7 Laser resurfacing
Summary and Key Features
• Laser resurfacing is a very popular procedure
• A variety of carbon dioxide, Er : YAG and yttrium-scandium-gallium-garnet (YSGG) lasers are included in this category
• Full field means 100% of the treated area is removed to the selected depth
• Fractional means discontinuous portions of the treated area are removed
• Recovery time is linked to amount of damage created
• Fractional treatments have less downtime than full field treatments
• Experience with these lasers is important to outcomes
• Post-treatment care is very important
• Complications can arise with all of these laser treatments
Introduction
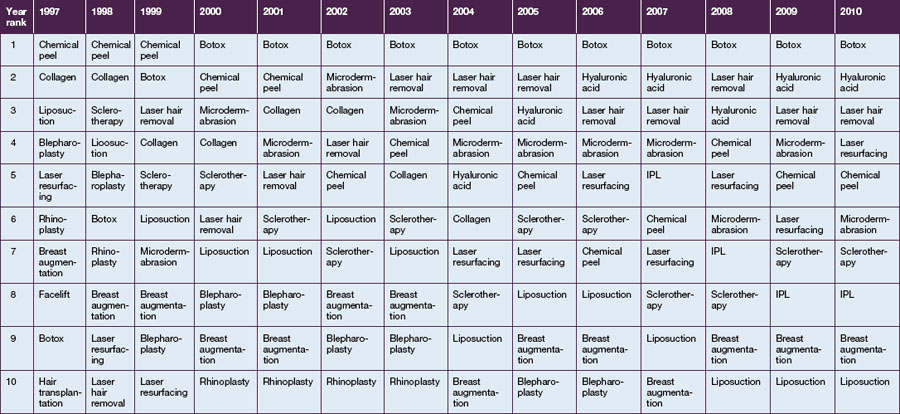
Laser resurfacing is a very popular procedure in the United States and worldwide. Data from The American Society of Aesthetic Plastic Surgery collected yearly from core specialists since 1997 through 2010 has shown the rise, fall, and rise again of this procedure as devices have been introduced (Table 7.1). In the mid 1990s carbon dioxide lasers were extremely popular, but toward the turn of the century they fell out of favor and were somewhat replaced by non-ablative technology. Laser resurfacing resurged in the last 5 years with the introduction of fractional lasers.
History
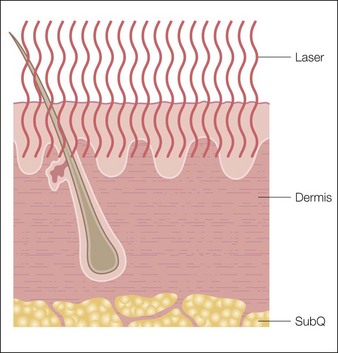
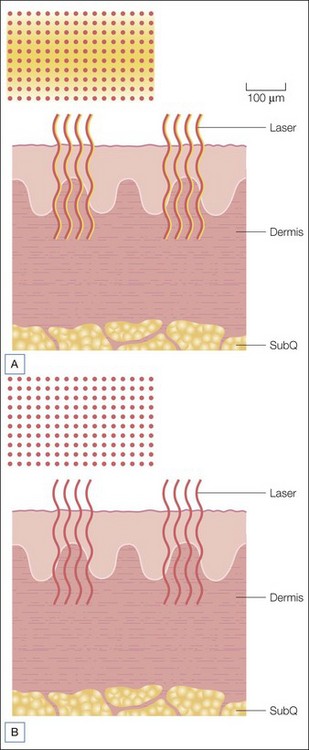
In 2004 Manstein et al introduced the concept of fractional photothermolysis. Full field or traditional laser resurfacing as described above removes the entire skin surface in the area being treated with depth of injury depending upon energy level, whereas fractional laser resurfacing treats a small ‘fraction’ of the skin at each session, leaving skip areas between each exposed area (Fig. 7.1). This was first performed commercially using non-ablative fluences at 1550 nm (Solta Medical, Mountain View, CA). These non-ablative fractional lasers created a column of thermal damage with intact epidermis. Healing occurred from deeper structures as well as from adjacent structures. This differs from full field resurfacing in which healing occurred from only deeper structures. Deeper treatments (i.e. to the reticular dermis) can safely be performed using this approach than would be tolerated using a full field treatment. Advantages of this approach include avoidance of an open wound and very low risk of pigment disturbance or scarring. Disadvantages have included the need for multiple treatments and somewhat less clinical response than with full field ablative resurfacing. Since the introduction of the original system there have been many manufacturers that have introduced similar non-ablative fractional devices with wavelengths of 1440 nm, 1540 nm, and 1550 nm. These devices differ in power output, spot size, density, etc. and comparisons of clinical efficacy are difficult, yet similar degrees of tissue injury should produce similar clinical results.
