Laparoscopic Surgery for Stress Urinary Incontinence (Burch Colposuspension)
Laparoscopic Burch colposuspension is one of the primary surgical treatment options for stress urinary incontinence. Cure rates appear to be similar to open Burch colposuspension in most studies, although studies with long-term follow-up are not available. Several reviews of the literature on laparoscopic Burch colposuspension have been published.
Laparoscopic Burch colposuspension can be done using an extraperitoneal or an intraperitoneal approach. The intraperitoneal approach to the Burch colposuspension begins with insertion of the laparoscope through a 5- to 10-mm intraumbilical trocar, followed by intra-abdominal insufflation. Inspection of the peritoneal cavity is performed, delineating the inferior epigastric vessels, abdominal and pelvic organs, and any abdominal or pelvic pathology. Two additional trocars (5 mm and 5/12 mm) are placed under direct vision, one on each side in the lower abdomen.
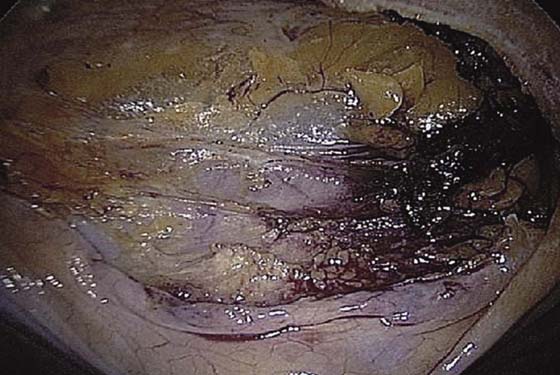
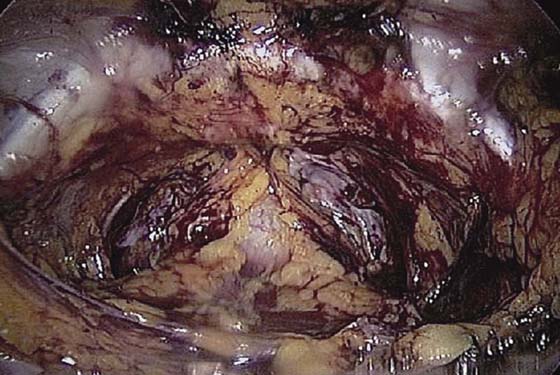
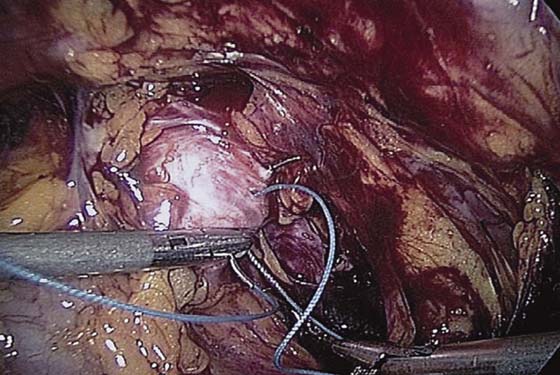
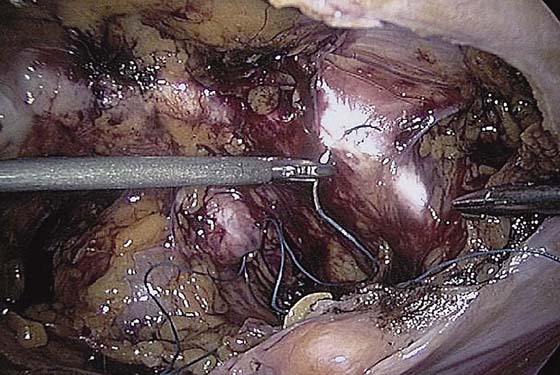
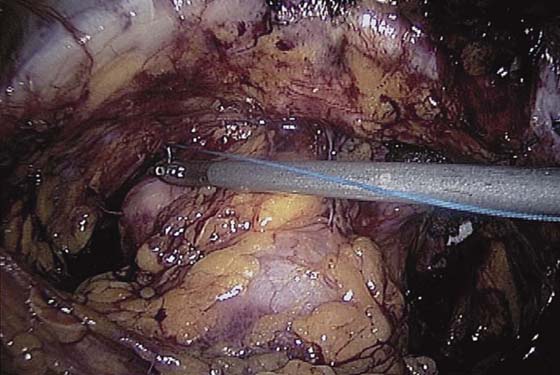
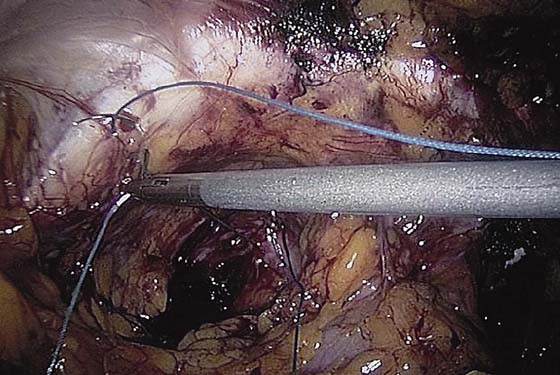
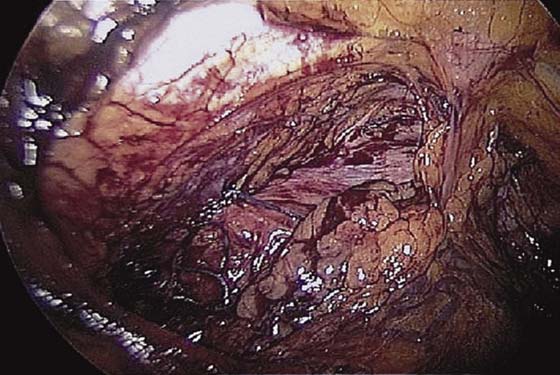
The bladder is filled with 200 to 300 mL sterile water or saline. A probe can be used to press the base of the bladder upward so that the upper margin of the bladder is easily delineated (Fig. 119–1). Using sharp dissection with electrocautery or a harmonic scalpel, a transverse incision is made 2 cm above the bladder reflection between the median umbilical ligaments (Fig. 119–2). Blunt and sharp dissection aiming toward the posterior/superior aspect of the pubic symphysis decreases risk of bladder injury. Identification of the areolar tissue at the point of incision confirms a proper plane of dissection (Fig. 119–3). Blunt dissection is then carried out inferolaterally on both sides to identify the pubic symphysis, Cooper’s ligaments, obturator internus muscles, arcus tendineus fasciae pelvis, and bladder neck (Fig. 119–4). Midline dissection over the urethra should be avoided.
