CHAPTER 3 Labral Pathology
Our understanding of labral pathology as a cause of hip pain is evolving. The exact prevalence of acetabular labral tears in the general population is unknown. Injuries to the acetabular labrum are the most consistent pathologic findings identified at the time of hip arthroscopy. In the review of their last 300 cases by Kelly and colleagues,1 labral tears were present in 90%. Labral tears are most frequently anterior and often are associated with sudden twisting or pivoting motions.
ANATOMY AND PATHOANATOMY
The hip labrum is a fibrocartilaginous structure that surrounds the rim of the acetabulum in an almost circumferential manner. It is contiguous with the transverse acetabular ligament across the acetabular notch. The labrum is widest in the anterior half, thickest in the superior half, and merges with the articular hyaline cartilage of the acetabulum through a transition zone of 1 to 2 mm.2 The labrum is firmly attached to the rim of the acetabulum. Its junction with the osseous margin is irregular, and there may be extension of bone into the substance of the labrum. A group of three or four vessels is located in the substance of the labrum on the capsular side of this bony extension from the acetabulum and penetrates into the peripheral third of the labrum. The labrum is separated from the hip capsule by a narrow synovium-lined recess.3 Extrapolating from our understanding of the healing capacity of the meniscus, repair strategies should be considered for tears involving only the peripheral labrum.
Function
We are only beginning to understand the function of the labrum. The bony congruity of the hip joint allows for primary stability. The labrum functions as a secondary stabilizer by extending the acetabular congruity and helping maintain the negative intra-articular pressure within the joint. This has been confirmed through a poroelastic finite model that showed the labrum helps provide structural resistance to lateral motion of the femoral head within the acetabulum.4 Furthermore, it has been demonstrated that the labrum decreases the contact pressures within the hip, probably as a result of its effect on maintaining the articular fluid in contact with the weight-bearing cartilage.5
Causes of Labral Tearing
There are many theories on the mechanism of labral tearing, suggesting that the cause is multifactorial. Kelly and associates1 have identified at least five causes of labral tears: (1) trauma, (2) femoroacetabular impingement (FAI), (3) capsular laxity and hip hypermobility, (4) dysplasia, and (5) degeneration.
Injury to the labrum could occur with traction, which would cause a tear resulting from excessive or repetitive external rotation of the femoral head on the anterior labrum.6 Compression forces may also tear the labrum through excessive and repetitive flexion and/or internal rotation of the hip. This process could be accelerated with FAI (see Chapter 4). Atraumatic instability has also been attributed to a deficient labrum associated with redundant capsular or ligamentous tissue that allows for more strain, and may transiently cause an incongruent joint. Deformities of the femoral head or acetabulum (e.g., slipped capital femoral epiphysis lesions, Legg-Calvé-Perthes disease, developmental dysplasia of the hip) have been discussed as a cause of labral tearing from incongruities between the femur and acetabulum.7
In the setting of a normal labrum, supraphysiologic loads would be required to produce a labral tear. Conversely, in the setting of an abnormal labrum, tearing could occur at physiologic loads. Sports that require repeated hip rotation, such as football, golf, gymnastics, soccer, ballet, and baseball, are susceptible to overuse injuries to the labrum and capsuloligamentous complex.8
Regardless of the mechanism, most labral tears encountered at the time of arthroscopy occur in the anterior quadrant. In a series by Fitzgerald,9 45 of 49 labral injuries were documented in the anterior marginal attachment of the acetabulum. These findings were supported by another study, which reported that 96% of labral tears encountered in a series of 436 consecutive hip arthroscopies occur in the anterior quadrant.10
The data from cadavers show that labral lesions are extremely common, present in 93% of specimens. Because the labrum is thought to be a stabilizing structure in the hip, labral lesions might contribute to the development of osteoarthritis in numerous ways. Injury or degeneration of the labrum may result in instability of the femoral head in the acetabulum, resulting in cartilage damage adjacent to the damaged labrum. This instability also might be more widespread, resulting in cartilage damage in the weight-bearing region of the acetabulum.6 Finally, the lack of a seal may affect cartilage density as a result of fluid loss from the central articular compartment.4
HISTORY AND PHYSICAL EXAMINATION
The clinical presentation of patients with a tear of the labrum is variable and, as a result, the diagnosis is often missed initially. Burnett and coworkers11 have reported on a series of 66 patients in whom the diagnosis of a labral tear had been made by arthroscopy. In this series, the mean time from onset of symptoms to diagnosis was 21 months. An average of 3.3 health care providers had seen each patient prior to their being diagnosed. Groin pain was the most common complaint (92%), with the onset of symptoms most often insidious. The most common examination finding was a positive impingement sign, which occurred in 95% of patients in this series.
