Laparoscopic-Assisted Vaginal Hysterectomy
Laparoscopic-assisted vaginal hysterectomy (LAVH) was introduced in the past 20 years as an alternative to abdominal hysterectomy. LAVH is a safe alternative to abdominal hysterectomy when a vaginal hysterectomy is contraindicated. In a prospective randomized clinical trial of LAVH versus abdominal hysterectomy at the Cleveland Clinic Foundation, LAVH was shown to be associated with less postoperative pain, shorter hospital stays, and a more rapid return to normal activities and work than abdominal hysterectomy.
There are several classifications of laparoscopic hysterectomy. The laparoscopic ligation of the uterine artery appears to be the critical step that differentiates a laparoscopic procedure from a laparoscopic-assisted one. In fact, this division is arbitrary. In practice, the procedure is continued laparoscopically until the surgeon is confident that the procedure can be completed vaginally. Ligation of the uterine artery by laparoscopy does not necessarily imply a more difficult case or one requiring more skill. Often the term is meant to convey to the operating room staff whether a vaginal table should be ready for the case.
We do not give oral antibiotics or preoperative bowel preparation. The patient is given a single dose of intravenous antibiotic, usually a cephalosporin, before the procedure. Pneumatic compression stockings are placed on the calves. An orogastric tube is used if stomach distention is suspected. Examination under anesthesia is carried out, and a Foley catheter is inserted.
A standard three-port technique is used: one umbilical and one in each lower quadrant. One of the lower ports is a 10-mm site for introduction of an electrocoagulating/cutting device such as a Seitzinger tripolar cutting forceps (Cabot Medical, Langhorne, Pennsylvania). We use the electrosurgical device set at 50W pure cut current.
