4 Laser hair removal
Summary and Key Features
• Laser hair removal is the most commonly requested cosmetic procedure in the world
• The extended theory of selective photothermolysis enables the laser surgeon to target and destroy hair follicles, thereby leading to both permanent and temporary hair removal
• The ideal candidate for laser hair removal (LHR) is fair skinned with dark terminal hair; however, LHR can today be successfully performed in all skin types
• Thin hairs and hairs with white, blond and red color are extremely difficult to treat with laser hair removal devices
• Wax epilation should be avoided prior to laser hair removal treatments
• Lasers pose a safety risk to both the patient and device operator
• Informed consent should be reviewed with every patient prior to treatment
• Wavelengths, spot size, pulse duration, and skin cooling are key variables that can be used to tailor laser–tissue interactions for a given patient
• Roughly 15–30% of hairs can be removed with each treatment session using ideal parameters. Remaining hairs are often thinner and lighter in color
• The most common complication is pigmentary alteration, which can be temporary or permanent
Basic hair biology
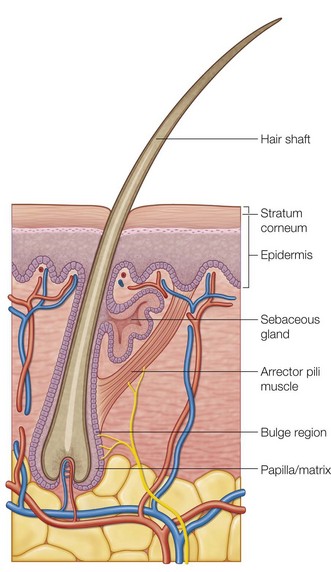
The hair follicle is a hormonally active structure (Fig. 4.1) that is anatomically divided into an infundibulum (hair follicle orifice to insertion of the sebaceous gland), isthmus (insertion of the sebaceous gland to the insertion of the arrector (erector) pili muscle), and inferior (insertion of the arrector pili to the base of the hair follicle) segments. The dermal papilla provides neurovascular support to the base of the follicle and helps form the hair shaft.
Mechanism of LHR
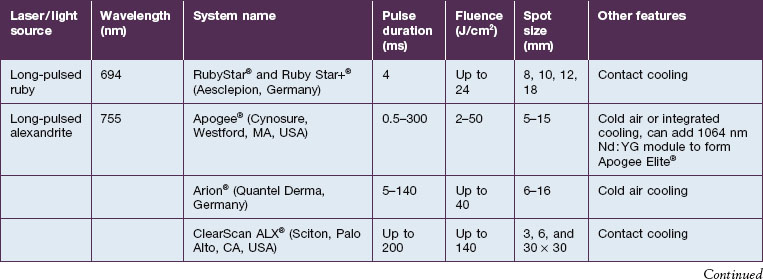
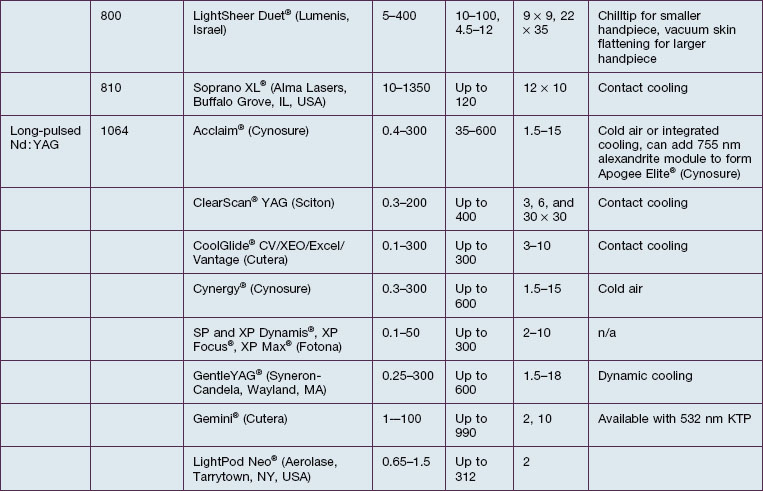
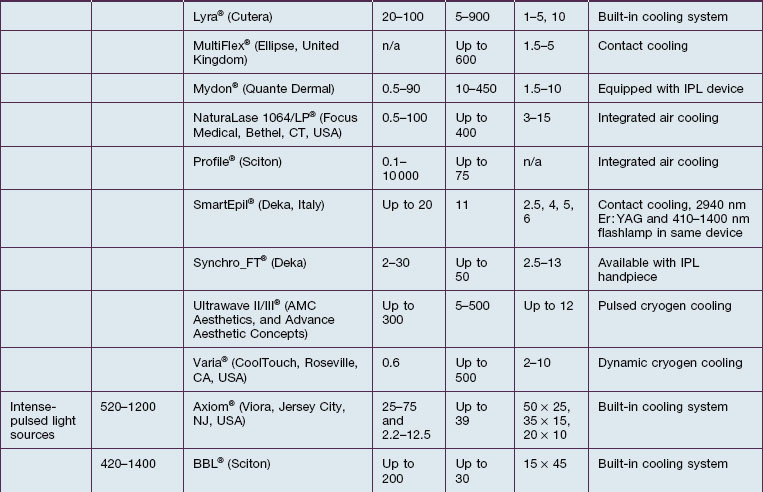
The theory of selective photothermolysis enables precise targeting of pigmented hair follicles by using the melanin of the hair shaft as a chromophore. Melanin has an absorbance spectrum that matches wavelengths in the red and near-infrared (IR) portion of the electromagnetic spectrum. To achieve permanent hair removal, the biological ‘target’ is the follicular stem cells located in the bulge region and / or dermal papilla. Due to the slight spatial separation of the chromophore and desired target, an extended theory of selective