduced passes, clinical efficacy remains statistically improved whilst reducing the PIH risk in Asians from 18.2% to 6% (Fig. 10.10).
Case studies
Case Study 1
Freckles and lentigo
A 55-year-old female who enjoys outdoor activities and sunbathing presents with troubling pigmentation on her face (Fig. 10.11A–D), which has been increasing in numbers in recent years. She does not use sunscreens and continues to play golf on a regular basis. She has a busy job that requires her to meet with clients on a daily basis and requests a treatment with little downtime.
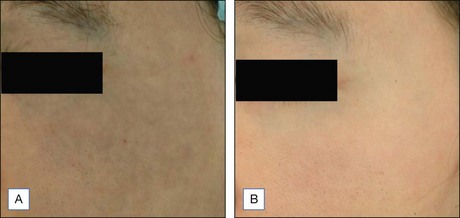
Case Study 2
Nevus of Ota
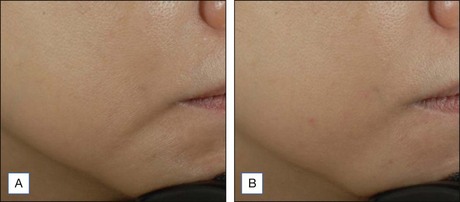
A 23-year-old Chinese male presents with a bluish-gray patch over his left forehead, temple, malar area, and periorbital skin (Fig. 10.12A,B). It has been present since infancy and has gradually enlarged and darkened in color over the years. It has, however, been stable since he reached adulthood and he is keen to have it treated.
Case Study 3
Hori’s macules
A 28-year-old Chinese female presents with speckled dark pigmentation over her malar cheeks (Fig. 10.13A,B). She noticed this only in the last 2 years and worries that it may darken further. She does not use regular sunscreen.
Case Study 4
Becker’s nevus
A 27-year-old male developed a hairy, pigmented area on his left jaw during his teens and presented requesting its removal (Fig. 10.14A,B). It has not changed in size or darkened in recent years, but he is highly troubled by its cosmetic appearance.
Case Study 5
Melanocytic nevi
A 34-year-old Chinese male requested that two moles on his right cheek be removed (Fig. 10.15A,B). He has no family history of any skin malignancies and his moles have not changed for several years. Examination showed a dark-brown junctional nevus and another brown compound nevus on his cheek. During the consultation, the need for multiple treatments and risk of PIH was discussed. It was also explained that there may not be complete clearance and recurrence may occur.
Alam M, Dover JS, Arndt KA. Treatment of facial telangiectasia with variable-pulse high-fluence pulsed-dye laser: comparison of efficacy with fluences immediately above and below the purpura threshold. Dermatologic Surgery. 2003;29:681–685.
Asahina A, Watanabe T, Kishi A, et al. Evaluation of the treatment of port-wine stains with the 595 nm long pulsed dye laser: a large prospective study in adult Japanese patients. Journal of the American Academy of Dermatology. 2006;54:487–493.
Chan HH, Fung WKK, Ying SY, et al. An in vivo trial comparing the use of different types of 532 nm Nd:YAG lasers in the treatment of facial lentigines in Oriental patients. Dermatologic Surgery. 2000;26(8):743–749.
Chan NP, Ho SG, Yeung CK, et al. The use of non-ablative fractional resurfacing in Asian acne scar patients. Lasers in Surgery and Medicine. 2010;42(10):710–715.
Chan NPY, Ho SGY, Shek SYN, et al. A case series of facial depigmentation associated with low fluence Q-switched 1064 nm Nd:YAG laser for skin rejuvenation and melasma. Lasers in Surgery and Medicine. 2010;42(8):712–719.
Cho SB, Park SJ, Kim MJ, et al. Treatment of acquired bilateral nevus of Ota-like macules (Hori’s nevus) using 1064 nm Q-switched Nd:YAG with low fluence. International Journal of Dermatology. 2009;48:1308–1312.
Dufresne RG, Phillips KA, Vittorio CC, et al. A screening questionnaire for body dysmorphic disorder in a cosmetic surgery practice. Dermatologic Surgery. 2001;27:457–462.
