Knee and lower leg
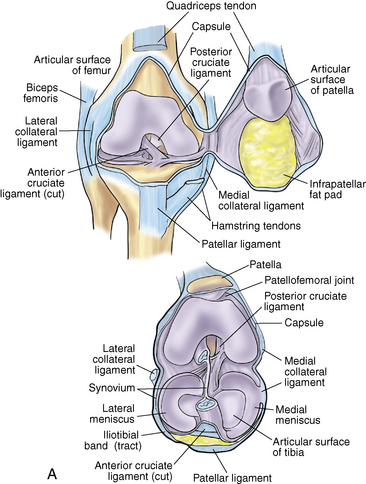
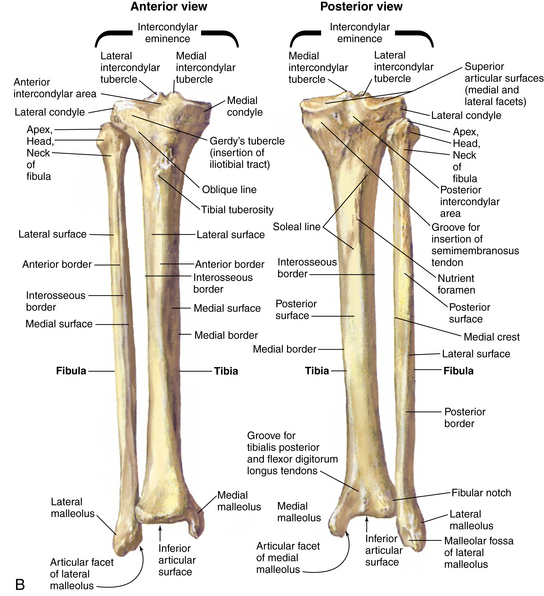
Anatomy
Ligaments: Table 7-1
Table 7-1.
Location and Function of Knee Ligaments
| LIGAMENT | LOCATION | FUNCTION |
| Anterior cruciate ligament (ACL) | Originates on the tibia just anterior to the area between the tibial eminences and runs obliquely to the lateral femoral condyle | Primary restraint to anterior translation of the tibia; also rotational stability |
| Posterior cruciate ligament (PCL) | Originates on lateral border of the medial femoral condyle and inserts on the posterior rim of the tibia | Primary restraint to posterior translation of the tibia |
| Medial collateral ligament (MCL) | Originates on the medial femoral epicondyle and inserts on the medial proximal tibia | Primary restraint to valgus force |
| Lateral collateral ligament (LCL) | Originates on the lateral femoral epicondyle and inserts on the anterolateral fibula | Primary restraint to varus stress |
| Posteromedial corner (PMC): posterior oblique ligament | Located deep and posterior to the MCL | Restraint to tibial internal rotation and valgus force |
| Posterolateral corner (PLC): biceps, iliotibial band, popliteus, popliteofibular ligament, and joint capsule | Located posterior to the LCL | Resistance to external rotation of the knee |
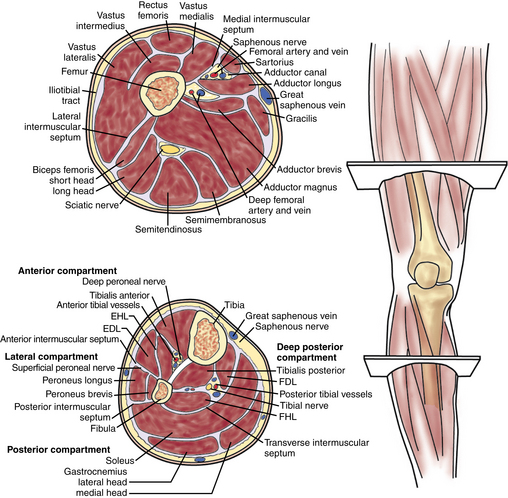
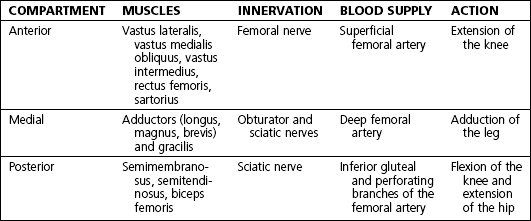
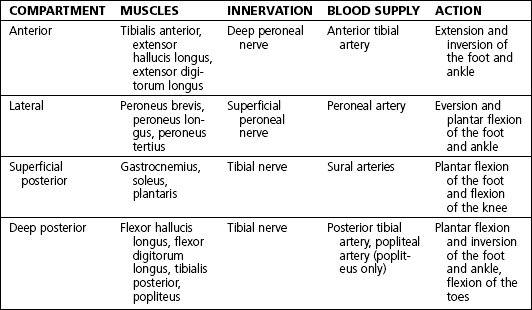
Muscles, nerves, and arteries: Figure 7-2 and tables 7-2 and 7-3
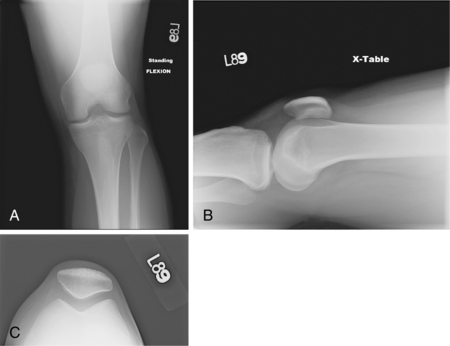
Normal radiographic appearance: Figures 7-3 and 7-4
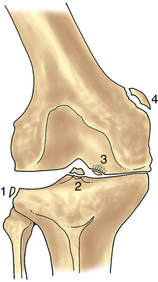
Figure 7-4. Illustration showing multiple radiographic findings. 1, Segond fracture (lateral capsular sign); 2, tibial eminence fracture; 3, osteochondritis dissecans; 4, Pellegrini-Stieda lesion. (From Miller MD, Hart JA, MacKnight JM, editors: Essential orthopaedics, Philadelphia, 2010, Saunders.)
Physical examination
Observe: gait (antalgic, assistive devices), alignment (valgus, varus), and feet (pes planus or cavus), ecchymosis, abrasion, gross deformity, effusion, quadriceps atrophy, and leg length discrepancy
Palpate: quadriceps muscle and tendon, patella (all poles, tendon, and fat pads), medial collateral ligament (MCL) and medial joint line, lateral collateral ligament (LCL) and lateral joint line, bursa (prepatellar and infrapatellar, pes anserine), and popliteal fossa
Normal range of motion (ROM): up to 10 degrees of hyperextension and 130 degrees of flexion
Neurovascular examination (Table 7-4): assessment of sensation and motor function of the foot; palpation of dorsalis pedis, posterior tibial, and popliteal pulses; test of patellar reflex
Table 7-4.
Lower Extremity Neurologic Examination
| NERVE | MOTOR FUNCTION | SENSORY DISTRIBUTION |
| Sural | Foot plantar flexion | Lateral heel |
| Saphenous | None | Medial leg and ankle |
| Superficial peroneal | Foot eversion | Dorsum of the foot |
| Deep peroneal | Great toe flexion | First web space |
| Tibial | Toe plantar flexion | Sole of the foot |
Special tests
 Patellar apprehension test: The patient lies supine with the knee in 20 to 30 degrees of flexion and the quadriceps relaxed. Carefully glide the patella laterally. A positive test result is the presence of a reactive contraction of the quadriceps muscles by the patient in an attempt to avoid a recurrence of the dislocation or a sense of apprehension or fear that the patella will dislocate.
Patellar apprehension test: The patient lies supine with the knee in 20 to 30 degrees of flexion and the quadriceps relaxed. Carefully glide the patella laterally. A positive test result is the presence of a reactive contraction of the quadriceps muscles by the patient in an attempt to avoid a recurrence of the dislocation or a sense of apprehension or fear that the patella will dislocate.
 Patellar grind test: The patient lies supine with knee fully extended. Push the patella distally in the trochlear groove. Have the patient tighten the quadriceps against patella resistance. Pain with or without crepitus is considered a positive test result.
Patellar grind test: The patient lies supine with knee fully extended. Push the patella distally in the trochlear groove. Have the patient tighten the quadriceps against patella resistance. Pain with or without crepitus is considered a positive test result.
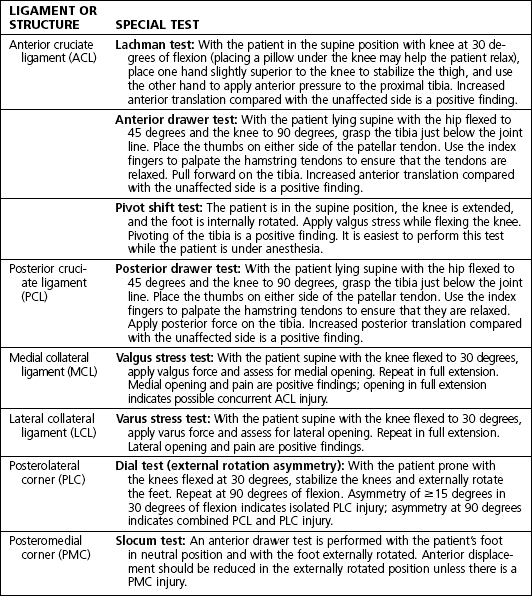
Ligament examination: Table 7-5 and figures 7-5 and 7-6

Figure 7-5. The Lachman examination. Note that the hand closest to the head of the patient grasps the thigh, and the opposite hand performs the examination with the thumb close to the joint line. A pillow can be placed under the knee to help the patient relax. (From Miller MD, Hart JA, MacKnight JM, editors: Essential orthopaedics, Philadelphia, 2010, Saunders.)

