Chapter 18 Kyphoplasty
Indications
Kyphoplasty is performed in patients with recent vertebral fractures due to osteoporosis, angiomas, myelomas, metastasis, and so on, who present with pain refractory to conservative treatment including bed rest and drug treatment. The best results are obtained when the vertebral collapse has occurred recently—that is 3 months or less before the patient’s presentation [1,2].
Contraindications
Contraindications to kyphoplasty may be absolute or relative [1–3]. Absolute contraindications are as follows:
Complications
There is an overall incidence rate of complications with this procedure ranges from 0 to 9.8% [4–9]. The most common is cement extravasation, which may be avoided with the following precautions [10]:
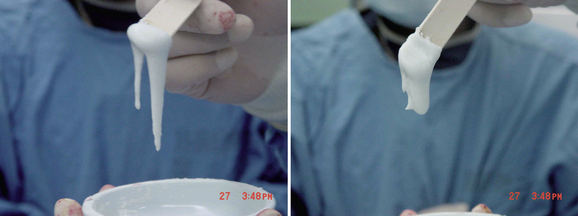
 Filling the void with thick, toothpaste-like cement using a low-pressure injection yields less cement leakage than filling the interstices of a fractured vertebra with thin, less viscous cement via a high-pressure injection, as is done in vertebroplasty.
Filling the void with thick, toothpaste-like cement using a low-pressure injection yields less cement leakage than filling the interstices of a fractured vertebra with thin, less viscous cement via a high-pressure injection, as is done in vertebroplasty. Adequate imaging with high-quality digital fluoroscopy, adequate cement opacification with sterile barium, and injection of cement which is not too liquefied can avoid leakage.
Adequate imaging with high-quality digital fluoroscopy, adequate cement opacification with sterile barium, and injection of cement which is not too liquefied can avoid leakage.Other, extremely rare complications of kyphoplasty are as follows:
Preoperative preparation
The imaging diagnosis would include the following:
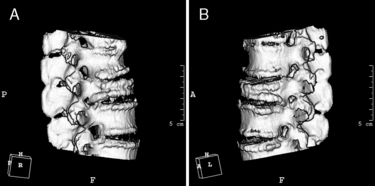
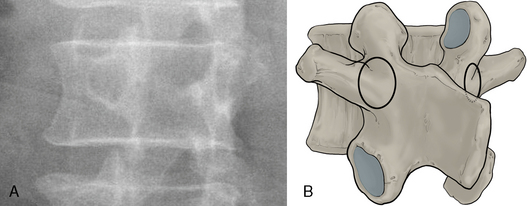
 Computed tomography (CT) scan with or without three-dimensional imaging to assess details of the bony architecture in cases of suspicion of a posterior cortical fracture (Fig. 18-1)
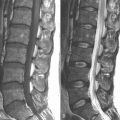
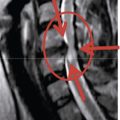