Fractional ablative resurfacing with carbon dioxide, erbium, and yttrium-scandium-gallium-garnet (YSGG) systems was introduced with the intent of providing more significant results than non-ablative fractional systems while achieving shorter healing times and complications when compared with full field ablative systems (Fig. 7.2). These devices differ not only in wavelength but in system power, spot size, and amount of thermal damage created adjacent to and deep to the ablated hole. One popular erbium system, the Sciton ProFractional®, allows one to vary the amount of thermal damage similarly to their full field system. Other newer carbon dioxide fractional lasers allow variation of the thermal damage zones (Deka Medical) while others allow superficial and deeper penetration with a single scan (Syneron, Yokneum, Israel). As with the non-ablative fractional systems, direct comparison between devices is difficult as devices differ in power output, spot size, density, and degree of thermal damage, but similar degrees of injury should produce similar clinical results.
Expected benefits and alternatives
Lasers and technical overview
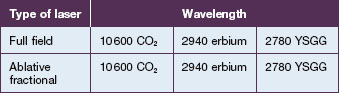
As discussed above, current devices used for ablative laser resurfacing include carbon dioxide, Er : YAG, and YSGG lasers, in both full field and fractional modes, and non-ablative devices in a variety of wavelengths including 1440 nm, 1540 nm, 1550 nm, and 1927 nm (Table 7.2). Some machines offer upgradeable expandable platforms where full field devices and fractional devices are available in one machine whereas other companies offer only isolated full field or fractional devices.
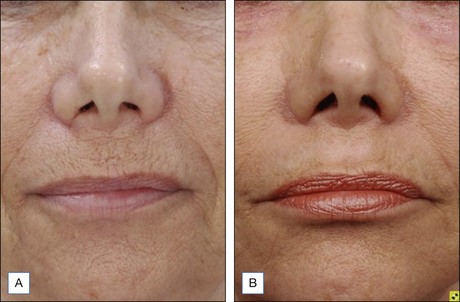
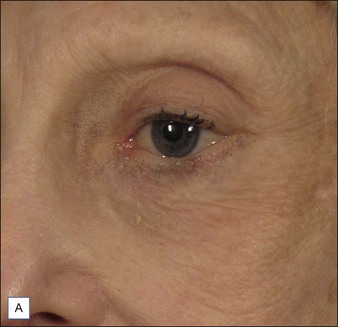
Er : YAG full field
The erbium : YAG laser (2940 nm) has an absorption coefficient 10 times greater than the carbon dioxide laser and ablates tissue more efficiently and leaves less residual thermal damage (5–10 µm). There is a linear relationship between energy density (fluence) delivered and tissue ablated with 3–4 µm of tissue removed per J/cm2 and multiple passes can be used to produce deeper tissue removal without additive residual thermal injury. This leads to recovery time of deep full field Er : YAG laser resurfacing of 7 days to full epithelialization followed by 3–6 weeks of erythema. Superficial and deep resurfacing can be performed with these devices with increasing results and increasing recovery times with deeper treatments (Figs 7.3 and 7.4). Complications including hypopigmentation were less than with carbon dioxide laser full field resurfacing.