We use a Hulka tenaculum as our uterine manipulator. A useful instrument for a total laparoscopic hysterectomy is a Koh colpotomizer (CooperSurgical Inc, Trumbull, Connecticut). This rigid cone fits on the RUMI uterine manipulator (CooperSurgical) and fits snugly on the cervix. It serves to delineate the fornices of the vagina that will be incised laparoscopically. This apparatus also has a balloon that will prevent escape of carbon dioxide through the vagina. The vaginal table should include vaginal wall retractors and long instruments. At the end of the case a cystoscopy is performed. The bladder should be distended to check for injury. Intravenous indigo carmine also can be used to verify the integrity of the ureters.
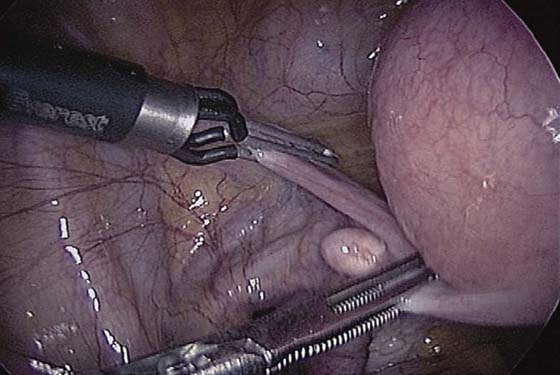
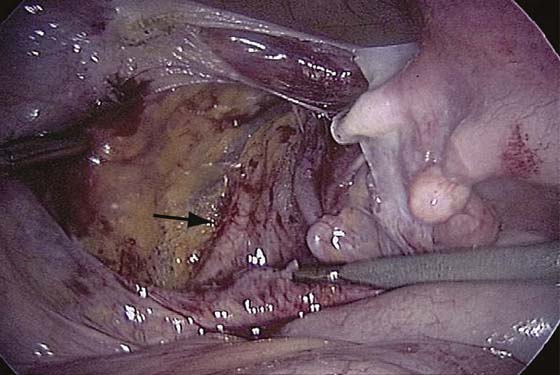
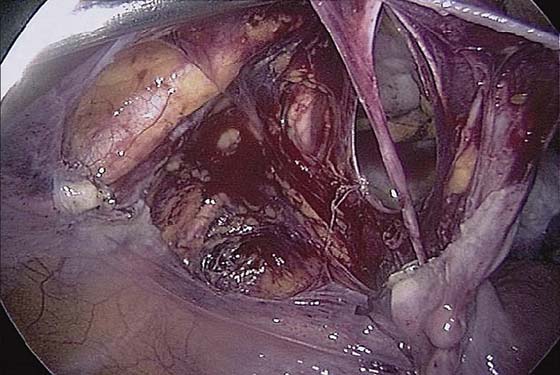
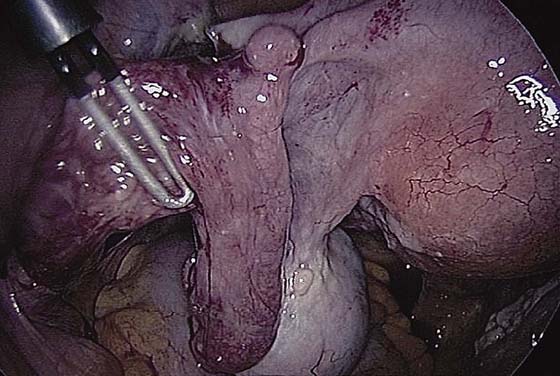
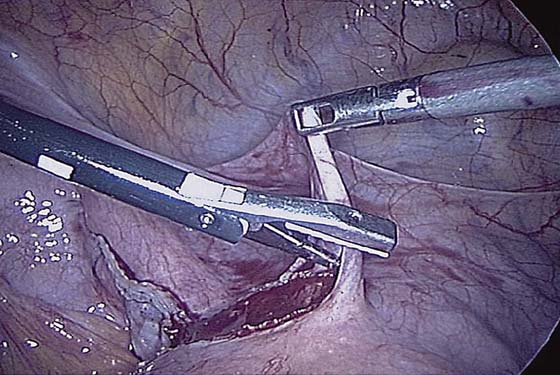
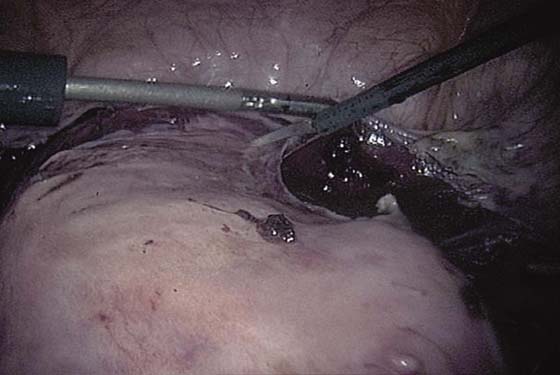
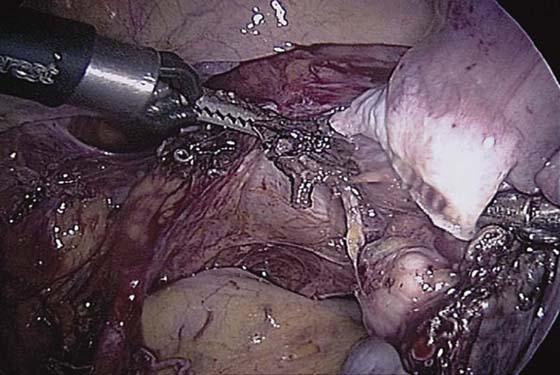
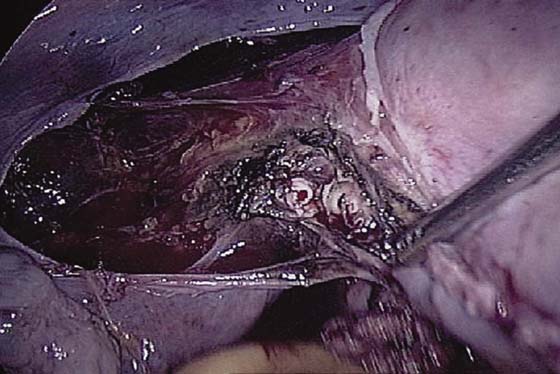
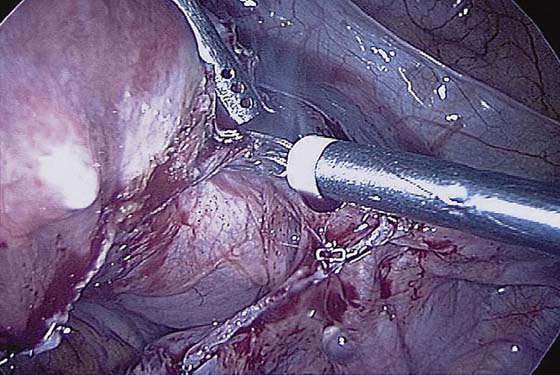
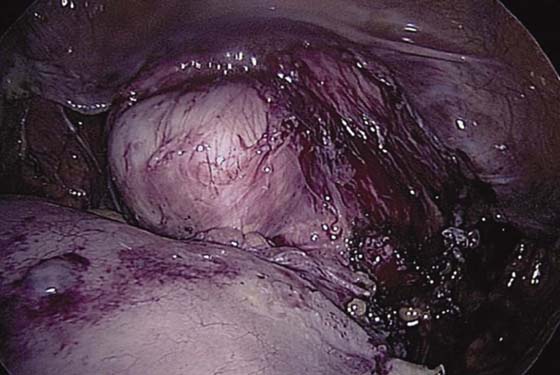
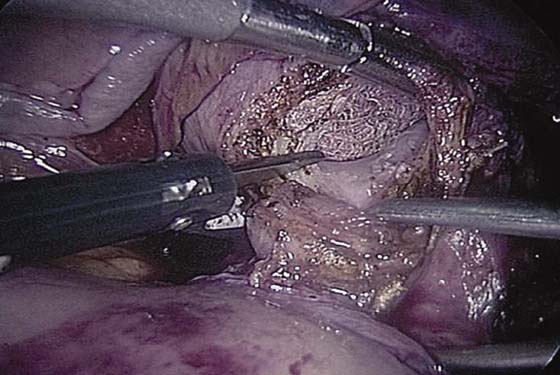
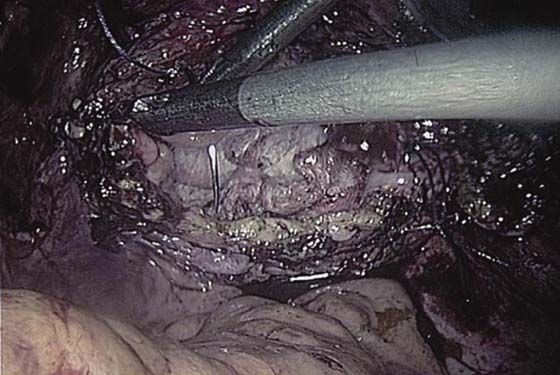
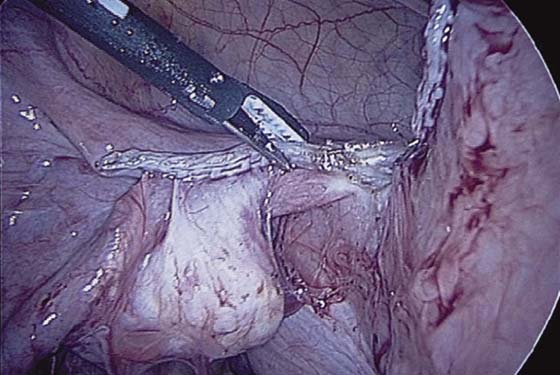
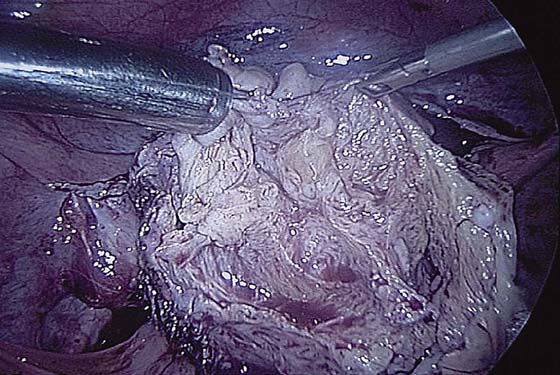
The technique of LAVH is as follows: The round ligament is electrocoagulated and transected (Fig. 117–1). The uterus is pulled to the opposite side. The incision from the round ligament is carried cephalad to open the retroperitoneal space lateral to the ovarian vessels (Fig. 117–2) and caudad to incise the bladder peritoneum. The ureter is then identified