Computed tomography (CT) scan with or without three-dimensional imaging to assess details of the bony architecture in cases of suspicion of a posterior cortical fracture (Fig. 18-1) Magnetic resonance imaging (MRI) to detect signal change caused by bone edema at the level of a recent fracture (Fig. 18-2)
Magnetic resonance imaging (MRI) to detect signal change caused by bone edema at the level of a recent fracture (Fig. 18-2)Radiologic anatomy for kyphoplasty
Radiologic landmarks for kyphoplasty should be identified as follows (Fig. 18-3)
Methods of kyphoplasty
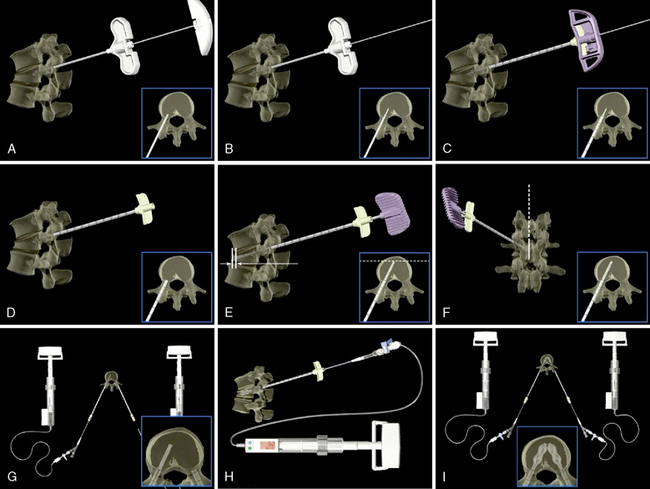
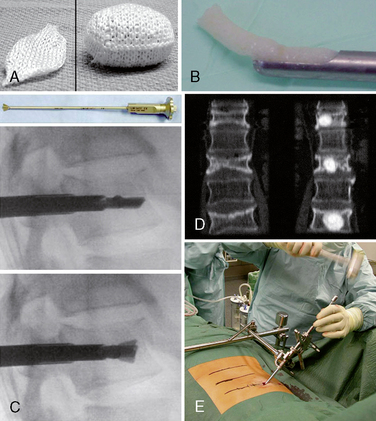
 Bone graft kyphoplasty: OptiMesh Deployable Grafting System (Spineology, Inc., St. Paul, MN) (Fig. 18-4)
Bone graft kyphoplasty: OptiMesh Deployable Grafting System (Spineology, Inc., St. Paul, MN) (Fig. 18-4)Instrumentation
Operating Room Setup
Figure 18-5 depicts the operating room setup for balloon kyphoplasty, consisting of the following:
Kyphoplasty Kit
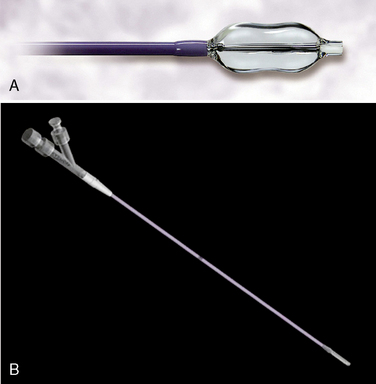
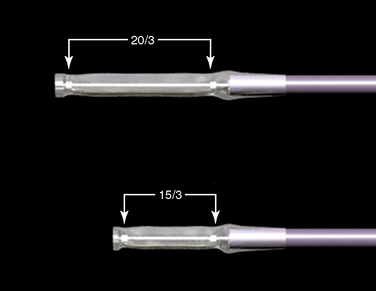
Figure 18-6 illustrates the components of the balloon kyphoplasty system manufactured by Medtronic, Sunnyvale, CA, use of which is described in the procedure section of this chapter:
 KYPHON® Inflation Syringe, which consists of a long tube to keep the clinician out of the radiation beam, an easy to read digital pressure gauge and volume scale, and provide safe, precise control of balloon inflation (Fig. 18-9)
KYPHON® Inflation Syringe, which consists of a long tube to keep the clinician out of the radiation beam, an easy to read digital pressure gauge and volume scale, and provide safe, precise control of balloon inflation (Fig. 18-9)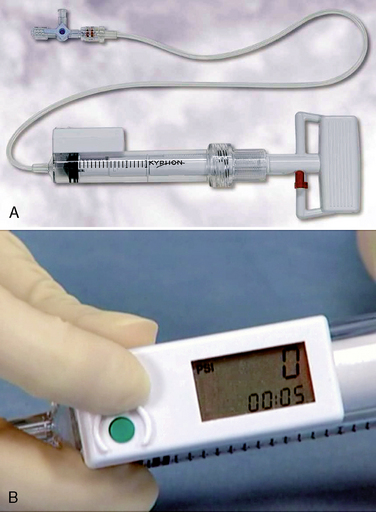
Figure 18–9 Inflation syringe with volume scale (A) The digital pressure gauge and time shown on monitor. (B)
(Courtesy of Kyphon, Inc., Sunnyvale, CA.)
Bone Cement
Use of bone cement for kyphoplasty is associated with following potential problems:
 A high exothermal polymerization temperature can lead to thermal necrosis of the soft tissues at the peri-augmentation site [12,13].
A high exothermal polymerization temperature can lead to thermal necrosis of the soft tissues at the peri-augmentation site [12,13]. Exposure to the fumes of the liquid monomer may cause idiosyncratic or asthmatic reactions and/or lacrimation [13].