Glaich AS, Goldberg LH, Dai T, et al. Fractional resurfacing: a new therapeutic modality for Becker’s nevus. Archives of Dermatology. 2007;143:1488–1490.
Ho SG, Yeung CK, Chan NP, et al. A retrospective analysis of the management of acne post-inflammatory hyperpigmentation using topical treatment, laser treatment, or combination topical and laser treatments in oriental patients. Lasers in Surgery and Medicine. 2011;43(1):1–7.
Ho SGY, Yeung CK, Chan NPY, et al. A comparison of Q-switched and long-pulsed alexandrite laser for the treatment of freckles and lentigines in oriental patients. Lasers in Surgery and Medicine. 2011;43(2):108–113.
Jasim ZF, Woo WK, Handley JM. Long-pulsed (6-ms) pulsed dye laser treatment of rosacea-associated telangiectasia using subpurpuric clinical threshold. Dermatologic Surgery. 2004;30:37–40.
Kagami S, Asahina A, Watanabe R, et al. Treatment of 153 Japanese patients with Q-switched alexandrite laser. Lasers in Medical Science. 2007;22:159–163.
Kawada A, Shiraishi H, Asai M, et al. Clinical improvement of solar lentigines and ephelides with an intense pulsed light source. Dermatol Surg. 2002;28:504–508.
Kono T, Chan HH, Groff WF, et al. Long-pulse pulsed dye laser delivered with compression for treatment of facial lentigines. Dermatologic Surgery. 2007;33:945–950.
Kono T, Nozaki M, Chan HH, et al. A retrospective study looking at the long-term complications of Q-switched ruby laser in the treatment of nevus of Ota. Lasers in Surgery and Medicine. 2001;29:156–159.
Lee HS, Won CH, Lee DH, et al. Treatment of melasma in Asian skin using a fractional 1550 nm laser: an open clinical study. Dermatologic Surgery. 2009;35:1499–1504.
Negishi K, Kushikata N, Tezuka Y, et al. Study of the incidence and nature of ‘very subtle epidermal melasma’ in relation to intense pulsed light treatment. Dermatologic Surgery. 2004;30:881–886.
Negishi K, Tezuka Y, Kushikata N, et al. Photorejuvenation for Asian skin by intense pulse light. Dermatologic Surgery. 2001;27:627–632.
Negishi K, Wakamatsu S, Kushikata N, et al. Full-face photorejuvenation of photodamaged skin by intense pulsed light with integrated contact cooling: initial experiences in Asian patients. Lasers in Surgery and Medicine. 2002;30:298–305.
Polnikorn N. Treatment of refractory melasma with the MedLite C6 Q-switched Nd:YAG laser and alpha arbutin: a prospective study. Cosmetic Laser Therapy. 2010;12:126–131.
Rokhsar CK, Fitzpatrick RE. The treatment of melasma with fractional photothermolysis: a pilot study. Dermatologic Surgery. 2005;31:1645–1650.
Trelles MA, Allones I, Moreno-Arias GA, et al. Becker’s naevus: a comparative study between erbium:YAG and Q-switched neodymium:YAG; clinical and histopathological findings. British Journal of Dermatology. 2005;152:308–313.
Wang CC, Hui CY, Sue YM, et al. Intense pulsed light for the treatment of refractory melasma in Asian patients. Dermatologic Surgery. 2004;30:1196–1200.
Wanitphakdeedecha R, Thanomkitti K, Sethabutra P, et al. A split axilla comparison study of axillary hair removal with low fluence high repetition rate 810 nm diode laser vs. high fluence low repetition rate 1064 nm Nd:YAG laser. Journal of the European Academy of Dermatology and Venereology Sep 19. 2011. Epub ahead of print
Watanabe S, Takahashi H. Treatment of nevus of Ota with the Q-switched ruby laser. New England Journal of Medicine. 1994;331:1745–1750.
Zhou X, Gold MH, Lu Z, et al. Efficacy and safety of Q-switched 1064 nm neodymium-doped yttrium aluminium garnet laser treatment of melasma. Dermatologic Surgery. 2011;37(7):962–970.