and kept in view. A peritoneal window is made (Fig. 117–3). The ovarian vessels are grasped and electrocoagulated (Fig. 117–4). The bladder peritoneum is then dissected downward until the vagina is identified (Figs. 117–5 and 117–6). The uterine artery is identified and electrocoagulated (Figs. 117–7 through 117–9). The process is repeated on the opposite side. A sponge forceps is placed in the vagina in the anterior fornix, and the vagina is tented upward (Fig. 117–10). An incision is made circumferentially around the vagina (Fig. 117–11). After removal of the uterus through the vagina, carbon dioxide (CO2) may escape through the vagina. If the Koh colpotomizer is used, the balloon will prevent this. If not, the vagina can be packed. The vault is then sutured with 0 Vicryl on a CT-1 needle (Fig. 117–12). Three to four interrupted stitches are placed and tied extracorporeally. A McCall’s culdoplasty is generally performed.
The patient is usually discharged within 24 hours. Some patients can return to work as early as 1 week after surgery, but most require 4 weeks of convalescence.
If the ovaries are conserved, surgery starts with occlusion and transection of the utero-ovarian ligaments. This can be accomplished with bipolar energy or with a stapling device (Figs. 117–13 and 117–14). However, the use of a stapling device is not cost effective.
If a supracervical hysterectomy is performed, the specimen will require morcellation (Fig. 117–15). The morcellator device usually requires a 10/12-mm port. The cervical stump is closed, and the bladder peritoneum is sutured over it (Fig. 117–16).
FIGURE 117–1 The round ligament is grasped, electrocoagulated, and cut.
FIGURE 117–2 The retroperitoneal space is dissected, and the ureter is identified (arrow).