photothermolysis was proposed that requires diffusion of heat from the chromophore to the desired target for destruction. This requires a laser pulse duration that is longer in duration than if the actual chromophore and desired target are identical. Temporary LHR can result when the follicular stem cells are not completely destroyed, primarily through induction of a catagen-like state in pigmented hair follicles. Temporary LHR is much easier to achieve than permanent removal when using lower fluences. Long-term hair removal depends on hair color, skin color, and tolerated fluence. Roughly 15–30% long-term hair loss may be observed with each treatment when optimal treatment parameters are used (Fig. 4.2). A list of laser and light devices that are currently commercially available for hair removal is given in Table 4.1.
Key factors in optimizing treatment
Patient selection
A focused medical history, physical examination, and informed consent, including setting realistic expectations and potentials risks, should be performed prior to any laser treatment (Box 4.1). Patients with evidence of endocrine or menstrual dysfunction should be appropriately worked up. Similarly, patients with an explosive onset of hypertrichosis should be evaluated for paraneoplastic etiologies. Treatment of a pregnant woman for non-urgent conditions is discouraged by the authors, although there is no evidence suggesting a potential risk to pregnant women undergoing LHR. The past medical history should be reviewed to identify patients with photosensitive conditions, such as autoimmune connective tissue disorders, or disorders prone to the Koebner phenomenon. A history of recurrent cutaneous infections at or in the vicinity of the treatment area might warrant the use of prophylactic medications. Any past history of keloid or hypertrophic scar formation should be elicited as well. Previous hair removal methods, including past laser treatments, should be reviewed. Any methods of hair shaft epilation (e.g. waxing or tweezing) that entirely remove the target chromophore render LHR less effective for at least 2 weeks. Although there is little evidence for the time frame a patient must wait after complete epilation of the hair shaft and laser treatment, we recommend a minimum of 6 weeks. Shaving and depilatory creams can be used up to the day of laser treatment as they do not remove the entire hair shaft.