Non-ablative fractional
As previously mentioned, non-ablative fractional resurfacing involves the simultaneous or sequential placement of multiple small spots of laser light onto the surface of the skin with intervening skip areas of unexposed skin. The chromophore used is water and the wavelengths used are 1440, 1470, 1550, and 1540 nm. The lasers create a column of tissue coagulation from 300 to 1200 µm and are called microthermal zones (MTZ). This subject is covered in Chapter 6 and readers are referred there for a more extensive discussion.
Fractional ablative technology
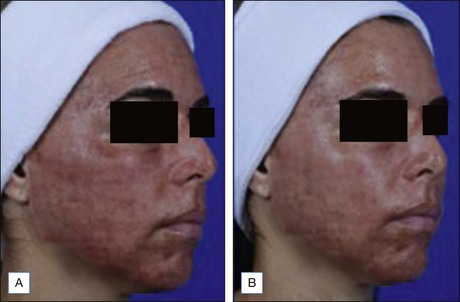
Both ablative fractional and non-ablative fractional devices are used to treat acne and other scars. Multiple treatments are needed and there is no current consensus as to the best technology for this at present. It is very common in our offices to perform combination treatment with superficial full field Er : YAG resurfacing followed by Er : YAG fractional treatment. The superficial Er : YAG treatment improves skin texture and minor irregularities while the fractional treatment is useful for collagen remodeling (Figs 7.5, 7.6).

Figure 7.6 (A, B) This patient had scars of the forehead treated with ablative fractional resurfacing.
As fractional CO2 treatments have been pushed to higher and higher coverages in an attempt to maximize efficacy, healing times predictably have increased. More importantly, complications such as scarring and hypopigmentation have been observed at coverages in excess of 45%. CO2 resurfacing histology consistently shows a significant component of tissue ablation and coagulation. Efficacious resurfacing is believed to require a significant component of both. One strategy that has been explored to increase coverage percentage and maximize efficacy involves a combination treatment with ablative Er : YAG fractional and non-ablative fractional exposures in a single treatment session. This provides a component of largely ablative exposure with the fractional Er : YAG treatment and a component of coagulation with the non-ablative fractional treatment. Rather than being spatially overlapped as in a fractional CO2 microthermal zone, the coagulation and ablation are separated. Coverages up to 65% are routinely applied with only a modest increase in healing time and erythema compared with fractional Er : YAG treatment alone and somewhat less than that reported for fractional CO2. Advantages of this approach include preservation of the short recovery and low incidence of complications seen with fractional Er : YAG treatments and the potential for significant improvement even in perioral rhytides. Disadvantages include the need for two lasers or a single laser platform that offers both options and the time-consuming nature of the treatments (Fig. 7.7).
Overview of treatment strategy
Treatment approach
There are a few absolute contraindications for laser treatment and some areas of caution.
Relative contraindications
Pre- and post-treatment regimens
Use of sunblock is mandatory for all laser-resurfacing patients after epithelialization is complete. We also recommend institution of a skin care regimen after epithelialization is complete and the skin has had a chance to ‘calm down’. This may mean a few days for fractional treatments to a few weeks for full field treatments. There are many good skin care regimens appropriate after laser resurfacing. The combination of 4% hydroquinone and low-strength Retin-A® (tretinoin) is still used, although newer regimens with added growth factors are favored by some. The key is to start these regimens slowly to avoid irritation of the skin (see below – dermatitis).
Complications and their treatment
Infection
Infection after laser resurfacing can be viral, bacterial, or fungal. The most well-known complication is due to herpes simplex virus. Many patients have been infected previously and so are carriers. The current recommendation as outlined above is for all patients to be prophylaxed against herpes viral infections. Some patients may avoid taking the anti-viral medications whereas others may experience breakthrough infection (Fig. 7.8). The treatment is early recognition of the infection and treatment with oral antiviral agents. For very severe infections with herpes simplex or zoster intravenous anti-viral medication may be needed.