Figure 7-6. The posterior drawer examination. Note that the starting point is evaluated by palpating the medial tibial plateau in relation to the medial femoral condyle before a posteriorly directed force is applied. (From Miller MD, Hart JA, MacKnight JM, editors: Essential orthopaedics, Philadelphia, 2010, Saunders.)
Meniscal examination
 McMurray test: With patient supine, take hold of the heel with one hand and flex the leg. Place the free hand on the knee with fingers along the medial joint line and the thumb and thenar eminence on the lateral joint line. Apply valgus force, and externally rotate the lower leg, and then maintain valgus force while internally rotating. A palpable or audible click is considered a positive finding.
McMurray test: With patient supine, take hold of the heel with one hand and flex the leg. Place the free hand on the knee with fingers along the medial joint line and the thumb and thenar eminence on the lateral joint line. Apply valgus force, and externally rotate the lower leg, and then maintain valgus force while internally rotating. A palpable or audible click is considered a positive finding.
Differential diagnosis: Table 7-6
 The differential diagnosis for immediate effusion, in order of frequency, is as follows: anterior cruciate ligament (ACL) tear, patella dislocation, osteochondral fracture, and peripheral meniscus tear.
The differential diagnosis for immediate effusion, in order of frequency, is as follows: anterior cruciate ligament (ACL) tear, patella dislocation, osteochondral fracture, and peripheral meniscus tear.
Table 7-6.
Differential Diagnosis Based on Location of Knee Pain
| LOCATION | DIFFERENTIAL DIAGNOSES |
| Anterior | Patellofemoral chondromalacia, prepatellar bursitis, patellar tendinitis, patellar fracture, patellofemoral osteoarthritis |
| Medial | Meniscus tear, MCL injury, osteoarthritis, pes anserine bursitis |
| Lateral | Meniscus tear, LCL injury, osteoarthritis, iliotibial band syndrome |
| Posterior | Tear of posterior horn of medial or lateral meniscus, neurovascular injury (popliteal artery or nerve), PLC injury |
LCL, lateral collateral ligament; MCL, medial collateral ligament; PLC, posterolateral corner.
Anterior cruciate ligament injury
 The mechanism is typically a noncontact pivoting injury.
The mechanism is typically a noncontact pivoting injury.
 The patient often reports feeling or hearing a “pop” at the time of injury.
The patient often reports feeling or hearing a “pop” at the time of injury.
 The patient is typically unable to continue activity or complete a sporting event.
The patient is typically unable to continue activity or complete a sporting event.
 Instability with pivoting and swelling after activity are seen in chronic ACL tears.
Instability with pivoting and swelling after activity are seen in chronic ACL tears.
Physical examination
 Observation: Note effusion, abrasion, and deformity.
Observation: Note effusion, abrasion, and deformity.
 Palpation: Patellar ballottement is performed to assess for effusion. Joint line tenderness may be present secondary to concurrent meniscus tear.
Palpation: Patellar ballottement is performed to assess for effusion. Joint line tenderness may be present secondary to concurrent meniscus tear.
 ROM: Decreased ROM may result from effusion. The lack of ability to extend the knee fully may occur with a concurrent displaced bucket handle meniscus tear.
ROM: Decreased ROM may result from effusion. The lack of ability to extend the knee fully may occur with a concurrent displaced bucket handle meniscus tear.
Special tests
 Lachman, anterior drawer, and pivot shift tests
Lachman, anterior drawer, and pivot shift tests
 Posterior drawer test to evaluate for posterior cruciate ligament (PCL) injury
Posterior drawer test to evaluate for posterior cruciate ligament (PCL) injury
 McMurray test to evaluate for meniscus tear
McMurray test to evaluate for meniscus tear
 Dial test to evaluate for posterolateral corner (PLC) injury
Dial test to evaluate for posterolateral corner (PLC) injury
 Valgus and varus stress to evaluate the collateral ligaments
Valgus and varus stress to evaluate the collateral ligaments
 Patella apprehension and patella glide tests to evaluate for possible patella dislocation
Patella apprehension and patella glide tests to evaluate for possible patella dislocation
Imaging
• Obtain standing flexion, lateral, and sunrise views.
• Findings are often unremarkable; however, lateral tibial avulsion (Segond fracture) is highly suggestive of an ACL tear.
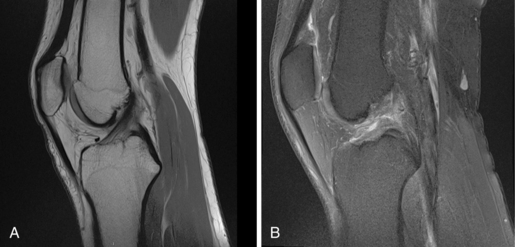
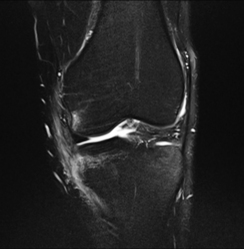
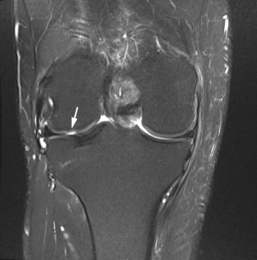
 Magnetic resonance imaging (MRI) of the knee without contrast (Fig. 7-7)
Magnetic resonance imaging (MRI) of the knee without contrast (Fig. 7-7)
Initial treatment
 Treatment options, as well as the risks and benefits of all options, should be thoroughly reviewed and discussed with the patient.
Treatment options, as well as the risks and benefits of all options, should be thoroughly reviewed and discussed with the patient.
 Graft selection for surgical reconstruction is made based on a variety of factors. In most cases, it is preferable to use a patient’s own tissue (autograft). Allograft (cadaveric tissue) is used when autograft is not available or to supplement inadequate autograft.
Graft selection for surgical reconstruction is made based on a variety of factors. In most cases, it is preferable to use a patient’s own tissue (autograft). Allograft (cadaveric tissue) is used when autograft is not available or to supplement inadequate autograft.
 The most common sources of autograft are the hamstring tendons (typically gracilis and semitendinosus) or a bone patella tendon bone (BPTB) graft (central third of the inferior patella, patella tendon, and a small portion of the tibial tuberosity).
The most common sources of autograft are the hamstring tendons (typically gracilis and semitendinosus) or a bone patella tendon bone (BPTB) graft (central third of the inferior patella, patella tendon, and a small portion of the tibial tuberosity).
Treatment options
 Conservative management may be appropriate for patients with a low activity level and less than 5 mm of laxity compared with the unaffected side.
Conservative management may be appropriate for patients with a low activity level and less than 5 mm of laxity compared with the unaffected side.
 Physical therapy (PT) for ROM and quadriceps strengthening is indicated.
Physical therapy (PT) for ROM and quadriceps strengthening is indicated.
 Without surgery, the patient may have recurrent instability and be at increased risk for meniscus tears and chondral injury or degeneration.
Without surgery, the patient may have recurrent instability and be at increased risk for meniscus tears and chondral injury or degeneration.
Operative management
Informed consent and counseling
 Possible complications include instrument breakage, aberrant tunnels, cartilage injury, hardware failure, loss of motion, residual laxity, paresthesia, effusion, deep vein thrombosis (DVT), and infection. Persistent anterior knee pain, patella tendon rupture, and patella fracture are potential complications if BPTB autograft is used.
Possible complications include instrument breakage, aberrant tunnels, cartilage injury, hardware failure, loss of motion, residual laxity, paresthesia, effusion, deep vein thrombosis (DVT), and infection. Persistent anterior knee pain, patella tendon rupture, and patella fracture are potential complications if BPTB autograft is used.
 Anesthesia risks include paralysis, cardiac arrest, brain damage, and death.
Anesthesia risks include paralysis, cardiac arrest, brain damage, and death.
 Postoperative PT is essential to regain motion and return to sports or physical activities.
Postoperative PT is essential to regain motion and return to sports or physical activities.
 Return to sports is usually not expected until 6 months postoperatively.
Return to sports is usually not expected until 6 months postoperatively.
Surgical procedures
Anterior cruciate ligament reconstruction:
 Prepare and drape the lower extremity in a sterile fashion.
Prepare and drape the lower extremity in a sterile fashion.
 Diagnostic arthroscopy is used to visualize the ACL and confirm injury, as well as to evaluate and treat meniscus tears, loose bodies, and chondral defects.
Diagnostic arthroscopy is used to visualize the ACL and confirm injury, as well as to evaluate and treat meniscus tears, loose bodies, and chondral defects.
 Graft harvesting: Techniques vary based on graft choice. A midline incision is made for BPTB graft, and a small oscillating saw is used to cut bone plugs from the patella and tibial tubercle. A medial vertical incision approximately 5 cm below the joint line is made for harvest of a hamstring graft. The semitendinosus and gracilis are identified and harvested with a tendon stripper.