Exposure to the fumes of the liquid monomer may cause idiosyncratic or asthmatic reactions and/or lacrimation [13].We use a bone cement mixture (CMW1, DePuy, Blackpool, UK) that consists of the following:
Procedure
Inserting the Tools into the Fractured Vertebral Body
The single posterolateral approach should be restricted for special cases in which a transpedicular or extrapedicular approach cannot be performed. This approach could promote leakage directly back via the epidural veins to the epidural venous plexus along the anterior aspect of the spinal canal as a result of needle placement in the center of the vertebra rather than in the anterior quarter. Also, this approach carries the possibility of transecting the segmental artery or even injuring the exiting nerve root, because the needle trajectory potentially endangers the nerve root and segmental artery [14].
Please refer to the chapter 19 for the unipedicular approach from pages 266 to 267.
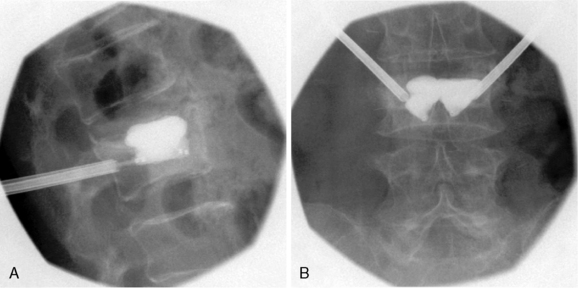
 Mid-pedicle level: When the bone access needle tip is presumed to be located at the midpoint of the pedicular diameter on the lateral view, its location on the AP view should be checked; here it should be central in the pedicle outline. If the tip is located too laterally, the lateral cortical wall of the pedicle may be damaged, and ballooning of the bone tamp may not be possible. If the tip is located too medially, the medial cortical wall of pedicle may be damaged, thereby leading to spinal canal violation (Fig. 18-15).
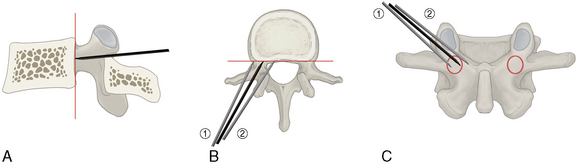
Mid-pedicle level: When the bone access needle tip is presumed to be located at the midpoint of the pedicular diameter on the lateral view, its location on the AP view should be checked; here it should be central in the pedicle outline. If the tip is located too laterally, the lateral cortical wall of the pedicle may be damaged, and ballooning of the bone tamp may not be possible. If the tip is located too medially, the medial cortical wall of pedicle may be damaged, thereby leading to spinal canal violation (Fig. 18-15). At the posterior vertebral cortical margin on the lateral view: If the bone access needle reaches the posterior vertebral cortical margin on the lateral view, it should be just inside the medial border of the pedicle outline on the AP view and then is advanced slightly into the vertebral body. If the needle is placed too laterally, it may damage the lateral cortical wall of the pedicle, and ballooning of the bone tamp may not be possible. If the needle is placed too medially, it may result in an accidental penetration of the medial cortical wall of pedicle, thereby leading to spinal canal violation (Fig. 18-16).
