Laser Excision and Vaporization
Although carbon dioxide (CO2) laser vaporization of vulvar intraepithelial neoplasia is an effective, quick, and cost-efficient method of treatment, it does present a significant disadvantage: No tissue specimen is available for histologic examination when tissue is ablated; therefore, no information relative to margins or the severity of the disease can be obtained. For obtaining a tissue specimen, laser excision is preferable to ablative techniques.
Laser Excision by Thin Section
The laser “thin section” has three advantages: It (1) requires neither closure nor grafting, (2) heals rapidly without gross scar formation, and (3) provides a specimen for pathologic examination.
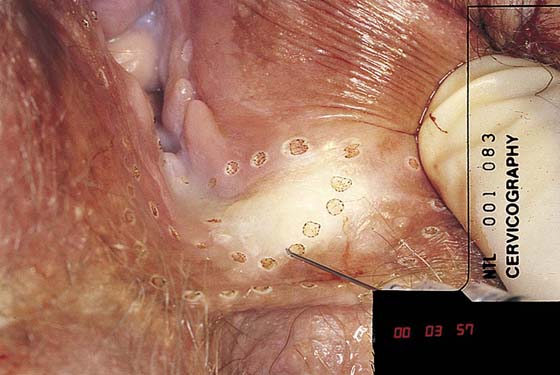
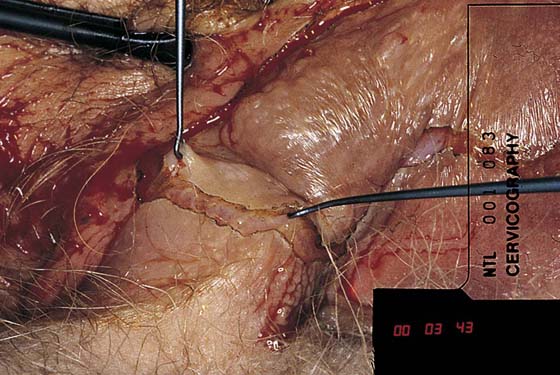
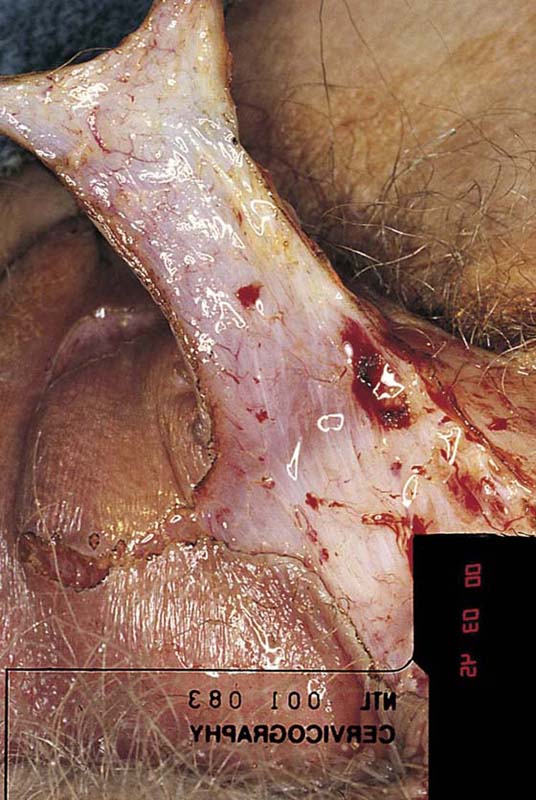
The lesion should be mapped preoperatively. The patient is positioned and prepared as for a knife resection (Fig. 69–1). A superpulsed (UltraPulse) CO2 laser coupled to a micromanipulator is the instrument of choice. The area for resection is outlined with laser spots (Fig. 69–2). The laser power is set at 8 to 12 W, and a tracer cut is made around the lesion. Next, a 1 : 100 vasopressin solution is injected subdermally, completely circumscribing the lesion and infiltrating beneath the skin (Fig. 69–3). Next, laser power is increased to 15 to 20 W, and, with a tightly focused beam, a plane is created parallel to the surface of the skin. The cut is made beneath the papillary dermis into the reticular dermis (Fig. 69–4). Maintenance of the plane and the excision is facilitated by keeping constant tension on the skin that is to be excised (Fig. 69–5). Small bleeding vessels are directly sutured with 4-0 or 5-0 Vicryl (Fig. 69–6). Application of clamps is avoided to diminish trauma to the tissue.