FIGURE 117–3 A window is made in the medial leaf of the broad ligament above the ureter.
FIGURE 117–4 The ovarian vessels are grasped and electrocoagulated.
FIGURE 117–5 The bladder peritoneum can be dissected downward with a harmonic energy device (Ultrashears, US Surgical, Norwalk, Connecticut).
FIGURE 117–6 The bladder peritoneum can be dissected downward with scissors using electrosurgery.
FIGURE 117–7 The uterine artery is identified along the uterus and is electrocoagulated and cut.
FIGURE 117–8 The transected uterine artery is seen.
FIGURE 117–9 The procedure is repeated on the other side using a bipolar cautery.
FIGURE 117–10 The vagina is tented upward with a sponge stick in the vagina.
FIGURE 117–11 The vagina is then incised. In this case, harmonic energy is used (Ultrashears, US Surgical, Norwalk, Connecticut). Note that a laparoscopic tenaculum on the cervix moves the specimen around. Note the sponge in the vagina to prevent escape of carbon dioxide.
FIGURE 117–12 The vagina is closed with 0 Vicryl on a CT-1 needle. Note the sponge in the vagina to prevent gas from escaping.
FIGURE 117–13 A multifire Endo GIA (US Surgical, Norwalk, Connecticut) stapling device with a vascular cartridge has been applied across the utero-ovarian and round ligaments.
FIGURE 117–14 The instrument has been fired and the transection site is examined for bleeding.
FIGURE 117–15 A morcellator (Steiner Electromechanic Morcellator, Karl Storz GmbH & Co KG, Tuttlingen, Germany) has been introduced through a 10/12-mm port. The uterus is morcellated and is removed in pieces.
FIGURE 117–16 The cervical stump is sutured closed and the bladder peritoneum is sutured to the peritoneum behind the cervix. A knot pusher is used for extracorporeal tying.

 Mark D. Walters
Mark D. Walters