Graft harvesting: Techniques vary based on graft choice. A midline incision is made for BPTB graft, and a small oscillating saw is used to cut bone plugs from the patella and tibial tubercle. A medial vertical incision approximately 5 cm below the joint line is made for harvest of a hamstring graft. The semitendinosus and gracilis are identified and harvested with a tendon stripper.
 Graft preparation: This varies based on the graft source. All grafts should be handled carefully and are prepared by a qualified assistant at area separate from the operative field.
Graft preparation: This varies based on the graft source. All grafts should be handled carefully and are prepared by a qualified assistant at area separate from the operative field.
 Débridement and notchplasty: Excess fibrous tissue and the ACL stump are débrided with a motorized shaver and bur to allow for better visualization of the back of the notch and to provide clearance for the graft.
Débridement and notchplasty: Excess fibrous tissue and the ACL stump are débrided with a motorized shaver and bur to allow for better visualization of the back of the notch and to provide clearance for the graft.
 Tunnel placement: The technique for tibial and femoral tunnel placement is determined by the surgeon’s preference. The goal is to recreate the normal anatomic position of the ACL.
Tunnel placement: The technique for tibial and femoral tunnel placement is determined by the surgeon’s preference. The goal is to recreate the normal anatomic position of the ACL.
 Graft passage: Sutures that are attached to both ends of the graft are passed through the tunnels.
Graft passage: Sutures that are attached to both ends of the graft are passed through the tunnels.
 Graft fixation: If BPTB graft is used, the graft is fixed with interference screws. For hamstring graft, an implant designed for soft tissue fixation is used.
Graft fixation: If BPTB graft is used, the graft is fixed with interference screws. For hamstring graft, an implant designed for soft tissue fixation is used.
 Wound closure: Multilayer closure is augmented with Steri-Strips; then a sterile dressing and an elastic compression (ACE) wrap are applied.
Wound closure: Multilayer closure is augmented with Steri-Strips; then a sterile dressing and an elastic compression (ACE) wrap are applied.
Estimated postoperative course
 Postoperative day 0 to 6 weeks
Postoperative day 0 to 6 weeks
• The patient may remove the wound dressing the second day after surgery and replace it with self-adhesive bandages, gauze, and an elastic compression (ACE) wrap.
• Ice, elevation, and pain medication as needed (PRN) are indicated for comfort.
• The patient uses a cane or crutches for the first few days for comfort.
• Begin PT on postoperative day 1 or 2. Early-stage PT focuses on ROM, edema control, scar management, isometric quadriceps strengthening, and normalization of gait.
• A wound check, suture removal, and assessment of ROM and stability are performed at 10 to 14 days postoperatively.
 Postoperative 6 weeks to 3 months
Postoperative 6 weeks to 3 months
• Obtain radiographs to assess tunnels and the position of the graft fixation device.
• Evaluate healing of the surgical site, ROM, and stability of reconstruction.
• Evaluate ROM and stability of reconstruction.
• The patient may begin straight ahead running at 3 months under the guidance of a physical therapist or a certified athletic trainer (ATC).
• The patient may return to sports at 6 months if able to pass functional testing with the ATC or the physical therapist.
Posterior cruciate ligament injury
 The mechanism of injury is typically a blow to the anterior tibia (i.e., dashboard injury) or a fall on a plantar flexed foot. Hyperextension or hyperflexion injuries also lead to PCL tear.
The mechanism of injury is typically a blow to the anterior tibia (i.e., dashboard injury) or a fall on a plantar flexed foot. Hyperextension or hyperflexion injuries also lead to PCL tear.
 Frank instability may or may not be present.
Frank instability may or may not be present.
 Anterior and medial knee pain may be reported in chronic injury.
Anterior and medial knee pain may be reported in chronic injury.
 Isolated PCL rupture is rare; it more commonly occurs in the multiligament knee injury.
Isolated PCL rupture is rare; it more commonly occurs in the multiligament knee injury.
Physical examination
 Observation: Note effusion, ecchymosis, abrasion, and obvious deformity.
Observation: Note effusion, ecchymosis, abrasion, and obvious deformity.
 Palpation: Patellar ballottement is performed to assess for effusion. Joint line tenderness may be present because of concurrent meniscus tear.
Palpation: Patellar ballottement is performed to assess for effusion. Joint line tenderness may be present because of concurrent meniscus tear.
Special tests: Figures 7-8 and 7-9
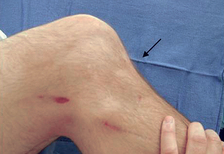
Figure 7-8. Positive posterior sag test. Note the position of the tibia (arrow). (From Miller MD, Hart JA, MacKnight JM, editors: Essential orthopaedics, Philadelphia, 2010, Saunders.)

Figure 7-9. External rotation asymmetry. With the knees stabilized, both feet are passively externally rotated and the thigh-foot angle is measured. Asymmetry of 15 degrees or more implies injury to the posterolateral corner structures. The test is performed in both 30 degrees (A) and 90 degrees (B) of knee flexion. Asymmetry in both 30 and 90 degrees implies injury to both the posterolateral corner and the posterior cruciate ligament. (From Miller MD, Hart JA, MacKnight JM, editors: Essential orthopaedics, Philadelphia, 2010, Saunders.)
 Posterior drawer test: See the classification section.
Posterior drawer test: See the classification section.
 Posterior sag test: With the knee and hip at 90 degrees of flexion, look for posterior sag of the tibia.
Posterior sag test: With the knee and hip at 90 degrees of flexion, look for posterior sag of the tibia.
 Dial test: This is used to assess the PLC.
Dial test: This is used to assess the PLC.
 Complete a thorough knee examination to rule out other ligamentous, meniscal, or patellar disorders.
Complete a thorough knee examination to rule out other ligamentous, meniscal, or patellar disorders.
Imaging
 Radiographs: Standing flexion, lateral, and sunrise views are often unremarkable, but they may show a PCL avulsion fragment. Stress views are obtained by applying posterior force to the proximal tibia with a Telos device.
Radiographs: Standing flexion, lateral, and sunrise views are often unremarkable, but they may show a PCL avulsion fragment. Stress views are obtained by applying posterior force to the proximal tibia with a Telos device.
 MRI: Imaging helps to identify the degree of injury (partial versus complete tear) and associated ligament, meniscus, and chondral injuries.
MRI: Imaging helps to identify the degree of injury (partial versus complete tear) and associated ligament, meniscus, and chondral injuries.
Classification
 Classification is based in the degree of posterior subluxation of the tibia in relation to the femoral condyles:
Classification is based in the degree of posterior subluxation of the tibia in relation to the femoral condyles:
Grade I: partial tear; posterior drawer demonstrating posterior tibial displacement that is anterior to the anterior aspect of the femoral condyles
Grade II: posterior drawer demonstrating posterior tibial displacement that is flush with the anterior aspect of the femoral condyles
Grade III: complete tear; posterior drawer demonstrating posterior tibial displacement posterior to the anterior aspect of the femoral condyles
Initial treatment
 Unlike the ACL, the PCL has some healing potential.
Unlike the ACL, the PCL has some healing potential.
 Not all PCL injuries require surgical reconstruction. Nonoperative management consists of intensive PT.
Not all PCL injuries require surgical reconstruction. Nonoperative management consists of intensive PT.
 Some research indicates an increased risk of developing degenerative changes in the PCL-deficient knee, especially in the patellofemoral compartment.
Some research indicates an increased risk of developing degenerative changes in the PCL-deficient knee, especially in the patellofemoral compartment.
Treatment options
Operative management
Informed consent and counseling
 Possible complications include residual laxity, instrument breakage, aberrant tunnels, avascular necrosis of the medial femoral condyle, cartilage injury, heterotopic ossification, hardware failure, loss of motion, neurovascular injury, paresthesia, effusion, DVT, and infection. Anesthesia risks include paralysis, cardiac arrest, brain damage, and death.
Possible complications include residual laxity, instrument breakage, aberrant tunnels, avascular necrosis of the medial femoral condyle, cartilage injury, heterotopic ossification, hardware failure, loss of motion, neurovascular injury, paresthesia, effusion, DVT, and infection. Anesthesia risks include paralysis, cardiac arrest, brain damage, and death.
 Postoperative PT is essential to regain full ROM, strengthen quadriceps, and return to sport or physical activities.
Postoperative PT is essential to regain full ROM, strengthen quadriceps, and return to sport or physical activities.
Surgical procedure: Figure 7-10
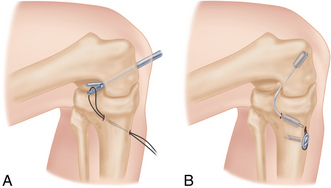
Figure 7-10. Posterior cruciate ligament reconstruction. A, The graft is passed from tibia to femur. B, Fixation is established with interference screws, and back-up fixation may be used if desired. (From Miller MD, Hart JA, editors: SMART: sports medicine assessment and review textbook, Philadelphia, 2011, Saunders.)
 Autograft (patellar tendon, quadriceps tendon, or hamstring tendons) or allograft (patellar tendon, quadriceps tendon, Achilles tendon, and hamstring tendons) may be used.