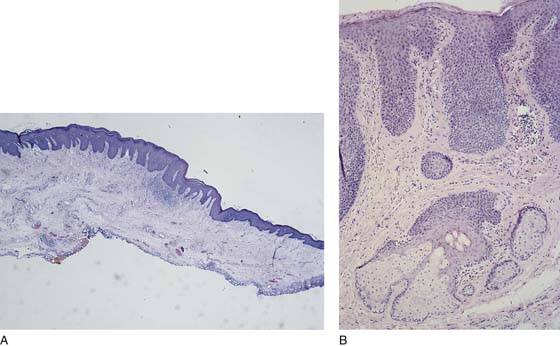
The excised specimen is placed in fixative and sent to pathology (Figs. 69–7 and 69–8A, B). Postoperatively, the patient is instructed to take tub baths in salt water (Instant Ocean) twice daily and to apply silver sulfadiazine (Silvadene) cream to the wound site 3 times per day. Alternatively, a urethane dressing (OpSite) is applied to the wound (Fig. 69–9A, B). Healing is complete at 4 to 6 weeks (Fig. 69–10A, B).
Laser Vaporization
CO2 laser vaporization is performed by using specifications identical to those used for excision (i.e., vaporization in hair-bearing areas, perineum, and perianal skin to a depth of 2.3 mm with a 3-mm peripheral margin) (Figs. 69–11 through 69–16). For the labia minora, periclitoral lesion vaporization is carried to a depth no greater than 1 mm; again, wide peripheral margins are recommended to diminish the chance of recurrence (Figs. 69–17 and 69–18). Preoperative mapping with extensive preoperative tissue sampling is a requirement before any laser vaporization to (1) determine that the disease is not invasive carcinoma, and (2) predict the extent of the disease and the peripheral margins for vaporization. The medial and lateral margins of the neoplasia are outlined after the patient has been anesthetized, prepared, and draped (Figs. 69–19 and 69–20). Power is set at 20 W, and the beam is defocused to permit a 2-mm-diameter spot (Figs. 69–21 and 69–22). The laser places multiple impact spots, much in the manner of marking the lesion with a pen. The spots are then connected, producing a clear outline of the area to be vaporized (Figs. 69–23 and 69–24). Laser power is turned up to 30 to 40 W, and the entire zone is vaporized to a uniform 2-mm depth (note that vaporization between 0.5 and 1.5 mm is accounted for by thermal conduction injury) (Figs. 69–25 through 69–27). When the vaporization is complete, any char is washed away. The wound is covered with Silvadene cream. The patient is instructed to take salt water tub baths 3 times daily, followed by application of Silvadene cream (Fig. 69–28).
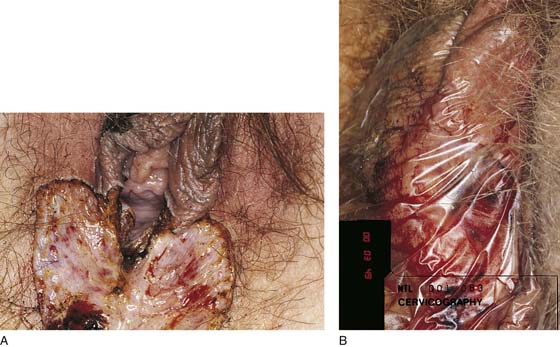
FIGURE 69–1 Raised, pigmented lesions characteristic of vulvar intraepithelial neoplasia (VIN) are clearly seen at the postcommissure, perineum, and lower labia majora.
FIGURE 69–2 The area to be thin section–excised is outlined by carbon dioxide (CO2) laser spots delivered by an UltraPulse CO2 laser coupled to an operating microscope. Spot, 1.5 mm; power, 20 W.
FIGURE 69–3 A 1 : 100 vasopressin solution is injected subdermally. This will serve a dual purpose: as a hemostatic agent and as a heat sink.