Most patients who present with labral injury report activity-related groin pain in the affected hip. A few patients also report gluteal or trochanteric pain, secondary to aberrant gait mechanics. In some patients, the gluteal pain may be a sign of posterior labral injury. Although most patients do not specifically report loss of hip range of motion (ROM), this finding is almost universally seen. Hips with structural abnormalities, such as acetabular retroversion, coxa profunda, or pistol grip deformities, may have decreased ROM from anatomic limitations, but may also be limited by pain. Patients with pathologic hip conditions also commonly develop late capsulitis, synovitis, and/or trochanteric bursitis. Differential diagnosis of the classic mechanical symptoms (painful catching or clicking) of labral tears includes a snapping iliotibial tendon or hypermobile psoas tendon.1 Many other conditions can produce symptoms around the hip. The differential diagnosis should include an array of disorders such as sacroiliitis, degenerative disk disease, abductor muscle problems, osteonecrosis, psoas tendinitis, pubic rami fractures, and stress fractures of the proximal femur. More chronic problems are usually associated with trochanteric bursitis.12
In addition to functionally limiting symptoms, reproducible physical findings, and mechanical symptoms, restricted ROM from pain or a perceived mechanical block is a further indication of an intra-articular cause. Findings on physical examination can include a positive McCarthy sign—with both hips fully flexed, the patient’s pain is reproduced by extending the affected leg, first in external rotation and then in internal rotation. Also common is inguinal pain with flexion, adduction, and internal rotation of the hip, as well as anterior inguinal pain with ipsilateral resisted straight leg raising.13 The pain, which may be of sudden onset or associated with a traumatic event such as a fall or twisting injury, is generally exacerbated with activity and does not respond to conservative treatment including ice, rest, nonsteroidal anti-inflammatory drugs (NSAIDs), and physical therapy. Conservative treatment may be successful for muscle strains but not for acetabular labral tears.
The impingement test was first described for patients with femoroacetabular impingement, but is equally useful for labral injuries. With the hip at 90 degrees of flexion, maximum internal rotation and adduction is performed. Contact between the anterosuperior acetabular rim and femoral neck elicits pain (Fig. 3-1). The hip can also be tested at varying degrees of flexion. Posterior labral tears can be tested with the leg externally rotated and in hyperextension.
DIAGNOSTIC IMAGING