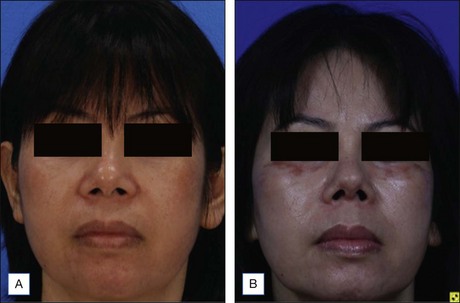
True fungal infection is rare, but infection with yeast (Candida albicans) is common (Fig. 7.9). The patient usually presents with an extremely red face with a history of having improvement in the healing and suddenly appearing much redder. Treatment is topical anti-fungal therapy with or without an oral antifungal medication such as fluconazole.
Hypopigmentation
This is a dreaded complication of deep laser resurfacing and has been reported both with carbon dioxide and Er : YAG treatments and with full field and fractional treatments. It is not uncommon with deep carbon dioxide resurfacing, with some series reporting up to 70% of patients getting hypopigmentation. It is rare with deep Er : YAG full field resurfacing and very rare with all fractional treatments. There are not many effective treatments, but some have reported improvement with excimer laser therapy. Blending of the noticeable line of demarcation is often helpful (Fig. 7.10).
Hyperpigmentation
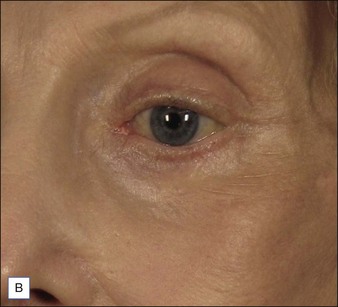
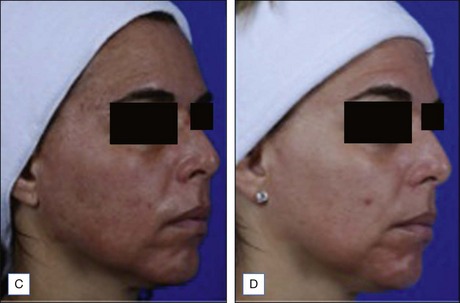
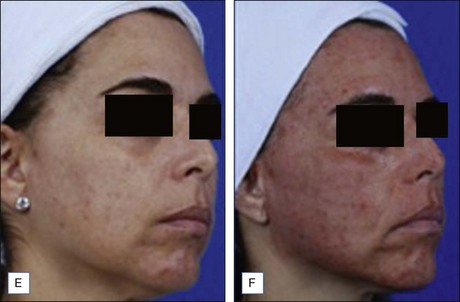
Postinflammatory pigmentation (PIH) is a very common problem following laser resurfacing. It is more common in darker skin types and in patients who have had early sun exposure (Fig. 7.11). Prevention as outlined above is key. Treatment is with topical bleaching creams, often combined with retinoids. Failures of this regimen are usually treated with IPL.
Scarring
Scarring after laser resurfacing may occur owing to overly aggressive full field or fractional treatment, infection, or even scratching by the patient. Full field resurfacing is a controlled first-degree or second-degree burn and anything such as infection may convert that controlled second-degree burn into a third-degree burn with resultant scarring. Overaggressive fractional resurfacing may be due to too deep a treatment, or too much density, creating a full field defect when a fractional treatment was intended. We prefer early treatment of thickened areas that appear to be heading towards scarring with potent topical corticosteroids such as a pulsed regimen with clobetasol. Intralesional corticosteroids, intralesional 5-FU, vascular laser or IPL treatment, and fractional lasers have all been used to improve hypertropic scars after laser resurfacing (Fig. 7.12).
Bass LS. Erbium : YAG laser skin resurfacing: Preliminary clinical evaluation. Annals of Plastic Surgery. 1998;40:328–334.
Bass LS, DelGuzzo M, Doherty S, et al. Combined ablative and non-ablative fractional treatment for facial skin rejuvenation. Lasers in Surgery and Medicine. 2009;15(suppl):29.
Bogle MA, Arndt KA, Dover JS. Evaluation of plasma skin regeneration technology in low fluence full-facial rejuvenation. Archives of Dermatology. 2007;143:168–174.
Chan H. Effective and safe use of lasers, light sources, and radiofrequency devices in the clinical management of Asian patients with selected dermatoses. Lasers in Surgery and Medicine. 2005;37:179–185.