Box 4.1
Pertinent medical history for laser / pulsed light hair removal
 Presence of conditions that may cause hypertrichosis:
Presence of conditions that may cause hypertrichosis:
 Drugs (i.e. corticosteroids, hormones, immunosuppressives, self or spousal use of minoxidil)
Drugs (i.e. corticosteroids, hormones, immunosuppressives, self or spousal use of minoxidil)
 History of local or recurrent skin infection
History of local or recurrent skin infection
 History of herpes simplex, especially perioral
History of herpes simplex, especially perioral
 History of herpes genitalis, important when treating the pubic or bikini area
History of herpes genitalis, important when treating the pubic or bikini area
 History of keloids / hypertrophic scarring
History of keloids / hypertrophic scarring
 History of koebnerizing skin disorders such as vitiligo and psoriasis
History of koebnerizing skin disorders such as vitiligo and psoriasis
 Previous treatment modalities – method, frequency, and date of last treatment, as well as response
Previous treatment modalities – method, frequency, and date of last treatment, as well as response
 Recent suntan or exposure to tanning or light cabinet
Recent suntan or exposure to tanning or light cabinet
 Onset of hair regrowth (recent)
Onset of hair regrowth (recent)
 Patient’s hobbies or habits which might interfere with treatment
Patient’s hobbies or habits which might interfere with treatment
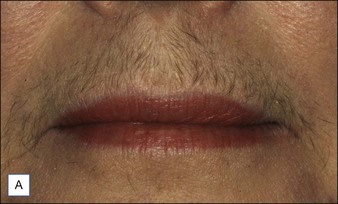
The physical exam should corroborate the patient’s Fitzpatrick skin phototype. This will help determine which lasers and light sources are safe to use for that patient (see Table 4.1) because epidermal melanin in darkly pigmented patients competes with the melanin within hair follicles as a chromophore. Importantly, every patient should always be evaluated for the presence of a tan and, if present, laser treatment should be delayed or the treatment parameters appropriately adjusted until the tan has faded. Finally, the patient’s hair color should be noted as the chromophore for LHR is melanin. Black and brown terminal hairs typically contain sufficient amount of melanin to serve as a chromophore for LHR. In contrast the lack of melanin, paucity of melanin or presence of eumelanin in the hair follicle, which clinically correlates with white, gray, or red / blonde hair respectively, is predictive of a poor response to laser hair removal (Fig. 4.3). For patients with little to no melanin in their hair follicles, attempts have been made to use exogenous chromophores that can be topically delivered to the hair follicles, thereby making the removal of white, gray, red, and blonde hair hypothetically possible. This concept was first demonstrated with a topical carbon solution dissolved in mineral oil. However, we have noticed very little long-term hair reduction efficacy of topical chromophores in our experience. The coarseness and density of hair are also important to note as these factors will influence parameter settings (see below).
Device variables
Wavelength
The long-pulsed ruby laser (694 nm) was the first device used to selectively target hair follicles, resulting in long-term hair loss. The long-pulsed ruby laser can be safely used in Fitzpatrick skin phototypes I–III. Table 4.1 lists the long-pulsed ruby lasers that are commercially available.
The long-pulsed alexandrite (755 nm) laser has been shown to be effective for long-term hair removal in multiple studies. The long-pulsed alexandrite laser can be safely used in Fitzpatrick skin phototypes I–IV, although some experts limit the use of the long-pulsed alexandrite laser to Fitzpatrick skin phototypes I–III. A few studies have demonstrated the safety of the long-pulsed alexandrite laser in a large cohort of patients with Fitzpatrick skin phototypes IV–VI. Combination treatment of alexandrite and Nd : YAG lasers provides no added benefit over the alexandrite laser alone. The commercially available long-pulsed alexandrite devices are summarized in Table 4.1.
Fluence
Fluence is defined as the amount of energy delivered per unit area and is expressed as J/cm2. Higher fluences have been correlated with greater permanent hair removal, but are also more likely to cause untoward side effects. Recommended treatment fluences are often provided with each individual laser device for non-experienced operators. However, a more appropriate method of determining the optimal treatment fluence for a given patient is to evaluate for the desired clinical end point of perifollicular erythema and edema seen within a few minutes of treatment (Fig. 4.4). The highest possible tolerated fluence that yields this end point without any adverse effects is the best fluence for treatment. Fluences that cause epidermal disruption are too high and should be reduced.
Skin cooling
The presence of epidermal melanin, particularly in darker skin types, presents a competing chromophore to hair follicle melanin, which can be damaged during LHR (Fig. 4.5). Cooling of the skin surface is used to minimize epidermal damage as well as pain, while permitting treatment with higher fluences. All of the skin-cooling methods function by acting as a heat sink and removing heat from the skin surface. The least effective type of cooling is the use of an aqueous cold gel, which passively extracts heats from the skin and then is not capable of further skin cooling. Alternatively, cooling with forced chilled air can provide cooling to the skin before, during, and after a laser pulse. Currently, most of the available LHR devices have a built-in skin cooling system, which consists of either contact cooling or dynamic cooling with a cryogen spray. Contact cooling, usually with a sapphire tip, provides skin cooling just before and during a laser pulse. It is most useful for treatments with longer pulse durations (>10 ms). Dynamic cooling with cryogen liquid spray pre-cools the skin with a millisecond spray of cryogen just before the laser pulse. A second spray can be delivered just after the laser pulse for post-cooling, but parallel cooling during the laser pulse is not possible as the cryogen spray interferes with the laser beam. Dynamic cooling is best suited for use with pulse durations shorter than 5 ms.