Autograft (patellar tendon, quadriceps tendon, or hamstring tendons) or allograft (patellar tendon, quadriceps tendon, Achilles tendon, and hamstring tendons) may be used.
Transtibial single-bundle technique:
 The extremity is prepared and draped in standard sterile fashion. The tibial tunnel is drilled at the anterolateral cortex of the proximal tibia. The knee is flexed to 110 degrees while the proximal tibia is pushed in posteriorly. A plastic sheath is placed in contact with the lateral femoral condyle, and then a femoral tunnel is created 2 to 3 mm proximal to the articular junction at the 1 o’clock position in the right knee or the 11 o’clock position in the left. A fixation device (chosen based on surgeon preference) is attached to the graft with a whipstitch. The graft is passed through both tunnels and secured with interference screws. The incisions are irrigated, then closed, and a sterile dressing is applied.
The extremity is prepared and draped in standard sterile fashion. The tibial tunnel is drilled at the anterolateral cortex of the proximal tibia. The knee is flexed to 110 degrees while the proximal tibia is pushed in posteriorly. A plastic sheath is placed in contact with the lateral femoral condyle, and then a femoral tunnel is created 2 to 3 mm proximal to the articular junction at the 1 o’clock position in the right knee or the 11 o’clock position in the left. A fixation device (chosen based on surgeon preference) is attached to the graft with a whipstitch. The graft is passed through both tunnels and secured with interference screws. The incisions are irrigated, then closed, and a sterile dressing is applied.
Arthroscopic tibial inlay technique (single- or double-bundle):
 The extremity is prepared and draped in standard sterile fashion. Anterolateral and anteromedial portals are established. Diagnostic arthroscopy is performed; meniscal and cartilage disorders are addressed. Next, a posteromedial portal is established for instrument passage. The PCL stump is débrided, while preserving the anterior edge of the PCL footprint to serve as a reference point for the inlay. The tibial tunnel is prepared with the knee in flexion. An arthroscopic PCL guide is used to position a pin in the proximal aspect of the PCL footprint. A flip cutter is used to create the tibial socket in an inside-out fashion. A C-arm and the arthroscope are used for guidance. The femoral tunnels are created using a PCL guide centered over the medial femoral condyle at the border of the vastus medialis. For single-bundle reconstruction, the femoral tunnel is drilled at the 11 o’clock position; for double-bundle reconstruction, tunnels are drilled at 9 o’clock and 11 o’clock positions. Grafts are passed with the knee flexed at 90 degrees. The grafts are fixed (various fixation devices are available). The incisions are irrigated, then closed, and a sterile dressing is applied.
The extremity is prepared and draped in standard sterile fashion. Anterolateral and anteromedial portals are established. Diagnostic arthroscopy is performed; meniscal and cartilage disorders are addressed. Next, a posteromedial portal is established for instrument passage. The PCL stump is débrided, while preserving the anterior edge of the PCL footprint to serve as a reference point for the inlay. The tibial tunnel is prepared with the knee in flexion. An arthroscopic PCL guide is used to position a pin in the proximal aspect of the PCL footprint. A flip cutter is used to create the tibial socket in an inside-out fashion. A C-arm and the arthroscope are used for guidance. The femoral tunnels are created using a PCL guide centered over the medial femoral condyle at the border of the vastus medialis. For single-bundle reconstruction, the femoral tunnel is drilled at the 11 o’clock position; for double-bundle reconstruction, tunnels are drilled at 9 o’clock and 11 o’clock positions. Grafts are passed with the knee flexed at 90 degrees. The grafts are fixed (various fixation devices are available). The incisions are irrigated, then closed, and a sterile dressing is applied.
Estimated postoperative course
 Postoperative day 0 to 6 weeks
Postoperative day 0 to 6 weeks
• Hinged brace locked in full extension at all times for 6 weeks. 50% weight bearing in brace with crutches to assist with ambulation, prone passive ROM with PT.
• Remove the dressing on the second day after surgery, and replace it with gauze or self-adhesive bandages and an elastic compression (ACE) wrap.
• Ice, elevation, and PRN pain medications are used for comfort.
• A wound check, suture removal, and assessment of ROM and stability are performed at 10 to 14 days postoperatively.
Medial collateral ligament injury
• The mechanism of injury is typically valgus stress to the knee. It can result from contact or noncontact injury.
• Medial knee pain is present.
• The patient is typically able to bear weight.
• The patient may report a sensation of instability with pivoting.
• Effusion may or may not be noted; localized swelling is more common.
Physical examination
 Observation: Note effusion, ecchymosis, deformity, abrasion or contusion, and gait.
Observation: Note effusion, ecchymosis, deformity, abrasion or contusion, and gait.
 Palpation: Palpate the entire course of the MCL, from proximal to distal. Tenderness typically indicates some degree of MCL injury. Joint line tenderness is indicative of concomitant meniscus tear. Lateral tenderness of the distal femur and proximal tibia may result from bony contusion.
Palpation: Palpate the entire course of the MCL, from proximal to distal. Tenderness typically indicates some degree of MCL injury. Joint line tenderness is indicative of concomitant meniscus tear. Lateral tenderness of the distal femur and proximal tibia may result from bony contusion.
Special tests: Figure 7-11

Figure 7-11. Varus stress testing. A varus stress is applied across the knee. This examination is done in both 30 degrees of knee flexion and full extension. Opening in full extension implies concurrent injury to the cruciate ligament. (From Miller MD, Hart JA, MacKnight JM, editors: Essential orthopaedics, Philadelphia, 2010, Saunders.)
 Valgus stress testing with the knee in 30 degrees of flexion isolates the MCL and is the most sensitive test.
Valgus stress testing with the knee in 30 degrees of flexion isolates the MCL and is the most sensitive test.
 Valgus stress testing should also be performed in full extension. Laxity in this position suggests grade III injury (complete rupture), as well as other ligamentous injury.
Valgus stress testing should also be performed in full extension. Laxity in this position suggests grade III injury (complete rupture), as well as other ligamentous injury.
 The Slocum test is used to evaluate for posteromedial corner (PMC) laxity.
The Slocum test is used to evaluate for posteromedial corner (PMC) laxity.
 Complete a through knee examination to rule out other ligamentous, meniscal, or patellar injury.
Complete a through knee examination to rule out other ligamentous, meniscal, or patellar injury.
Imaging
• Standing flexion, lateral, and sunrise views are typically normal in acute injury unless bony avulsion is present. Stress radiographs may be helpful.
• Pellegrini-Stieda lesion: MCL calcification is seen on plain radiographs in chronic MCL injury.
• MRI is not required to make the diagnosis, but it may be helpful to identify additional injuries.
• Coronal sequences are best for identifying MCL injury.
• Bone bruises of the lateral femoral condyle and lateral tibial plateau may be seen.
• MRI allows for grading: grade I, periligamentous swelling and minor tearing; grade II, complete disruption of superficial layers, deep layers intact; grade III, complete disruption and fluid extravasation.
Treatment options
 Playmaker brace: worn during weight-bearing activities until physical examination reveals pain-free motion and stability, typically for 6 to 8 weeks
Playmaker brace: worn during weight-bearing activities until physical examination reveals pain-free motion and stability, typically for 6 to 8 weeks
 Typical return to play: grade I, 10 days; grade II, 20 days; grade 3, at least 4 weeks (typically recommend the use of the brace with sports activities for an additional 6 weeks)
Typical return to play: grade I, 10 days; grade II, 20 days; grade 3, at least 4 weeks (typically recommend the use of the brace with sports activities for an additional 6 weeks)
Operative management
Informed consent and counseling
 Possible complications include loss of motion, bleeding, infection, DVT, neurovascular injury, residual laxity, instrument breakage, cartilage injury, hardware failure, and effusion. Anesthesia risks include cardiac arrest, paralysis, brain damage, and death.
Possible complications include loss of motion, bleeding, infection, DVT, neurovascular injury, residual laxity, instrument breakage, cartilage injury, hardware failure, and effusion. Anesthesia risks include cardiac arrest, paralysis, brain damage, and death.
 Postoperative PT is essential for full recovery and return to sports or physical activities.
Postoperative PT is essential for full recovery and return to sports or physical activities.
Surgical procedures
 A medial incision is made between the medial epicondyle and the adductor tubercle. Various suturing techniques are used to re-tension and repair the MCL and surrounding structures such as the posterior oblique ligament and semimembranosus. Suture, suture anchor, or screw with washer is used to repair MCL avulsions from the origin or insertion.
A medial incision is made between the medial epicondyle and the adductor tubercle. Various suturing techniques are used to re-tension and repair the MCL and surrounding structures such as the posterior oblique ligament and semimembranosus. Suture, suture anchor, or screw with washer is used to repair MCL avulsions from the origin or insertion.
 Wound closure: Multilayer closure is augmented with Steri-Strips; then a sterile dressing and an elastic compression (ACE) wrap are applied.
Wound closure: Multilayer closure is augmented with Steri-Strips; then a sterile dressing and an elastic compression (ACE) wrap are applied.
 Diagnostic arthroscopy is performed to evaluate and treat concurrent meniscus tear and to determine whether the MCL is torn from the femoral or tibial side.
Diagnostic arthroscopy is performed to evaluate and treat concurrent meniscus tear and to determine whether the MCL is torn from the femoral or tibial side.