Clementoni MT, Gilardino P, Muti GF, et al. Non-sequential fractional ultrapulsed CO2 resurfacing of photoaged facial skin: Preliminary clinical report. Journal of Cosmetic and Laser Therapy. 2007;9:218–225.
Fitzpatrick RE, Rostan EF, Marchell N. Collagen tightening induced by carbon dioxide laser versus erbium : YAG laser. Lasers in Surgery and Medicine. 2000;27:395–403.
Fisher GH, Geronemus RG. Short-term side effects of fractional photothermolysis. Dermatologic Surgery. 2005;31:1245–1249.
Friedman PM, Glaich A, Rahman Z, et al. Fractional photothermolysis for the treatment of hypopigmented scars. American Society for Dermatologic Surgery Annual Meeting Presentation. 2006. October 2006
Geronemus RG. Fractional photothermolysis: Current and future applications. Lasers in Surgery and Medicine. 2006;38:169–176.
Kilmer S, Fitzpatrick R, Bernstein E, et al. Long term follow-up on the use of plasma skin regeneration (PSR) in full facial rejuvenation procedures. Lasers in Surgery and Medicine. 2005;36:22.
Kim KH, Fisher GH, Bernstein LJ, et al. Treatment of acneiform scars with fractional photothermolysis. Lasers in Surgery and Medicine. 2005;36:31.
Langlois JH, Kalakanis L, Rubenstein AT, et al. Maxims or myths of beauty? A meta-analytic and theoretical review. Psychological Bulletin. 2000;126:390–423.
Laubach H, Tannous Z, Anderson RR, et al. A histological evaluation of the dermal effects after fractional photothermolysis treatment. Lasers in Surgery and Medicine. 2005;26:86.
Manstein D, Herron GS, Sink RK, et al. Fractional photothermolysis: a new concept for cutaneous remodeling using microscopic patterns of thermal injury. Lasers in Surgery and Medicine. 2004;34:426–438.
Morrow PC, McElroy JC, Stamper BG, et al. The effects of physical attractiveness and other demographic characteristics on promotion decisions. Journal of Management. 1990;16:723–736.
Pozner JN, Goldberg DJ. Superficial erbium : YAG laser resurfacing of photodamaged skin. Journal of Cosmetic Laser Therapy. 2006;8(2):89–91.
Pozner JN, Goldberg DJ. Histologic effect of a variable pulsed Er : YAG laser. Dermatologic Surgery. 2000;26:733–776.
Pozner JN, Roberts TL. Variable-pulse width Er : YAG laser resurfacing. Clinics in Plastic Surgery. 2000;27:2. 263
Rahman Z, Rokhsar CK, Tse Y, et al. The treatment of photodamage and facial rhytides with fractional photothermolysis. Lasers in Surgery and Medicine. 2005;36:32.
Rahman Z, Alam M, Dover JS. Fractional laser treatment for pigmentation and texture improvement. Skin Therapy Letters. 2006;11:7–11.
Tannous ZS, Astner S. Utilizing fractional resurfacing in the treatment of therapy-resistant melasma. Journal of Cosmetic Laser Therapy. 2005;7:39–43.
Tannous Z, Laubach HJ, Anderson RR, et al. Changes of epidermal pigment distribution after fractional resurfacing: a clinicopathologic correlation. Lasers in Surgery and Medicine. 2005;36:32.
Tanzi EL, Alster TS. Fractional photothermolysis: Treatment of non-facial photodamage with a 1550 nm erbium-doped fiber laser. Lasers in Surgery and Medicine. 2005;36:31.
Weinstein C, Ramirez OM, Pozner JN. Postoperative care following CO2 laser resurfacing: Avoiding Pitfalls. Plastic and Reconstructive Surgery. 1997;100:1855–1866.
Weinstein CW, Ramirez OM, Pozner JN. Carbon dioxide laser resurfacing complications and their prevention. Aesthetic Surgery Journal. 1997;17:216–225.
Weiss RA, Gold M, Bene N, et al. Prospective clinical evaluation of 1440-nm laser delivered by microarray for the treatment of photoaging and scars. Journal of Drugs in Dermatology. 2006;5:740–744.