Multiple studies have demonstrated the superior accuracy of magnetic resonance arthrography (MRA) over standard magnetic resonance imaging (MRI) for diagnosing labral tears. Intra-articular gadolinium has been shown to improve the sensitivity of diagnosing labral pathology from 25% to 92% using a small field of view.14 Therefore, when clinical suspicion of a hip labral tear exists, MRA using a small field of view is the study of choice.
An intra-articular bupivacaine injection may be useful in situations in which the diagnosis of labral pathology is equivocal or if a tear has been diagnosed by MRA,15 but it is uncertain whether symptoms are related to this finding. Similar to its use in diagnosing external impingement of the shoulder, if patients experience relief from their symptoms following the injection, the diagnosis of pain secondary to hip intra-articular pathology is more certain. However, intra-articular pathology could still be present without pain relief from an injection.16
CLASSIFICATION
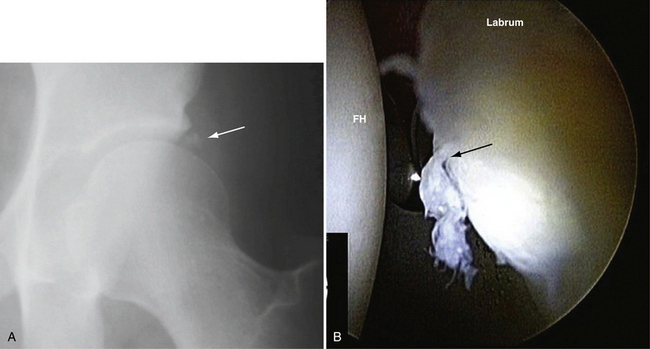
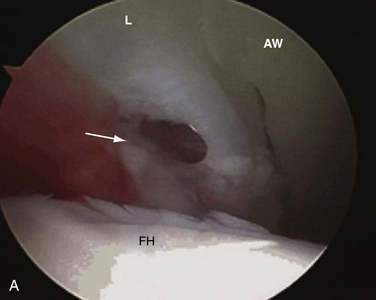
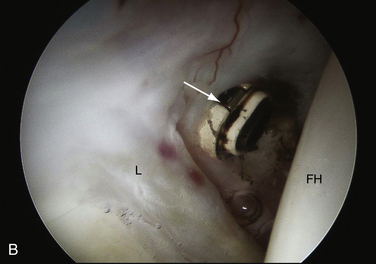
A outcome correlated classification system of labral injuries and chondral damage has been created by McCarthy and colleagues17 Stage 0, as compared with a normal acetabular labrum, is a contusion of the labrum with adjacent synovitis. Stage 1 is a discrete labral free margin tear with intact articular cartilage of the acetabulum and femoral head. Stage 2 is a labral tear with focal articular damage to the subjacent femoral head but with intact acetabular articular cartilage. Stage 3 is a labral tear with an adjacent focal acetabular articular cartilage lesion, with or without femoral head articular cartilage chondromalacia. Stage 4 constitutes an extensive acetabular labral tear with associated diffuse arthritic articular cartilage changes in the joint (Fig. 3-2). The labral injury involved the anterior half of the joint 95% of the time. All patients who had combined anterior and lateral labral injuries had associated degenerative arthritis in the joint.
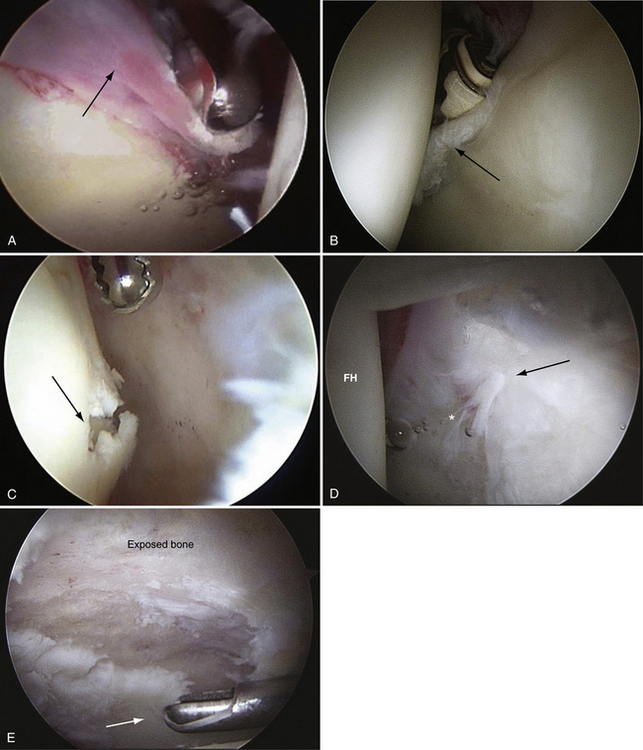
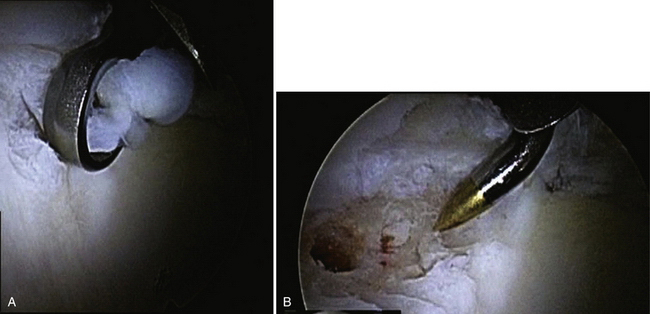
FIGURE 3-2 Classification of labral tears. A, Stage 0—labral contusion (arrow) with synovitis. B, Stage 1—labral tear (arrow) with intact articular cartilage of the acetabulum and femoral head. C, Stage 2—labral tear with focal articular damage (arrow) to the subjacent femoral head but with intact acetabular cartilage. D, Stage 3—labral tear (arrow) with an adjacent focal acetabular cartilage lesion, with or without femoral head (FH) articular cartilage damage. E, Stage 4—extensive acetabular labral tear, with associated diffuse arthritic articular cartilage changes in the joint. The arrow delineates transition to normal cartilage.