FIGURE 69–4 A shallow intradermal cut is made into the tissue with a highly pulsed, powerful laser cutting beam and a fine skin hook.
FIGURE 69–5 Tissue flaps are developed as the laser incision gains in area. Note the excellent hemostasis and the pink color of the skin to be excised, as well as the underlying dermis. The lack of thermal artifact is due to the superpulsed laser beam and the intradermal fluid.
FIGURE 69–6 The “butterfly” area of laser excision is almost complete. The remaining skin on traction, seen on the left side, is ready to be cut off.
FIGURE 69–7 The excised specimen is sent to pathology. The surgeon will be assured that no invasion has occurred and will know the status of deep as well as peripheral margins.
FIGURE 69–8 A. Microscopic section (magnification ×2) showing the excellent preservation and lack of cellular distortion of the thin-section sample. B. High-power view of Figure 69–8A shows the extension of neoplasia into underlying sebaceous glands. A hematoxylin and eosin stain has been used.
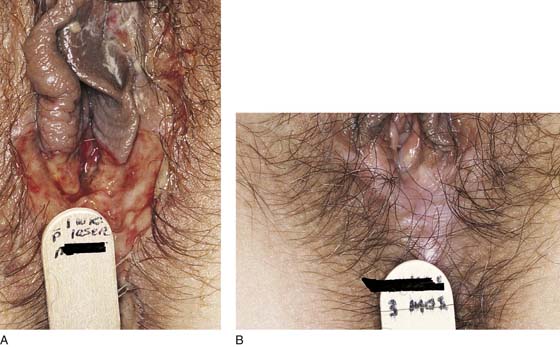
FIGURE 69–9 A. Intraepithelial neoplastic tissues have been completely excised (by intradermal section). The wound has been thoroughly irrigated with normal saline. B. A urethane dressing has been applied to the wound.
FIGURE 69–10 A. The wound is clean and healing at 1 week postoperatively. B. At 3 months, the wound is completely healed with no gross scar formation and no evidence of persisting neoplasia.
FIGURE 69–11 Extensive multifocal carcinoma in situ (CIS) of the vulva. The lesions were previously multiply biopsied and mapped. Note the darkly pigmented warty lesions.
FIGURE 69–12 The areas to be treated are outlined with the carbon dioxide (CO2) laser beam and vaporized with the microscope and laser-coupled micromanipulator. Vaporization carries into the reticular dermis but not the fat.
FIGURE 69–13 Vaporization is complete. Hair-bearing areas are treated to a depth of 2 mm. Non–hair-bearing areas are treated to shallower depths (1 mm).
FIGURE 69–14 The area of vulvar intraepithelial neoplasia (VIN) is outlined with the carbon dioxide (CO2) laser beam at 20 W of power.
FIGURE 69–15 Vaporization with a 2-mm spot (beam diameter) is carried out uniformly to a 2-mm depth.
FIGURE 69–16 Vaporization is complete. The wound is cleansed with sterile water or saline to remove the char.
FIGURE 69–17 Typical flat, warty carcinoma in situ (CIS) of the vestibule and labia minora.
FIGURE 69–18 Carbon dioxide (CO2) laser vaporization to a depth of 1 mm has been completed.
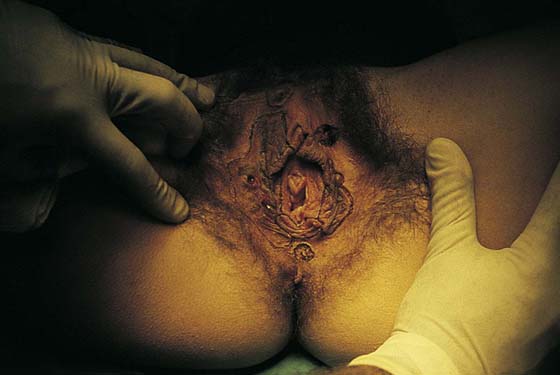
FIGURE 69–19 This patient has a parakeratotic (red) lesion consistent with carcinoma in situ (CIS) involving the left labium majus, perineum, and proximal buttock skin.