At the posterior vertebral cortical margin on the lateral view: If the bone access needle reaches the posterior vertebral cortical margin on the lateral view, it should be just inside the medial border of the pedicle outline on the AP view and then is advanced slightly into the vertebral body. If the needle is placed too laterally, it may damage the lateral cortical wall of the pedicle, and ballooning of the bone tamp may not be possible. If the needle is placed too medially, it may result in an accidental penetration of the medial cortical wall of pedicle, thereby leading to spinal canal violation (Fig. 18-16).Placing and Inflating the Bone Tamp
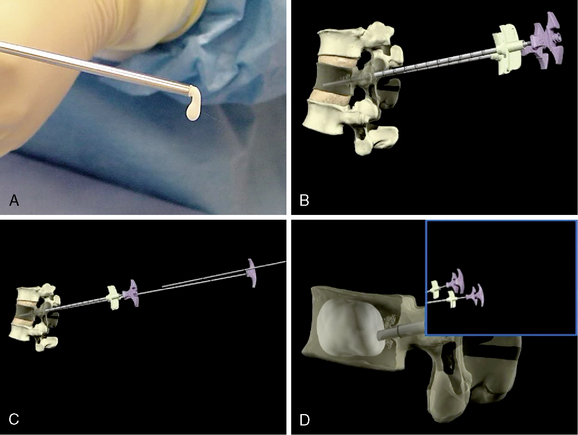
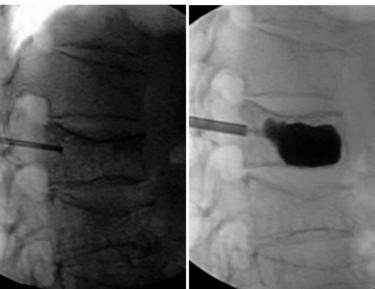
The bone tamp is placed (Fig. 18-18) and inflated (Fig. 18-19) as follows:
Mixing the Cement and Filling the Void
The factors influencing the cement hardening time included the following:
Table 18.1 Sample Hardening Times for Polymethylmethacrylate (PMMA) Formulations*
| Formulation | Time (min) |
|---|---|
| CMW1 original | 8-9 |
| CMW1 radiopaque | 8-9 |
| CMW2 | 4.5-5 |
| CMW3 | 8.5-9.5 |
* Products listed in table are CMW, manufactured by DePuy, Blackpool, UK.
Postoperative management
Potential adverse results
The potential adverse results of kyphoplasty are as follows:
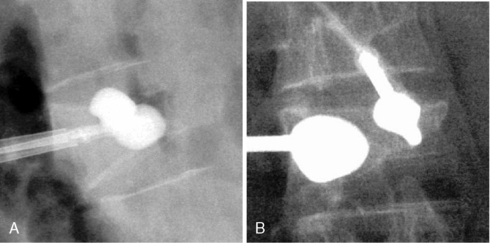
CASE STUDY 18.1
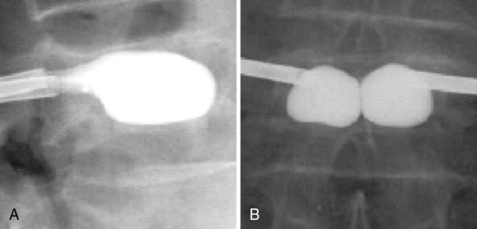
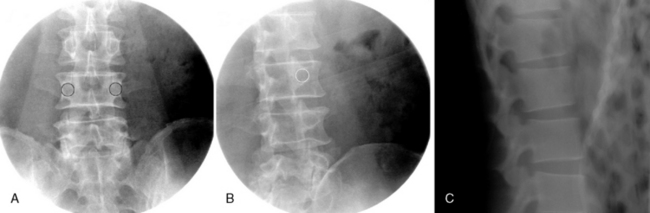
A 52-year-old man with multiple myeloma suffered from sudden lower back pain after a traumatic injury 1 month before his outpatient clinic visit. On physical examination, severe tenderness at the L1 level was noted. His initial pain intensity was 7 to 8 on a 10-cm visual analog scale (VAS). No neurologic abnormalities were found. Plain radiographs and a bone scan (Fig. 18-22) revealed an acute compression fracture at the L1 level. Morphine (10 mg PO bid), Celebrex (100 mg PO bid.) were prescribed, but this regimen achieved no significant pain relief.
A kyphoplasty using a bipedicular transpedicular approach was performed at the L1 level. Significant height restoration was noted (Fig. 18-23). The patient was discharged 2 hours after the procedure. One day after the procedure, his pain VAS score was 3 to 4.
1 Masala S., Fiori R., Massari F., et al. Kyphoplasty: Indications, contraindications and technique. Radiol Med. 2005;110:97-105.
2 Spivak J.M., Johnson M.G. Percutaneous treatment of vertebral body pathology. J Am Acad Orthop Surg. 2005;13:6-17.
3 Peh W.C.G., Gilula L.A., Peck D.D. Percutaneous vertebroplasty for severe osteoporotic vertebral body compression fractures. Radiology. 2002;223:121-126.
4 Coumans J.V., Reinhardt M.K., Lieberman I.H. Kyphoplasty for vertebral compression fractures: 1-year clinical outcomes from a prospective study. J Neurosurg Spine. 2003;99:44-50.