 A 10- to 15-cm medial hockey stick incision is made. Primary repair is typically completed as described earlier and is then combined or reinforced with MCL reconstruction using semitendinosus autograft or allograft. The graft tissue is used to reconstruct the superficial MCL anatomically. The graft is secured at the anatomic origin and insertion with screws and washers or sutures. The posteromedial capsule can be secured to the graft to eliminate laxity.
A 10- to 15-cm medial hockey stick incision is made. Primary repair is typically completed as described earlier and is then combined or reinforced with MCL reconstruction using semitendinosus autograft or allograft. The graft tissue is used to reconstruct the superficial MCL anatomically. The graft is secured at the anatomic origin and insertion with screws and washers or sutures. The posteromedial capsule can be secured to the graft to eliminate laxity.
 Wound closure: Multilayer closure is augmented with Steri-Strips; then a sterile dressing and an elastic compression (ACE) wrap are applied
Wound closure: Multilayer closure is augmented with Steri-Strips; then a sterile dressing and an elastic compression (ACE) wrap are applied
Estimated postoperative course
 Postoperative day 0 to 6 weeks
Postoperative day 0 to 6 weeks
• An integrated ROM (IROM) brace locked in full extension is worn at all times for the first 2 weeks, then at 0 to 90 degrees for weeks 2 to 6. The patient has 50% weight bearing with crutches.
• The patient may remove the dressing on the second day after surgery and replace it with gauze or self-adhesive bandages and an elastic compression (ACE) wrap.
• Ice, elevation, and PRN pain medications are used for comfort.
• A wound check, suture removal, and assessment of ROM and stability are performed at 10 to 14 days postoperatively.
 Postoperative 6 weeks to 3 months
Postoperative 6 weeks to 3 months
• Full weight bearing is allowed as tolerated; the patient may be weaned off crutches. Discontinue the brace.
• Obtain radiographs, evaluate healing of the surgical site, and assess ROM and stability of reconstruction.
• PT: Advance to full ROM as soon as possible, facilitate gait normalization with treadmill walking, and continue quadriceps strengthening.
Knee dislocation
 The mechanism of injury is typically high-energy trauma such as a motor vehicle collision, but it can also occur in lower-velocity sports injuries. Knee dislocation can occur in obese patients with events that involve minimal trauma.
The mechanism of injury is typically high-energy trauma such as a motor vehicle collision, but it can also occur in lower-velocity sports injuries. Knee dislocation can occur in obese patients with events that involve minimal trauma.
 An obvious deformity may be present, but the knee may also spontaneously reduce before the patient seeks medical attention.
An obvious deformity may be present, but the knee may also spontaneously reduce before the patient seeks medical attention.
Physical examination
Special tests
 Compartment syndrome evaluation
Compartment syndrome evaluation
• Remember the six Ps: pain, pressure, paresthesia, pulselessness, pallor, and paralysis.
• Monitor compartment pressures.
• Consider checking serum creatine kinase and urine myoglobin levels.
• Serial examination must be performed.
• Dorsalis pedis and posterior tibial pulses should be symmetric bilaterally.
• Check the ankle-brachial index (ABI). An ABI greater than 0.9 is considered normal.
• An abnormal ABI is an indication for an arteriogram with venous runoff.
 Knee ligament examination (knee dislocation often causes multiligament injury)
Knee ligament examination (knee dislocation often causes multiligament injury)
Imaging
 Radiographs (Fig. 7-13): Anteroposterior (AP) and lateral views help to identify associated osseous injuries such as tibial plateau fracture, proximal fibular fracture, avulsion of Gerdy tubercle, intercondylar spine fracture, fibular head avulsion, and Segond or PCL avulsion fragments. Stress views will help assess degree of laxity resulting from ligamentous injury.
Radiographs (Fig. 7-13): Anteroposterior (AP) and lateral views help to identify associated osseous injuries such as tibial plateau fracture, proximal fibular fracture, avulsion of Gerdy tubercle, intercondylar spine fracture, fibular head avulsion, and Segond or PCL avulsion fragments. Stress views will help assess degree of laxity resulting from ligamentous injury.
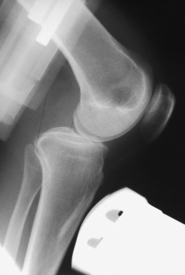
Figure 7-13. Stress radiograph demonstrating posterior translation secondary to posterior cruciate ligament rupture.
 MRI is not needed on an emergency basis, but it is helpful for identifying the extent of ligament injury and preparing for surgical reconstruction.
MRI is not needed on an emergency basis, but it is helpful for identifying the extent of ligament injury and preparing for surgical reconstruction.
 Arteriogram with venous runoff is used to assess for vascular injury.
Arteriogram with venous runoff is used to assess for vascular injury.
Classification
 Types of dislocations also defined by the direction of displacement of the tibia in respect to the femoral condyles: posterior, anterior, medial, lateral, and rotator (Fig. 7-14)
Types of dislocations also defined by the direction of displacement of the tibia in respect to the femoral condyles: posterior, anterior, medial, lateral, and rotator (Fig. 7-14)
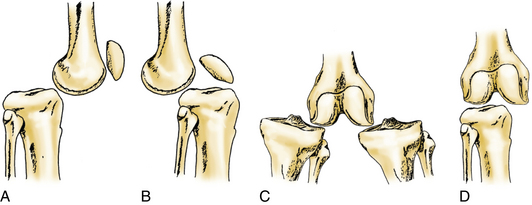
Figure 7-14. Descriptive classification system of knee joint dislocations. A, Posterior. B, Anterior. C, Medial or lateral. D, Rotatory. (From Bryant BJ, Musahl V, Harner CD: The dislocated knee. In Scott WN, editor: Insall and Scott surgery of the knee, ed 5, Philadelphia, 2012, Churchill Livingstone.)
Initial treatment
 Knee dislocation can result in multiligament injury.
Knee dislocation can result in multiligament injury.
 The peroneal nerve, which provides sensation to the dorsum of the foot and controls dorsiflexion of the ankle, is injured in up to 20% of knee dislocations.
The peroneal nerve, which provides sensation to the dorsum of the foot and controls dorsiflexion of the ankle, is injured in up to 20% of knee dislocations.
 Popliteal artery injury occurs in approximately 19% of knee dislocations.
Popliteal artery injury occurs in approximately 19% of knee dislocations.
 The long-term risk of posttraumatic arthritis is approximately 50%.
The long-term risk of posttraumatic arthritis is approximately 50%.
First treatment steps
 Closed reduction should be performed as soon as possible. Once the dislocation is reduced, repeat a neurovascular examination. Apply a long-leg splint or knee immobilizer; then repeat the radiographs to ensure that reduction is maintained.
Closed reduction should be performed as soon as possible. Once the dislocation is reduced, repeat a neurovascular examination. Apply a long-leg splint or knee immobilizer; then repeat the radiographs to ensure that reduction is maintained.
 Rapid identification and repair of vascular injuries are essential. Delay of 6 to 8 hours is associated with a high amputation rate.
Rapid identification and repair of vascular injuries are essential. Delay of 6 to 8 hours is associated with a high amputation rate.
Treatment options
Operative management
 Emergency surgery may be necessary if the dislocation is not reducible or evidence indicates vascular injury.
Emergency surgery may be necessary if the dislocation is not reducible or evidence indicates vascular injury.
 Surgical reconstruction will address multiligament injury. Timing often depends on the presence or absence of vascular injury. If vascular injury was previously repaired, consult a vascular surgeon for clearance before proceeding with ligament reconstruction.
Surgical reconstruction will address multiligament injury. Timing often depends on the presence or absence of vascular injury. If vascular injury was previously repaired, consult a vascular surgeon for clearance before proceeding with ligament reconstruction.
 If initial surgery must be delayed because of other more urgent injuries, the use of an external fixator may be necessary until definitive treatment with ligament reconstruction can be safely performed.
If initial surgery must be delayed because of other more urgent injuries, the use of an external fixator may be necessary until definitive treatment with ligament reconstruction can be safely performed.
 A combination of allograft and autograft is typically used for multiligament reconstruction.
A combination of allograft and autograft is typically used for multiligament reconstruction.
 Ligament reconstruction is performed as described in previous sections.
Ligament reconstruction is performed as described in previous sections.
 Later tendon transfer may be needed for patients with nerve injury.
Later tendon transfer may be needed for patients with nerve injury.
Estimated postoperative course
 Postoperative day 0 to 6 weeks
Postoperative day 0 to 6 weeks
• An IROM brace locked in full extension is worn at all times for the first 2 weeks and then at 0 to 90 degrees for weeks 2 to 6. The patient is 50% weight bearing with crutches for 6 weeks.
• Remove the dressing on the second day after surgery, and replace it with gauze or self-adhesive bandages and an elastic compression (ACE) wrap.
• Ice, elevation, and PRN pain medications are indicated.
• A wound check, suture removal, and assessment of ROM and stability are performed at 10 to 14 days postoperatively.
• PT: Straight leg raises with brace locked in extension, ROM exercises in the prone position, scar management, and modalities are used. The patient may begin using the stationary bike at 2 weeks.
Patella chondromalacia
 Patients complain of anterior knee pain that is aggravated by running, squatting, ascending or descending stairs, walking on inclines, sitting with the knee bent for a prolonged period, and rising from a seated position.