FIGURE 69–20 The lesion is trace-marked with the carbon dioxide (CO2) laser after injection of a local anesthetic.
FIGURE 69–21 The area within the tracing is systematically vaporized to a 2-mm depth.
FIGURE 69–22 Vaporization is complete. The wound is irrigated with sterile water and covered with Silvadene cream.
FIGURE 69–23 Typical pigmented, focal papular carcinoma in situ (CIS) of the perianal skin. The lesion has been trace-marked with the carbon dioxide (CO2) laser. A 3-mm margin has been traced.
FIGURE 69–24 The lesion has been completely vaporized. The char has been irrigated away.
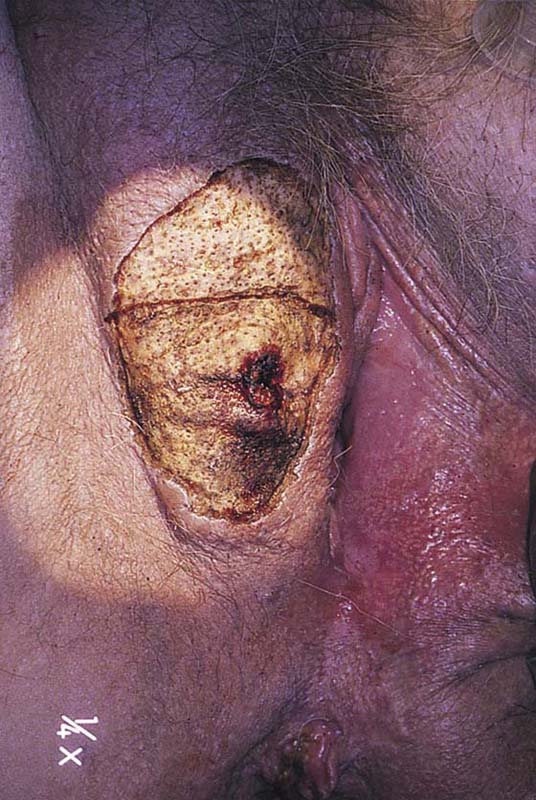
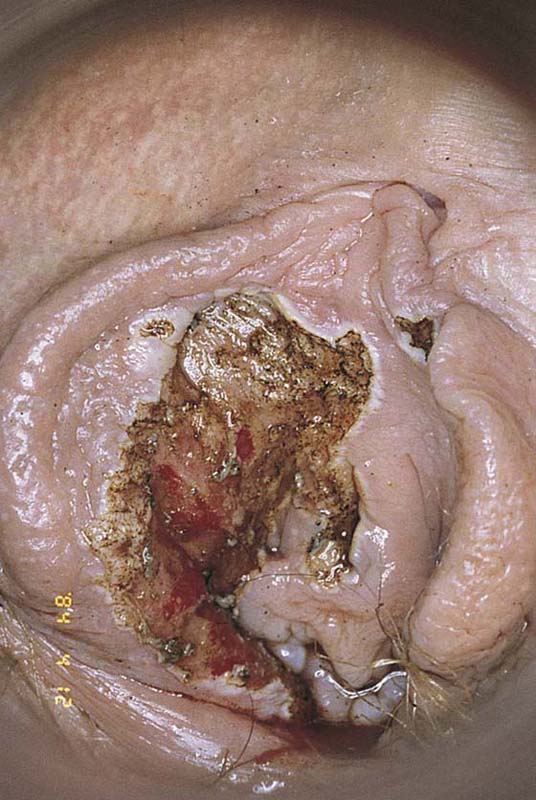
FIGURE 69–25 This woman had a previous “simple” vulvectomy for carcinoma in situ (CIS). Extensive, diffuse anal and perianal recurrent lesions are clearly visible.
FIGURE 69–26 With the patient under general anesthesia, the perianal carcinoma in situ (CIS) is outlined for vaporization.
FIGURE 69–27 The lesions have been completely vaporized to a depth of 1.5 to 2.0 mm, and the wound is covered with Xeroform gauze.
FIGURE 69–28 The same patient depicted in Figure 69–19 at her 1-week postoperative visit. The wound is clean. Healing has begun from the deeper and peripheral skin appendages.