FIGURE 119–1 The bladder is filled before the Burch colposuspension is begun. The upper margin of the bladder can be delineated by pressing up on the base of the bladder.
FIGURE 119–2 Sharp dissection is used to incise the peritoneum 2 cm above the bladder reflection.
FIGURE 119–3 Identification of areolar tissue at the point of incision confirms the proper plane of dissection.
FIGURE 119–4 The space of Retzius is visualized.
After the space of Retzius is exposed, the surgeon places two fingers in the vagina and identifies the urethrovesical junction by placing gentle traction on the Foley catheter. Using a vaginal finger to elevate the vaginal wall lateral to the bladder neck, we place stitches in the vaginal wall excluding the vaginal epithelium at the level of, or just proximal to, the midurethra and bladder neck (Fig. 119–5). A 0 nonabsorbable suture is placed in a figure-of-8 stitch, incorporating the entire thickness of the anterior vaginal wall. The needle is then passed through Cooper’s ligament ipsilaterally (Fig. 119–6). If a double-armed suture is used, we make two passes through Cooper’s ligament and subsequently tie above the ligament. We place Gelfoam between the vaginal wall and the obturator fascia before knot-tying to promote fibrosis. With simultaneous vaginal elevation, the suture is tied with six extracorporeal square knots. Two granny half-hitches and a flat square knot secure the stitch (Fig. 119–7).
Sutures are tied as they are placed to avoid tangling. Midurethral sutures are placed first, although this is a matter of preference. It is easier to place stitches from the contralateral low abdominal port. Fig. 119–8 shows the left bladder neck suture being placed from the right lower quadrant port, although it is possible to place it from either side. Both ends of the suture are then sutured into Cooper’s ligament (Fig. 119–9) and tied. Two sutures are placed on each side to complete the operation (Fig. 119–10). The appropriate level of bladder neck elevation is estimated with the surgeon’s vaginal hand. The goal is to elevate the vaginal wall to the level of the arcus tendineus fasciae pelvis bilaterally, so that the bladder neck is supported and stabilized by the vaginal wall. In tying the sutures, the surgeon should not reapproximate the vaginal wall to Cooper’s ligament or place too much tension on the vaginal wall. A suture bridge of 1.5 to 2 cm is common.
If the patient has a large anterior vaginal wall prolapse, a paravaginal defect repair can be done in conjunction with a Burch colposuspension. When this is done, we bluntly dissect the paravaginal spaces on each side of the bladder. The dissection should identify bilaterally the lateral and lower edges of the bladder and urethra, the anterior vaginal wall and endopelvic fascia, the obturator internus muscle and fascia, and the arcus tendineus fasciae pelvis (Fig. 119–11). The arcus tendineus fasciae pelvis is a condensation of obturator fascia that runs from the pubic bone to the ischial spine. The ischial spine should be palpated or visualized as well as possible. Care should be taken to identify the obturator foramen and the neurovascular bundle to avoid damaging the obturator vessels and nerve. Starting at the vaginal apex, a single 2-0 nonabsorbable, 36- or 48-inch suture on a CT-2 needle is used to place a suture in the full thickness of the vagina, excluding the vaginal epithelium, and then into the arcus tendineus fasciae pelvis, which is 3 to 4 cm below the obturator fossa. This suture is then tied extracorporeally. An additional three to five sutures are placed through the vaginal wall and into the arcus tendineus fasciae pelvis or the fascia of the obturator internus muscle at 1-cm intervals until the defect is closed (Fig. 119–12). The same procedure is performed on the opposite side. If the procedure is performed concomitantly with the Burch colposuspension, the paravaginal defect repair should be performed first because exposure of the lateral defects decreases after the Burch sutures are tied. We place the stitch at the level of the ischial spine first and then place subsequent stitches as needed toward the pubic bone.
FIGURE 119–5 Using laparoscopic suturing technique, a suture is placed in the right vaginal wall and endopelvic fascia at the level of, or just proximal to, the midurethra and bladder neck.
FIGURE 119–6 The needle is passed through Cooper’s ligament ipsilaterally.
FIGURE 119–7 The right Burch colposuspension suture is tied using extracorporeal knot-tying technique.
FIGURE 119–8 The left periurethral suture is placed at the level of the bladder neck.
FIGURE 119–9 Both ends of the left periurethral suture are placed through Cooper’s ligament from the contralateral port.
FIGURE 119–10 The completed Burch colposuspension procedure is shown with two sutures on each side of the bladder neck.
FIGURE 119–11 The arcus tendineus fasciae pelvis with left paravaginal defect is shown.
FIGURE 119–12 The left paravaginal defect repair is completed with three sutures, before the Burch colposuspension sutures are placed on the left.

 Tommaso Falcone
Tommaso Falcone