TREATMENT
Surgical Management
Arthroscopic Technique
The decision to proceed with operative intervention should be heavily weighted on refractory pain and mechanical symptoms. Most labral tears are treated with débridement. However, some tears are amenable to arthroscopic repair. As noted, the blood supply to the labrum enters from the adjacent joint capsule. Vascularity was detected in the peripheral third of the labrum whereas the inner two thirds of the labrum were avascular. Thus, peripheral tears have healing potential and repairs should be considered if this is observed at the time of surgery. However, McCarthy and colleagues6 have reported on 436 consecutive hip arthroscopies, including 261 labral tears, and all the tears were located at the relatively avascular articular junction.
Arthroscopic Labral Débridement.
It is our preference to use a general anesthetic supplemented with a lumbar plexus block for post-perative analgesia and relaxation.18 The procedure can be performed in the supine or lateral position and should use both a 30- and 70-degree arthroscope for a thorough assessment of the labrum and any associated pathology. Modified arthroscopic flexible instruments, extended shavers, and hip-specific instrumentation should be available to improve access to all areas of the joint.
The goal of the surgical procedure should be to preserve as much tissue as is technically feasible while resecting the degenerative or damaged material. This is important to maintain the labrum’s role as a secondary joint stabilizer and minimize the potential for arthrosis. Fraying from the labral tears should be débrided with the use of motorized shavers or RF probes. Placing absorbable suture through the defect and tying the suture through the capsule can stabilize intrasubstance labral tears. It is important to delineate the areas of abnormal tissue identified on radiographs (in the form of perilabral calcifications) and on MRA and MRI scans (abnormal signal intensity) to address the labral pathology thoroughly. Occasionally, perilabral calcifications can be in the formative stage; these should be sought out and decompressed (Fig. 3-3).
Adjacent cartilage damage should be sought and thoroughly assessed. Superficial lesions can be gently débrided with mechanical shavers and perhaps stabilized with the use of RF probes. Grade IV Outerbridge lesions may be managed with a thorough débridement down to a bleeding bed and preparation with microfracture awls (Fig. 3-4).
Arthroscopic Labral Repair.
The decision to perform a labral repair is still a process in its infancy. The current indications are symptomatic tears that have obvious vascularity within their substance or are reparable to the acetabular bony wall or adjacent capsule. In general, a tear less than 1cm in length does not require repair because there are minimal associated instability and mechanical symptomatology. Expert arthroscopic skills and appropriate instrumentation are also required to perform this repair. It can be performed in the supine or lateral position under general anesthesia, often supplemented with a lumbar plexus block (see earlier).
Best results can be expected with operations with the correct indications, as follows:
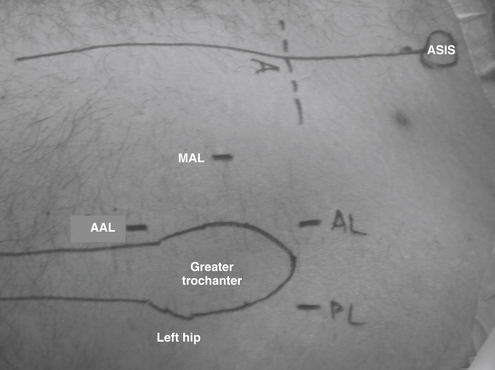
The arthroscopic technique uses routine anterior and anterolateral portals and an accessory midanterior portal that is halfway between the two portals and 5 cm distal (Fig. 3-5). This accessory portal allows for a more appropriate angle for suture anchor placement. However, caution should be taken in creating this portal because excessively distal placement places the ascending lateral circumflex artery at risk, with the possibility of bleeding and compromise of the surgical field.19
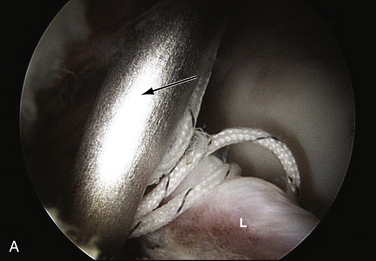
As with labral débridement, the procedure includes a diagnostic arthroscopy, with treatment of any associated pathology. Any degenerative tissue is débrided, and the labrum is elevated from the bone. The bony bed is prepared by decorticating with a curette or shaver to stimulate healing (Fig. 3-6).