Complications
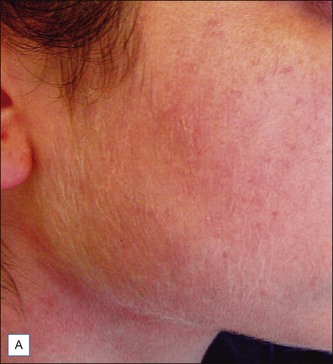
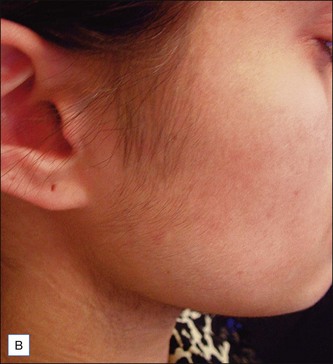
The most common complications of LHR are epidermal damage (Fig. 4.6) and pigmentary alterations, including hyper- and hypopigmentation (Fig. 4.7). This may result from selecting a non-optimal wavelength, pulse duration or fluence, using inadequate epidermal cooling or treating a tanned patient (Fig. 4.8). Pigmentary alterations may also occur even when optimal treatment parameters are used. These changes are often transient and improve with time, although permanent hypopigmentation can occur (Fig. 4.7B). Zones of untreated hairs can result from a lack of overlapping between laser pulses (Fig. 4.9). Scarring is an exceedingly rare complication but can occur when excessive fluences and / or pulse stacking are used.


Figure 4.7 Example of laser hair removal induced hyperpigmentation (A) and permanent hypopigmentation (B).
Treatment of the lateral cheeks and chin area, or less commonly other areas, may result in the induction of terminal hairs, a phenomenon known as paradoxical hypertrichosis (Fig. 4.10). This has been reported to occur more commonly in females of Mediterranean, Middle Eastern, Asian and South Asian descent. The exact mechanism remains uncharacterized but it is thought that subtherapeutic laser fluences may lead to the stimulation of hair growth.
Caution should be exercised to avoid treatment of tattoos and nevi, particularly atypical nevi.
Conclusion
Future directions
Advances in pain control
A novel technique to reduce LHR-associated pain is pneumatic skin flattening (PSF). PSF works by coupling a vacuum chamber to generate negative pressure and to flatten the skin against the hand piece treatment window. Based on the gate theory of pain transmission, it stimulates pressure receptors in the skin immediately prior to firing of the laser pulse, thereby blocking activation of pain fibers. PSF is just beginning to be incorporated into commercially available lasers (see Table 4.1). A recent study of LHR using a LPDL with a large spot size and vacuum-assisted suction showed that the majority of subjects reported feeling no pain at all or up to moderate pain without the use of skin cooling or topical anesthetics. Notably, none of the subjects in the study reported experiencing severe or intolerable pain.
Alternative technologies for hair removal
Electro-optical synergy (ELOS) technology combines electrical (conducted radiofrequency) and optical (laser / light) energies. A handful of devices based on this technology have been produced (see Table 4.1). The theory behind ELOS is based on the optical component (laser or IPL) heating the hair shaft, which then is thought to concentrate the bipolar radiofrequency (RF) energy to the surrounding hair follicle. Based on this combination, lower fluences are needed for the optical component, thereby suggesting it might be well tolerated in all Fitzpatrick skin phototypes, and potentially effective in the removal of white and poorly pigmented hair. A study of 40 patients (Fitzpatrick skin phenotypes II–V) with varied facial and non-facial hair colors were treated with combined IPL / RF ELOS technology. An average clearance of 75% was observed at 18 months following four treatments. No significant adverse sequelae were noted and there were no treatment differences between patients of varying skin types or hair color. Pre-treatment with aminolevulinic acid (ALA) prior to use of a combined IPL and radiofrequency device has been shown to further augment the removal of terminal white hairs.
Alster TS, Bryan H, Williams CM. Long-pulsed Nd : YAG laser-assisted hair removal in pigmented skin: a clinical and histological evaluation. Archives of Dermatology. 2001;137(7):885–889.
Altshuler GB, Anderson RR, Manstein D, et al. Extended theory of selective photothermolysis. Lasers in Surgery and Medicine. 2001;29(5):416–432.
Anderson RR, Parrish JA. Selective photothermolysis: precise microsurgery by selective absorption of pulsed radiation. Science. 1983;220(4596):524–527.
Bernstein EF. Hair growth induced by diode laser treatment. Dermatologic Surgery. 2005;31(5):584–586.