5 Dudeney S., Lieberman I.H., Reinhardt M.K., et al. Kyphoplasty in the treatment of osteolytic vertebral compression fractures as a result of multiple myeloma. J Clin Oncol. 2002;20:2382-2387.
6 Garfin S.R., Yuan H.A., Reiley M.A. New technologies in spine: Kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine. 2001;26:1511-1515.
7 Phillips F.M., Ho E., Campbell-Hupp M., et al. Early radiographic and clinical results of balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. Spine. 2003;28:2260-2267.
8 Theodorou D.J., Theodorou S.J., Duncan T.D., et al. Percutaneous balloon kyphoplasty for the correction of spinal deformity in painful vertebral body compression fractures. Clin Imaging. 2002;26:1-5.
9 Lieberman I.H., Dudeney S., Reinhardt M.K., et al. Initial outcome and efficacy of “kyphoplasty” in the treatment of painful osteoporotic vertebral compression fractures. Spine. 2001;26:1631-1638.
10 Phillips F.M., Wetzel T., Lieberman I., et al. An In vivo comparison of the potential for extravertebral cement leak after vertebroplasty and kyphoplasty. Spine. 2002;27:2173-2179.
11 Maynard A.S., Jensen M.E., Schweickert P.A., et al. Value of bone scan imaging in predicting pain relief from percutaneous vertebroplasty in osteoporotic vertebral fractures. AJNR Am J Neuroradiol. 2000;21:1807-1812.
12 Lewis G. Properties of acrylic bone cement: State of the art review. J Biomed Mater Res. 1997;38:155-182.
13 San Millan R.D., Burkhart K., Jean B., et al. Pathology findings with acrylic implants. Bone. 1999;23:855-905.
14 Wong W., Mathis J.M. Vertebroplasty and kyphoplasty: Techniques for avoiding complications and pitfalls. Neurosurg Focus. 2005;18:E2.











































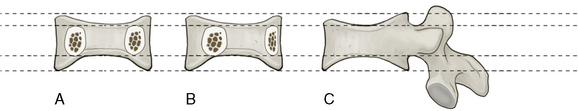
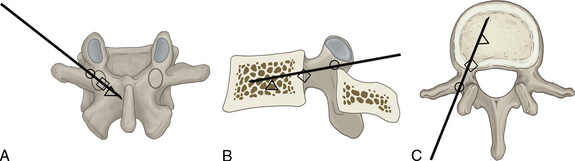
 , insertion point,
, insertion point,  , point at pedicle/vertebral body junction; Δ, mid-vertebral body; The needle tip should not pass medial to the medial border of the pedicle on the AP view until it is anterior to the posterior margin of the vertebral body on the lateral view. After penetration of the posterior margin of the vertebral body, the bone access needle is advanced only approximately 5 mm beyond this position. At that time, on the AP view, the tip should be located just medial to the medial border of the pedicle.
, point at pedicle/vertebral body junction; Δ, mid-vertebral body; The needle tip should not pass medial to the medial border of the pedicle on the AP view until it is anterior to the posterior margin of the vertebral body on the lateral view. After penetration of the posterior margin of the vertebral body, the bone access needle is advanced only approximately 5 mm beyond this position. At that time, on the AP view, the tip should be located just medial to the medial border of the pedicle.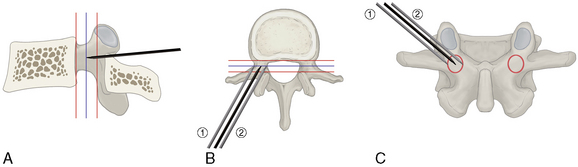
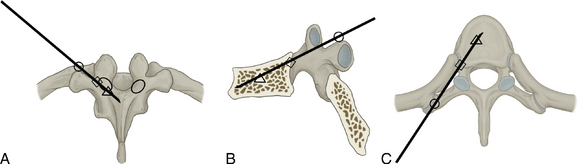
 , insertion point;
, insertion point;  , point at pedicle/vertebral body junction; Δ, mid-vertebral body;
, point at pedicle/vertebral body junction; Δ, mid-vertebral body;