One important consideration is to develop adequate access to the joint. Unlike the shoulder, the hip capsule is significantly thicker and less forgiving with respect to maneuverability within the joint. Therefore, a generous capsulotomy should be considered in many cases so that instruments can be moved within the joint and to limit the amount of iatrogenic damage to the articular cartilage. The capsulotomy can be performed with an arthroscopic knife or RF probe (Fig. 3-7). In addition, the use of slotted cannulas can make delivery of curved instruments significantly easier (Fig. 3-8). These devices are available in a variety of lengths and circumferences to allow their use in the hip.
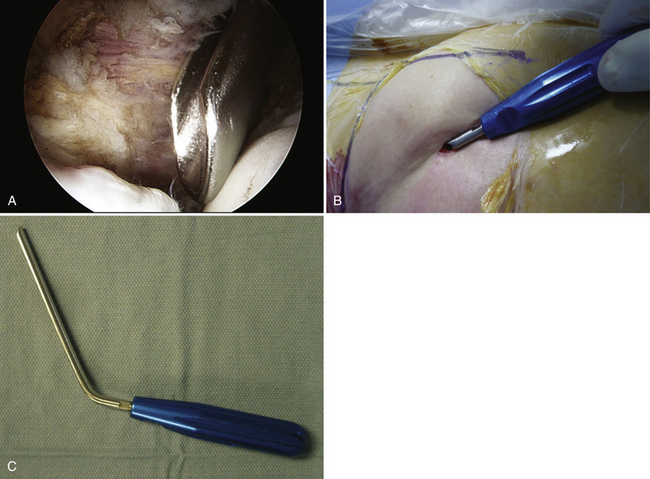
FIGURE 3-8 Use of a slotted cannula for instrument insertion. A, Endoscopic view of tool in place. The device is in the anterior portal of a right hip while viewed from the anterolateral portal. B, External view of cannula in place. C, Slotted cannula device.
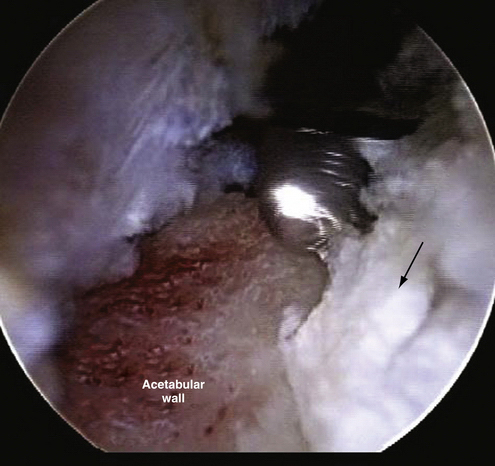
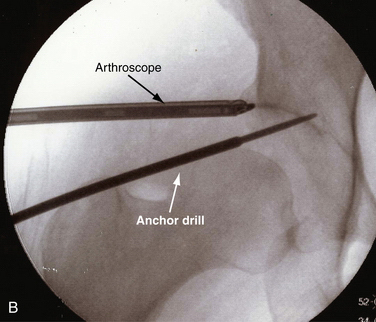
Similar to arthroscopic labral repair in the shoulder, suture anchors are effective to reattach labrum to bone. The position of the anchor is critical in re-establishing the normal anatomy of the labrum. It should be placed on the acetabular rim, with care to avoid penetrating into the articular cartilage. In contrast to the shoulder, the acetabular cavity is concave. This makes the requisite angle of the anchor insertion significantly more acute. Avoiding chondral injury, both to the head (delivery of the anchor) and with respect to acetabular penetration, is important, because it can become a factor in joint degeneration. Both endoscopic and fluoroscopic visualization are essential (Fig. 3-9). There are many options for suture anchors, some requiring traditional arthroscopic knot tying; knotless type anchors have recently been developed (Fig. 3-10).