Patients complain of anterior knee pain that is aggravated by running, squatting, ascending or descending stairs, walking on inclines, sitting with the knee bent for a prolonged period, and rising from a seated position.
 Pain is typically described as “achy,” but it may be sharp at times.
Pain is typically described as “achy,” but it may be sharp at times.
 Patients may complain that the knee gives way. This pseudoinstability is the result of pain, which inhibits proper contraction of the quadriceps.
Patients may complain that the knee gives way. This pseudoinstability is the result of pain, which inhibits proper contraction of the quadriceps.
 “Popping” or “creaking” under the patella is a common complaint.
“Popping” or “creaking” under the patella is a common complaint.
 The patient may complain of “catching” under the patella (pseudolocking); however, true locking is not typical of patellofemoral chondromalacia. Locking is an indication of other disorders such as a meniscus tear.
The patient may complain of “catching” under the patella (pseudolocking); however, true locking is not typical of patellofemoral chondromalacia. Locking is an indication of other disorders such as a meniscus tear.
Physical examination
 Observation: Gait, body habitus, knee alignment (valgus/varus), foot pronation, pes planus/cavus, quadriceps atrophy, and effusion are noted.
Observation: Gait, body habitus, knee alignment (valgus/varus), foot pronation, pes planus/cavus, quadriceps atrophy, and effusion are noted.
 Palpation: Note patellar tenderness, tenderness of quadriceps or patellar tendon, tight lateral retinaculum, and crepitus.
Palpation: Note patellar tenderness, tenderness of quadriceps or patellar tendon, tight lateral retinaculum, and crepitus.
 ROM should be normal. There may be anterior knee pain with the upper range of flexion.
ROM should be normal. There may be anterior knee pain with the upper range of flexion.
Imaging
Initial treatment
 Patellofemoral pain can almost always be managed nonoperatively with activity modification, PT, and a home exercise program.
Patellofemoral pain can almost always be managed nonoperatively with activity modification, PT, and a home exercise program.
 It may take an extended period for symptoms to improve; compliance with PT and a home exercise program is essential for recovery.
It may take an extended period for symptoms to improve; compliance with PT and a home exercise program is essential for recovery.
 Patients should be counseled on the importance of obtaining or maintaining a healthy body weight.
Patients should be counseled on the importance of obtaining or maintaining a healthy body weight.
Treatment options
• Activity modification: Patients must avoid activity that causes pain. Runners must decrease distance and frequency. Those with severe pain may have to stop running and cross train on a stationary bike or elliptical machine during the rehabilitation period.
• NSAIDs: A short course (2 to 3 weeks) may help to decrease pain.
 PT for quadriceps strengthening with emphasis on the VMO, hip adductor strengthening, and stretching to increase quadriceps hamstring and iliotibial band (ITB) flexibility.
PT for quadriceps strengthening with emphasis on the VMO, hip adductor strengthening, and stretching to increase quadriceps hamstring and iliotibial band (ITB) flexibility.
 Other modalities such as ice, electrical stimulation, iontophoresis. and ultrasound may be beneficial.
Other modalities such as ice, electrical stimulation, iontophoresis. and ultrasound may be beneficial.
 Patellar taping or bracing is used.
Patellar taping or bracing is used.
 Custom orthotics may be used to address foot pronation and/or pes planus.
Custom orthotics may be used to address foot pronation and/or pes planus.
Surgical procedures
Arthroscopic débridement and chondroplasty:
 Two small incisions are made medial and lateral to the patella tendon slightly above the joint line. An arthroscope is used to explore the suprapatellar pouch, patellofemoral joint, intercondylar notch, medial and lateral compartments, and medial and lateral gutters. A shaver is used to débride the patella and other areas of cartilage fraying.
Two small incisions are made medial and lateral to the patella tendon slightly above the joint line. An arthroscope is used to explore the suprapatellar pouch, patellofemoral joint, intercondylar notch, medial and lateral compartments, and medial and lateral gutters. A shaver is used to débride the patella and other areas of cartilage fraying.
Estimated postoperative course
 Postoperative day 0 to 6 weeks
Postoperative day 0 to 6 weeks
• Full weight bearing is allowed as tolerated, and crutches or a cane may be used if needed.
• Ice, elevation, and PRN pain medications are indicated for comfort.
• Remove the dressing 2 days after surgery, and replace it with a self-adhesive bandage or gauze.
• Patients may begin using a stationary bicycle 2 to 3 days after surgery. Start with low resistance for short periods and advance as tolerated. Swimming and use of an elliptical trainer may be started 1 week after surgery.
• Sutures are removed 10 to 14 days after surgery.
• Formal PT is indicated in patients with decreased ROM, persistent effusion, or quadriceps atrophy.
Patella and quadriceps tendon disorders
• Typically, presentation is anterior knee pain at the superior (quadriceps) or inferior (patellar) poles of the patella.
• The patient often reports a gradual onset, but symptoms may be aggravated by increasing or changing workouts.
• This is most commonly seen in patients who participate in jumping, running, and kicking sports.
• Usually present after acute traumatic injury
• Inability to extend or lift the leg
• Possible history of knee pain or tendinitis before acute injury
• Possible history of steroid injection or anabolic steroid use
• Patella tendon ruptures more common in patients less than 40 years of age, whereas quadriceps tendon ruptures more common in patients more than 40 years of age
Physical examination
Tendon rupture
• Observation: effusion, ecchymosis
• Palpation: palpable defect at the site of rupture
• ROM: complete loss of active extension
• Quadriceps tendon rupture: no movement of the patella with contraction of the quadriceps
• Patella tendon rupture: movement of the patella with contraction of the quadriceps
Imaging: Figure 7-17
 Radiographs: AP, lateral, and sunrise views are used to rule out fracture (the patella may be “high” with patella tendon rupture and “low” with quadriceps tendon rupture).
Radiographs: AP, lateral, and sunrise views are used to rule out fracture (the patella may be “high” with patella tendon rupture and “low” with quadriceps tendon rupture).
 MRI is not typically needed to evaluate acute tendon rupture, but it may be helpful in chronic tendinitis to evaluate degree of tendinopathy and other disorders.
MRI is not typically needed to evaluate acute tendon rupture, but it may be helpful in chronic tendinitis to evaluate degree of tendinopathy and other disorders.
Treatment options
Operative management
Informed consent and counseling
 Potential risks include rerupture, extensor mechanism dysfunction, loss of motion, failure to restore normal patella height, bleeding, infection, wound complications, and DVT or PE.
Potential risks include rerupture, extensor mechanism dysfunction, loss of motion, failure to restore normal patella height, bleeding, infection, wound complications, and DVT or PE.
 Anesthesia risks include paralysis, cardiac arrest, brain damage, and death.
Anesthesia risks include paralysis, cardiac arrest, brain damage, and death.
 Postoperative PT is essential to regain function, strength, and to return to sports or physical activity.
Postoperative PT is essential to regain function, strength, and to return to sports or physical activity.
Surgical procedures
 The surgical site is prepared and draped in standard sterile fashion. A midline incision is made to expose the tendon. The diseased portion of the tendon is excised and débrided. A rongeur or small drill bit may be used on the patellar pole to create marrow stimulation and promote healing. The tendon, peritenon, and skin are closed in a multilayer fashion, and a sterile dressing is applied.
The surgical site is prepared and draped in standard sterile fashion. A midline incision is made to expose the tendon. The diseased portion of the tendon is excised and débrided. A rongeur or small drill bit may be used on the patellar pole to create marrow stimulation and promote healing. The tendon, peritenon, and skin are closed in a multilayer fashion, and a sterile dressing is applied.
• The surgical site is prepared and draped in standard sterile fashion. A midline incision is made to expose the patella and ruptured tendon. Degenerated or inflammatory tissue is débrided. The distal pole of patella is dissected with a curette and rongeur; #5 Ethibond sutures are woven into the patellar tendon. Three longitudinal holes are drilled from the distal pole to the proximal pole of the patella. Ethibond sutures are passed through the drill holes with a suture passer. Sutures are tied to complete an anatomic reconstruction. The wound is irrigated and closed in a multilayer fashion, and then a sterile dressing is applied.
• The surgical site is prepared and draped in standard sterile fashion. A midline incision is made to expose the patella and ruptured tendon. The superior pole of the patella is dissected using a curette and rongeur. Using #5 FiberWire, three stitches are placed into the quadriceps tendon. Four longitudinal tunnels are drilled through the patella, and sutures are passed through the tunnels. Anatomic reconstruction is completed by securing knots at the distal end of the patella. The wound is irrigated and closed in a multilayer fashion, and then a sterile dressing is applied.
Estimated postoperative course
 Postoperative day 0 to 6 weeks
Postoperative day 0 to 6 weeks
• A hinged knee brace locked in full extension is used for 4 weeks.
• The patient is allowed full weight bearing in a brace.
• Perform a wound check and suture removal at 10 to 14 days postoperatively.
Patella instability
 The patient may present with acute traumatic dislocation or with a complaint of chronic dislocation or subluxation.
The patient may present with acute traumatic dislocation or with a complaint of chronic dislocation or subluxation.
 Acute patellar dislocation is a common cause of hemarthrosis.