Braun M. Comparison of high-fluence, single-pass diode laser to low-fluence, multiple-pass diode laser for laser hair reduction with 18 months of follow up. Journal of Drugs in Dermatology. 2011;10(1):62–65.
Campos VB, Dierickx CC, Farinelli WA, et al. Hair removal with an 800-nm pulsed diode laser. Journal of the American Academy of Dermatology. 2000;43(3):442–447.
Davoudi SM, Behnia F, Gorouhi F, et al. Comparison of long-pulsed alexandrite and Nd:YAG lasers, individually and in combination, for leg hair reduction: an assessor-blinded, randomized trial with 18 months of follow-up. Archives of Dermatology. 2008;144(10):1323–1327.
Dierickx CC, Grossman MC, Farinelli WA, et al. Permanent hair removal by normal-mode ruby laser. Archives of Dermatology. 1998;134(7):837–842.
Eremia S, Li C, Newman N. Laser hair removal with alexandrite versus diode laser using four treatment sessions: 1-year results. Dermatologic Surgery. 2001;27(11):925–929. discussion 929-930
Garcia C, Alamoudi H, Nakib M, et al. Alexandrite laser hair removal is safe for Fitzpatrick skin types IV–VI. Dermatologic Surgery. 2000;26(2):130–134.
Gold MH, Bell MW, Foster TD, et al. One-year follow-up using an intense pulsed light source for long-term hair removal. Journal of Cutaneous Laser Therapy. 1999;1(3):167–171.
Goldberg DJ, Littler CM, Wheeland RG. Topical suspension-assisted Q-switched Nd : YAG laser hair removal. Dermatologic Surgery. 1997;23(9):741–745.
Grossman MC, Dierickx C, Farinelli W, et al. Damage to hair follicles by normal-mode ruby laser pulses. Journal of the American Academy of Dermatology. 1996;35(6):889–894.
Haak CS, Nymann P, Pedersen AT, et al. Hair removal in hirsute women with normal testosterone levels: a randomized controlled trial of long-pulsed diode laser vs. intense pulsed light. British Journal of Dermatology. 2010;163(5):1007–1013.
Hussain M, Polnikorn N, Goldberg DJ. Laser-assisted hair removal in Asian skin: efficacy, complications, and the effect of single versus multiple treatments. Dermatologic Surgery. 2003;29(3):249–254.
Ibrahimi OA, Avram MM, Hanke CW, et al. Laser hair removal. Dermatologic Therapy. 2011;24(1):94–107.
Ibrahimi OA, Kilmer SL. Long-term clinical evaluation of a 800 nm long-pulsed diode laser with a large spot size and vacuum-assisted suction for hair removal. Dermatologic Surgery. 2012;38(6):912–917.
Khoury JG, Saluja R, Goldman MP. Comparative evaluation of long-pulse alexandrite and long-pulse Nd : YAG laser systems used individually and in combination for axillary hair removal. Dermatologic Surgery. 2008;34(5):665–670. discussion 670-661
Lask G, Friedman D, Elman M, et al. Pneumatic skin flattening (PSF): a novel technology for marked pain reduction in hair removal with high energy density lasers and IPLs. Journal of Cosmetic and Laser Therapy. 2006;8(2):76–81.
Lou WW, Quintana AT, Geronemus RG, et al. Prospective study of hair reduction by diode laser (800 nm) with long-term follow-up. Dermatologic Surgery. 2000;26(5):428–432.
Nouri K, Chen H, Saghari S, et al. Comparing 18- versus 12-mm spot size in hair removal using a gentlease 755-nm alexandrite laser. Dermatologic Surgery. 2004;30(4 Pt 1):494–497.
Rao J, Goldman MP. Prospective, comparative evaluation of three laser systems used individually and in combination for axillary hair removal. Dermatologic Surgery. 2005;31(12):1671–1676. discussion 1677
Richards RN, Meharg GE. Electrolysis: observations from 13 years and 140,000 hours of experience. Journal of the American Academy of Dermatology. 1885;33(4):662–666.
Rohrer TE, Chatrath V, Yamauchi P, et al. Can patients treat themselves with a small novel light based hair removal system? Lasers in Surgery and Medicine. 2003;33(1):25–29.
Zenzie HH, Altshuler GB, Smirnov MZ, et al. Evaluation of cooling methods for laser dermatology. Lasers in Surgery and Medicine. 2000;26(2):130–144.