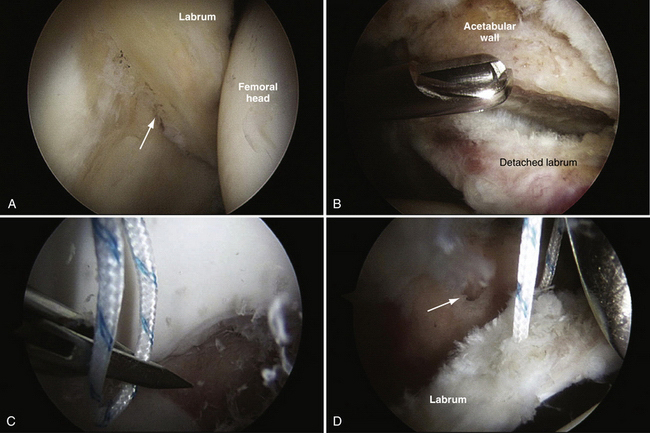
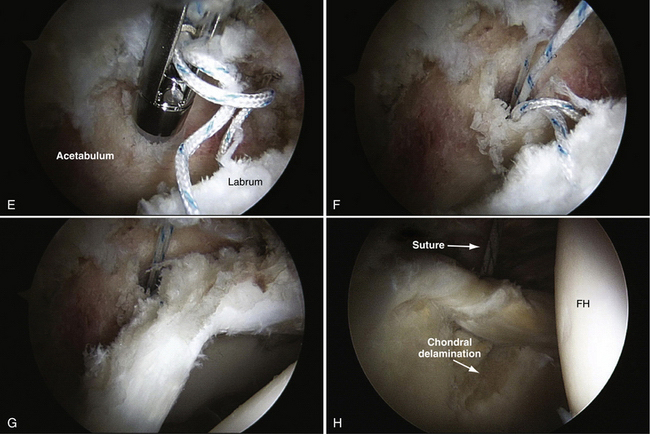
FIGURE 3-10 Repair of labrum using a knotless technique. This is a right hip in a patient with an associated chondral area of delamination. A, Initial view of tear from the anterolateral portal. B, Prepared site viewed from the anterior portal. The burr is inserted from the anterolateral portal. C, Capture of the labral tissue with a penetrator device. D, Final suture mattress in place in robust tissue. The arrow is pointing to the prepared anchor insertion site. E, Anchor in position for insertion into acetabular wall with loose sutures viewed is from the anterolateral portal. F, Anchor in place with suture prepared for advancement. G, Final repair viewed from the peripheral compartment (anterolateral portal) showing re-creation of the labral contour. H, Final repair viewed from the central compartment (anterolateral portal). FH, femoral head.
With a tear in the labrocapsular junction, the repair can be performed, attaching the labrum to the adjacent capsular tissue. Intrasubstance tears may be addressed in a similar manner. The cleavage plane in the labrum should be defined and débrided of nonviable tissue. A suture shuttle device can be used to deliver a looped monofilament suture between the junction of the articular cartilage and the fibrocartilage labrum. A suture penetrator is used through the capsule to grasp the loop of monofilament. The looped shuttle is used to shuttle a monofilament suture around the labral tear and through the capsule. The suture is then tied in an extra-articular position.
PEARLS& PITFALLS
The use of slotted cannulas, instead of disposable plastic devices (see Fig. 3-8), makes the insertion of longer tools and curved tools significantly easier in the hip joint. For the reasons noted, the hip capsule is very restricting. The insertion of plastic cannulas is fraught with difficulties, including articular cartilage damagepon insertion. With a slotted cannula, the capsular entry point is preserved and maneuverability within the joint is enhanced compared with using a closed cannula.
The liberal use of fluoroscopy while anchor insertion points are chosen allows for anchors to be placed in a safe location, with a minimal likelihood of penetrating the articular cartilage and causing iatrogenic damage. Unlike the glenoid cavity, the acetabulum is concave, making the angle of approach completely different to avoid penetration. The distortion that accompanies the use of the 70-degree arthroscope further confuses the situation and makes the use of fluoroscopy even more important.
POSTOPERATIVE PROTOCOL
Rehabilitation Following Labral Repair
Formal therapy for ROM and strengthening of the operative hip is also begun 7 to 10 days following surgery. Early ROM is initiated to limit the scarring in the joint associated with surgical trauma. Weight bearing following repair should be restricted to foot-flat (20% of body weight) ambulation for the first 4 weeks. The most important principle is to limit the rotational stresses that the repaired labrum experiences in the first few weeks. The range that puts the repair at risk includes flexion past 90 degrees, abduction past 25 degrees, and internal or external rotation past 25 degrees.20 Limitations are placed on flexion past 90 degrees for 10 days, whereas abduction and abduction are limited to 25 degrees for 4 weeks. Beginning at 4 weeks, a gradual progression from increasing the ROM to unrestricted strengthening is begun. The use of stationary bicycling is encouraged and instituted in the first 10 days. Aggressive hip flexor strengthening should also be limited until full ROM is obtained and hip mechanics are relatively normal. As noted, a significant tendinitis can develop, thus slowing recovery. Explosive and rotational activities should also be limited for at least 12 weeks. The return to unrestricted activity is also predicated on a full pain-free ROM, and normal strength of the pelvic, abdominal, and lower extremity musculature. This typically occurs at approximately 4 to 6 months postoperatively.