Acute patellar dislocation is a common cause of hemarthrosis.
 The patella may have to be manually reduced or may spontaneously reduce.
The patella may have to be manually reduced or may spontaneously reduce.
 Patients with chronic instability often report anterior knee pain and a sensation that the knee is “giving way” or “going out.”
Patients with chronic instability often report anterior knee pain and a sensation that the knee is “giving way” or “going out.”
Physical examination
 Observation: gait, lower extremity alignment, effusion
Observation: gait, lower extremity alignment, effusion
 Palpation: tenderness along the medial border of the patella
Palpation: tenderness along the medial border of the patella
Special tests
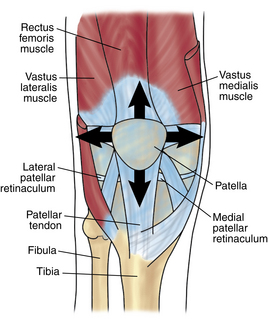
 J sign: The patella shifts laterally when the knee is extended (Fig. 7-18).
J sign: The patella shifts laterally when the knee is extended (Fig. 7-18).
 Q angle: The angle is formed from a line drawn from the anterior superior iliac spine to the center of the kneecap and from the center of the kneecap to the tibial tubercle. Measure that angle, and subtract from 180 degrees to determine Q angle.
Q angle: The angle is formed from a line drawn from the anterior superior iliac spine to the center of the kneecap and from the center of the kneecap to the tibial tubercle. Measure that angle, and subtract from 180 degrees to determine Q angle.
 Thorough knee examination to rule out ligamentous and meniscal injury
Thorough knee examination to rule out ligamentous and meniscal injury
Imaging
 Radiographs: Standing flexion, lateral and sunrise views may show trochlear dysplasia, patella alta subluxation or tilt of the patella, and degenerative changes.
Radiographs: Standing flexion, lateral and sunrise views may show trochlear dysplasia, patella alta subluxation or tilt of the patella, and degenerative changes.
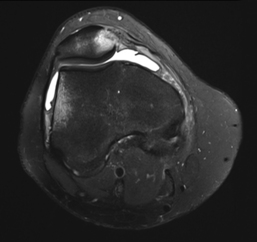
 MRI may show effusion, loose body, avulsion fracture, chondral injury, medial patellofemoral ligament (MPFL) tear, and subchondral edema (lateral femoral condyle and medial patella) (Fig. 7-19).
MRI may show effusion, loose body, avulsion fracture, chondral injury, medial patellofemoral ligament (MPFL) tear, and subchondral edema (lateral femoral condyle and medial patella) (Fig. 7-19).
Classification
 A classification system was developed by Dejour et al:
A classification system was developed by Dejour et al:
• Major patellar instability: more than one documented dislocation
• Objective patellar instability: one dislocation with associated anatomic abnormality
• Potential patellar instability: patellar pain with associated radiographic abnormalities
 Patellar instability is also classified as congenital, traumatic, obligatory, subluxation, or dislocation.
Patellar instability is also classified as congenital, traumatic, obligatory, subluxation, or dislocation.
Initial treatment
 The etiology of patellar instability is multifactorial. The following structural and functional factors can play a role in instability: patella alta, trochlear dysplasia or shallow groove, malalignment of the tibial tubercle, vastus medialis insufficiency, tight lateral structures, deficient MPFL, and joint laxity.
The etiology of patellar instability is multifactorial. The following structural and functional factors can play a role in instability: patella alta, trochlear dysplasia or shallow groove, malalignment of the tibial tubercle, vastus medialis insufficiency, tight lateral structures, deficient MPFL, and joint laxity.
Treatment options
 Crutches may be needed initially to assist with ambulation.
Crutches may be needed initially to assist with ambulation.
 Rest, ice, elevation, and NSAIDs are indicated.
Rest, ice, elevation, and NSAIDs are indicated.
 Limit activities that cause pain.
Limit activities that cause pain.
 Aspiration may be indicated for a large effusion that interferes with ROM.
Aspiration may be indicated for a large effusion that interferes with ROM.
 PT is indicated for quadriceps strengthening with emphasis on the vastus medialis, strengthening of the hip abductors and flexors, edema control, and ROM.
PT is indicated for quadriceps strengthening with emphasis on the vastus medialis, strengthening of the hip abductors and flexors, edema control, and ROM.
 Patella taping or a patella stabilizing brace may provide symptomatic relief.
Patella taping or a patella stabilizing brace may provide symptomatic relief.
 Weight loss is recommended to reduce the patellofemoral load.
Weight loss is recommended to reduce the patellofemoral load.
Surgical procedures
Proximal repair and realignment procedures:
 Primary repair of the MPFL: This procedure is indicated when instability is secondary to avulsion of the MPFL from the patellar or femoral attachment, rather than abnormal alignment. If the MPFL is disrupted at the patellar attachment, it is reattached to the patella with nonabsorbable sutures placed through drill holes in the patella. When the MPFL is torn from its femoral attachment, two suture anchors are placed into the femur at the MPFL origin, and mattress sutures are used to secure the MPFL.
Primary repair of the MPFL: This procedure is indicated when instability is secondary to avulsion of the MPFL from the patellar or femoral attachment, rather than abnormal alignment. If the MPFL is disrupted at the patellar attachment, it is reattached to the patella with nonabsorbable sutures placed through drill holes in the patella. When the MPFL is torn from its femoral attachment, two suture anchors are placed into the femur at the MPFL origin, and mattress sutures are used to secure the MPFL.
 Reconstruction of the MPFL: This procedure is indicated when the MPFL is deficient or attenuated. Soft tissue autograft or allograft (semitendinosus tendon) is used. The graft can be fixed to the patella with an EndoButton fixation device, interference screw, or biotenodesis screw. A screw and washer are used for femoral fixation.
Reconstruction of the MPFL: This procedure is indicated when the MPFL is deficient or attenuated. Soft tissue autograft or allograft (semitendinosus tendon) is used. The graft can be fixed to the patella with an EndoButton fixation device, interference screw, or biotenodesis screw. A screw and washer are used for femoral fixation.
 Lateral retinaculum release: This procedure is most often performed in combination with the previously mentioned medial stabilization techniques. Lateral release is indicated only for patients with a tight retinaculum leading to patellar tilt. The lateral retinaculum is released proximal to the patellar pole; the vastus lateralis is left intact to reduce medial patellar subluxation.
Lateral retinaculum release: This procedure is most often performed in combination with the previously mentioned medial stabilization techniques. Lateral release is indicated only for patients with a tight retinaculum leading to patellar tilt. The lateral retinaculum is released proximal to the patellar pole; the vastus lateralis is left intact to reduce medial patellar subluxation.
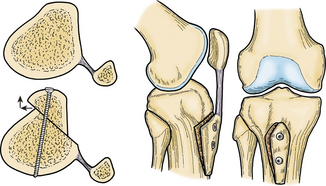
Anterior tibial tubercle transfer (fulkerson osteotomy): Figure 7-20:
 This procedure is indicated when the patella does not track properly because of an abnormal trochlea or high patella. The tibial tubercle is detached and then anteriorized, medialized, and secured with cortical screws. This procedure unloads the patellofemoral joint and corrects the Q angle.
This procedure is indicated when the patella does not track properly because of an abnormal trochlea or high patella. The tibial tubercle is detached and then anteriorized, medialized, and secured with cortical screws. This procedure unloads the patellofemoral joint and corrects the Q angle.
 Proximal and distal realignment procedures are often used in combination.
Proximal and distal realignment procedures are often used in combination.
Estimated postoperative course
 Postoperative day 0 to 6 weeks
Postoperative day 0 to 6 weeks
• Hinged brace locked in full extension
• Crutches and toe touch weight bearing for 2 weeks for MPFL reconstruction and 6 weeks for Fulkerson osteotomy
• Removal by the patient of the surgical dressing the third day after surgery and replacement with gauze or self-adhesive bandages.
• Wound check and suture removal 10 to 14 days postoperatively
Cartilage injuries
 These injuries may occur along with acute injury to ACL, meniscus, collateral ligaments or patella dislocation.
These injuries may occur along with acute injury to ACL, meniscus, collateral ligaments or patella dislocation.
 These injuries can occur secondary to high-energy trauma or dashboard injury when the patella is forced into the trochlea.
These injuries can occur secondary to high-energy trauma or dashboard injury when the patella is forced into the trochlea.
 Acute pain with or without effusion (possible hemarthrosis if subchondral bone is fractured) is noted.
Acute pain with or without effusion (possible hemarthrosis if subchondral bone is fractured) is noted.
 Pain is aggravated by weight bearing.
Pain is aggravated by weight bearing.
 Mechanical symptoms such as locking or catching may occur if there is a cartilage flap or loose body (cartilage displaced into the joint).
Mechanical symptoms such as locking or catching may occur if there is a cartilage flap or loose body (cartilage displaced into the joint).
 Osteochondritis dissecans (OCD) is a condition that typically affects the pediatric population. This condition is characterized by separation of an osteochondral fragment with or without articular cartilage involvement. It manifests with the foregoing symptoms. The origin appears to be idiopathic.
Osteochondritis dissecans (OCD) is a condition that typically affects the pediatric population. This condition is characterized by separation of an osteochondral fragment with or without articular cartilage involvement. It manifests with the foregoing symptoms. The origin appears to be idiopathic.