OUTCOMES
At a minimum of 2 years after hip arthroscopy, patient results were directly correlated with the stage of labral injury.21 There were 11 stage 0 lesions and 1 labral lesion, with all but one of these patients having good to excellent results (91%). There were 11 patients with stage 2 labral tears, with 82% good to excellent outcomes when the tear was resected. Two patients (18%) required additional surgical intervention, including open synovectomy, capsulectomy, and release of the reflected rectus femoris tendon secondary to poor results. Patients with stage 3 labral tears did not fare nearly as well and the extent of the acetabular cartilage erosion directly affected the result, with only 17% having good to excellent results. The results of patients with stage 4 labral tears (nine hips) directly correlated with the extent of hip degenerative arthritis. If the articular cartilage involvement was diffuse on the femoral head and acetabulum, regardless of the plain radiographic appearance, the symptomatic improvement after arthroscopy was transient. At follow-up, 78% had poor results and 43% eventually had total joint arthroplasty within 2 years of arthroscopy. These results have been confirmed with the only long-term outcome study of labral débridement by Byrd and Jones.22
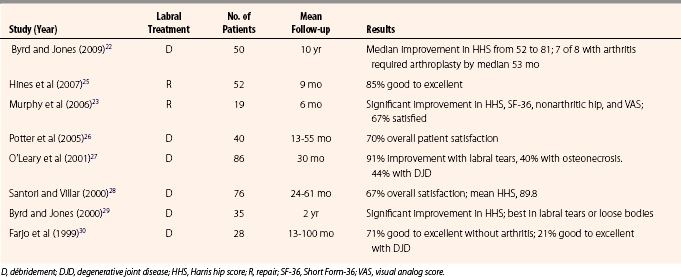
To date, there are no published series on the long-term outcome of arthroscopic repair of hip labral tears. Indications for which lesions constitute a reparable lesion are currently evolving. Recently, Hines and associates25 presented outcome results on a series of 52 patients who underwent arthroscopic hip labral repair, with a mean follow-up of 9 months. Another study of 19 patients by Murphy and coworkers23 has also recently been published. The results of these studies, as well as those documenting the outcome of labral débridement, are summarized in Table 3-1.
COMPLICATIONS
Hip arthroscopy has been shown to be relatively safe in several studies documenting its effectiveness and the number of complications. In one large series, there was a 1.6% complication rate, with problems including transient palsy of the sciatic or femoral nerves, paresthesias secondary to lateral femoral cutaneous nerve palsy, perineal injury, and instrument breakage.24 Although this study was not specific to the repair of the hip labrum, specific problems may be associated with this procedure. As a result of the tight confines and the multiple instruments that are inserted into the joint, the possibility of serious articular cartilage damage exists. Care should be taken while working within the joint to ensure that cartilage damage is minimal. In addition, with the insertion of suture anchors, there is a possibility of joint penetration. The liberal use of fluoroscopy to document the position of anchor insertion angles prior to committing to a specific position is critical to a successful procedure.
SUMMARY
The available literature supports the concept that the labrum is important for stability and cartilage homeostasis. More research needs to be done to evaluate the long-term effects of labral repair or excision. It would appear that the preservation of as much relatively normal labral tissue with any surgical procedure is critical to the long-term preservation of the native hip joint.
1. Kelly BT, Weiland DE, Schenker ML, Philippon MJ. Arthroscopic labral repair in the hip: surgical technique and review of the literature. Arthroscopy. 2005;21:1496-1504.
2. Seldes RM, Tan V, Hunt J, et al. Anatomy, histologic features, and vascularity of the adult acetabular labrum. Clin Orthop Relat Res. 2001;382:232-240.
3. Petersilge C. Imaging of the acetabular labrum. Magn Reson Imaging Clin North Am. 2005;13:641-652.
4. Ferguson SJ, Bryant JT, Ganz R, Ito K. The acetabular labrum seal: a poroelastic finite element model. Clin Biomech (Bristol, Avon). 2000;15:463-468.
5. Ferguson SJ, Bryant JT, Ganz R, Ito K. The influence of the acetabular labrum on hip joint cartilage consolidation: a poroelastic finite element model. J Biomech. 2000;33:953-960.
6. McCarthy J, Noble P, Aluisio FV, et al. Anatomy, pathologic features, and treatment of acetabular labral tears. Clin Orthop Relat Res. 2003;406:38-47.