Physical examination
Imaging
Classification: Tables 7-7 to 7-9
Table 7-7.
Clanton and DeLee Classification System for Osteochondritis Dissecans Lesions
| Type I | Depressed chondral fracture |
| Type II | Fragment attached by osseous bridge |
| Type III | Detached nondisplaced fragment |
| Type IV | Displaced fragment |
Data from Clanton TO, DeLee JC: Osteochondritis dissecans. History, pathophysiology, and current treatment concepts, Clin Orthop Relat Res 167:50-64, 1982.
Table 7-8.
Outerbridge Arthroscopic Grading System
| Grade 0 | Normal cartilage |
| Grade I | Softening and swelling |
| Grade II | Partial thickness defect, fissures <1.5 cm diameter |
| Grade III | Fissures down to subchondral bone, diameter >1.5 cm |
| Grade IV | Exposed subchondral bone |
Data from Spahn G, Klinger HM, Hofmann GO: How valid is the arthroscopic diagnosis of cartilage lesions? Results od an opinion survey among highly experienced arthroscopic surgeons, Arch Orthop Trauma Surg 129:1117-1121, 2010.
Table 7-9.
International Cartilage Repair Society Grading System
| Grade 0 | Normal |
| Grade 1 | Nearly normal, superficial lesions |
| Grade 2 | Abnormal, lesions extend <50% of cartilage depth |
| Grade 3 | Severely abnormal, lesions extend >50% of cartilage depth |
| Grade 4 | Lesions extend to subchondral bone |
Data from Spahn G, Klinger HM, Hofmann GO: How valid is the arthroscopic diagnosis of cartilage lesions? Results od an opinion survey among highly experienced arthroscopic surgeons, Arch Orthop Trauma Surg 129:1117-1121, 2010.
Initial treatment
 Articular cartilage lesions have limited healing potential, and persistent defects may progress to secondary OA.
Articular cartilage lesions have limited healing potential, and persistent defects may progress to secondary OA.
 The goal of surgical intervention is to repair the defect or promote the formation of tissue with structure and durability similar to those of normal articular cartilage, thus leading to pain-free joint function.
The goal of surgical intervention is to repair the defect or promote the formation of tissue with structure and durability similar to those of normal articular cartilage, thus leading to pain-free joint function.
Treatment options
 Rest, ice, elevation, NSAIDs, and compression for symptom management
Rest, ice, elevation, NSAIDs, and compression for symptom management
 PT for quadriceps strengthening and to restore ROM
PT for quadriceps strengthening and to restore ROM
 An unloader brace possibly helpful if there is overloading in a single compartment
An unloader brace possibly helpful if there is overloading in a single compartment
 Surgical intervention possibly required if no response to conservative measures
Surgical intervention possibly required if no response to conservative measures
 Surgical options: arthroscopic chondroplasty and loose body removal, microfracture, cartilage transfer (autograft versus allograft)
Surgical options: arthroscopic chondroplasty and loose body removal, microfracture, cartilage transfer (autograft versus allograft)
Operative management
Informed consent and counseling
 Potential risks: bleeding, infection, wound complications, loss of motion, DVT or PE, and failure of the procedure to hold up over time
Potential risks: bleeding, infection, wound complications, loss of motion, DVT or PE, and failure of the procedure to hold up over time
 Anesthesia complications: paralysis, cardiac arrest, brain damage, and death
Anesthesia complications: paralysis, cardiac arrest, brain damage, and death
 Postoperative PT and compliance with weight-bearing restrictions essential for full recovery
Postoperative PT and compliance with weight-bearing restrictions essential for full recovery
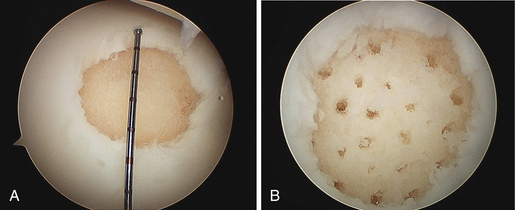
Surgical procedures
 Two small incisions are made medial and lateral to the patella tendon slightly above the joint line. An arthroscope is used to explore the suprapatellar pouch, patellofemoral joint, intercondylar notch, medial and lateral compartments, and medial and lateral gutters. A shaver is used to débride identified cartilage defects.
Two small incisions are made medial and lateral to the patella tendon slightly above the joint line. An arthroscope is used to explore the suprapatellar pouch, patellofemoral joint, intercondylar notch, medial and lateral compartments, and medial and lateral gutters. A shaver is used to débride identified cartilage defects.
Fixation of unstable fragments:
 This procedure can be performed if there is an osteochondral fragment and adequate subchondral bone. The defect is identified arthroscopically, and then underlying nonviable tissue is débrided with a shaver. Subchondral bone may be drilled or supplemented with bone graft, after which the osteochondral fragment is fixed with absorbable or nonabsorbable screws.
This procedure can be performed if there is an osteochondral fragment and adequate subchondral bone. The defect is identified arthroscopically, and then underlying nonviable tissue is débrided with a shaver. Subchondral bone may be drilled or supplemented with bone graft, after which the osteochondral fragment is fixed with absorbable or nonabsorbable screws.
 Two different techniques using osteochondral allograft exist. Very large defects can be “filled” using large osteochondral allograft plugs (“megaOATS”) that are cut to size and press fit into the defect. Minced juvenile allograft cartilage has also gained popularity to fill smaller defects and is particularly useful for patella defects, in which traditional OATS procedures have been difficult. The cartilage defect is débrided and filled with juvenile cartilage cells and is then sealed with fibrin glue. Hyaline cartilage fills the defect and functions similar to normal articular cartilage.
Two different techniques using osteochondral allograft exist. Very large defects can be “filled” using large osteochondral allograft plugs (“megaOATS”) that are cut to size and press fit into the defect. Minced juvenile allograft cartilage has also gained popularity to fill smaller defects and is particularly useful for patella defects, in which traditional OATS procedures have been difficult. The cartilage defect is débrided and filled with juvenile cartilage cells and is then sealed with fibrin glue. Hyaline cartilage fills the defect and functions similar to normal articular cartilage.
Estimated postoperative course
 Postoperative day 0 to 6 weeks
Postoperative day 0 to 6 weeks
• The surgical dressing can be removed on the second day after surgery and replaced with adhesive bandages or gauze.
• A wound check and suture removal are performed at 10 to 14 days postoperatively.
• Microfracture: Crutches and 25% weight bearing are indicated for 6 weeks. No limits on ROM are necessary; advance as tolerated.
• OATS: A brace and 50% weight bearing are indicated for 6 weeks.
• A continuous passive motion (CPM) machine may be ordered after microfracture or OATS.
• Ice, elevation, and PRN pain medication indicated for comfort.
• Begin PT at 10 to 14 days postoperatively.
• Arthroscopic débridement and chondroplasty: Only one postoperative visit is typically needed. The patient may bear weight and progress activity as tolerated.
Knee osteoarthritis
Imaging
• Standing flexion weight-bearing, AP lateral, and sunrise views are obtained. Bilateral films are often helpful for comparison.
• Common radiographic changes seen in OA include decreased joint space, osteophyte formation, subchondral sclerosis, cyst formation, and flattening of the femoral condyles (Fig. 7-23).
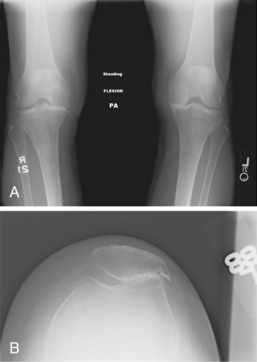
Figure 7-23. Radiographs demonstrating osteoarthritis (OA). A, Medial compartment OA. PA, posteroanterior. B, Patellofemoral OA.
• Full-length hip to ankle films are helpful to assess alignment if surgical intervention is indicated.
Treatment options
 Lifestyle modification includes low-impact exercise (stationary bicycle, elliptical trainer, swimming) and weight loss.
Lifestyle modification includes low-impact exercise (stationary bicycle, elliptical trainer, swimming) and weight loss.
 PT may help patients to develop an appropriate exercise routine.
PT may help patients to develop an appropriate exercise routine.
 Medications: Acetaminophen and NSAIDs are indicated. Narcotics are not recommended for long-term symptom management.
Medications: Acetaminophen and NSAIDs are indicated. Narcotics are not recommended for long-term symptom management.
 Dietary supplements: Glucosamine (1500 mg) and chondroitin sulfate (1200 mg) are recommended.
Dietary supplements: Glucosamine (1500 mg) and chondroitin sulfate (1200 mg) are recommended.
 Orthotics consist of a heel wedge and/or unloader brace (if OA is isolated to a single compartment).
Orthotics consist of a heel wedge and/or unloader brace (if OA is isolated to a single compartment).
 Intra-articular injections: Corticosteroid injections can be administered up to three times per year. Hyaluronic acid injections act as a lubricant, have few side effects, and may be helpful in patients in whom corticosteroid injection has failed.
Intra-articular injections: Corticosteroid injections can be administered up to three times per year. Hyaluronic acid injections act as a lubricant, have few side effects, and may be helpful in patients in whom corticosteroid injection has failed.