7. Byrd JW, Jones KS. Hip arthroscopy in the presence of dysplasia. Arthroscopy. 2003;19:1055-1060.
8. Byrd JW. Hip arthroscopy in athletes. Instr Course Lect. 2003;52:701-709.
9. Fitzgerald RH. Acetabular labrum tears. Diagnosis and treatment. Clin Orthop Relat Res. 1995;311:60-68.
10. McCarthy JC, Noble PC, Schuck MR, et al. The watershed labral lesion: its relationship to early arthritis of the hip. J Arthroplasty. 2001;16:81-87.
11. Burnett RS, Della Rocca GJ, Prather H, et al. Clinical presentation of patients with tears of the acetabular labrum. J Bone Joint Surg Am. 2006;88:1448-1457.
12. Sierra RJ, Trousdale RT, Ganz R, Leunig M. Hip disease in the young, active patient: evaluation and nonarthroplasty surgical options. J Am Acad Orthop Surg. 2008;16:689-703.
13. McCarthy JC. The diagnosis and treatment of labral and chondral injuries. Instr Course Lect. 2004;53:573-577.
14. Toomayan GA, Holman WR, Major NM, et al. Sensitivity of MR arthrography in the evaluation of acetabular labral tears. AJR Am J Roentgenol. 2006;186:449-453.
15. Byrd JW, Jones KS. Diagnostic accuracy of clinical assessment, magnetic resonance imaging, magnetic resonance arthrography, and intra-articular injection in hip arthroscopy patients. Am J Sports Med. 2004;32:1668-1674.
16. Martin RL, Irrgang JJ, Sekiya JK. The diagnostic accuracy of a clinical examination in determining intra-articular hip pain for potential hip arthroscopy candidates. Arthroscopy. 2008;24:1013-1018.
17. McCarthy J, Wardell S, Mason J, et al. Injuries to the acetabular labrum: classification, outcome, and relationship to degenerative arthritis, Paper presented at: American Academy of Orthopedic Surgeons 64th Annual Meeting; February 1997, San Francisco: American Academy of Orthopedic Surgeons; 1997.
18. Marino J, Russo J, Kenny M, et al. Continuous lumbar plexus block for postoperative pain control after total hip arthroplasty. A randomized controlled trial. J Bone Joint Surg Am. 2009;91:29-37.
19. Robertson WJ, Kelly BT. The safe zone for hip arthroscopy: a cadaveric assessment of central, peripheral, and lateral compartment portal placement. Arthroscopy. 2008;24:1019-1026.
20. Ikeda T, Awaya G, Suzuki S, et al. Torn acetabular labrum in young patients. Arthroscopic diagnosis and management. J Bone Joint Surg Br. 1988;70:13-16.
21. McCarthy JC, Noble PC, Schuck MR, et al. The Otto E. Aufranc Award: the role of labral lesions to development of early degenerative hip disease. Clin Orthop Relat Res. 2001;393:25-37.
22. Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with 10-year follow-up. Arthroscopy. 2009;25:365-368.
23. Murphy KP, Ross AE, Javernick MA, Lehman RAJr. Repair of the adult acetabular labrum, .e1-.e3. Arthroscopy. 2006;22:567.
24. Griffin DR, Villar RN. Complications of arthroscopy of the hip. J Bone Joint Surg Br. 1999;81:604-606.
25. Hines SL, Philippon MJ, Kuppersmith D. Early clinical results in a group of patients undergoing hip labral repairs, Paper presented at Annual Arthroscopy Association of North America 2007.Annual Meeting; August-September 2007, San Francisco: Arthroscopy Association of North America; 2007.
26. Potter BK, Freedman BA, Andersen RC, et al. Correlation of Short Form-36 and disability status with outcomes of arthroscopic acetabular labral debridement. Am J Sports Med. 2005;33:864-870.
27. O’Leary JA, Berend K, Vail TP. The relationship between diagnosis and outcome in arthroscopy of the hip. Arthroscopy. 2001;17:181-188.
28. Santori N, Villar RN. Acetabular labral tears: result of arthroscopic partial limbectomy. Arthroscopy. 2000;16:11-15.
29. Byrd JW, Jones KS. Prospective analysis of hip arthroscopy with 2-year follow-up. Arthroscopy. 2000;16:578-587.
30. Farjo LA, Glick JM, Sampson TG. Hip arthroscopy for acetabular labral tears. Arthroscopy. 1999;15:132-137.