KNEE
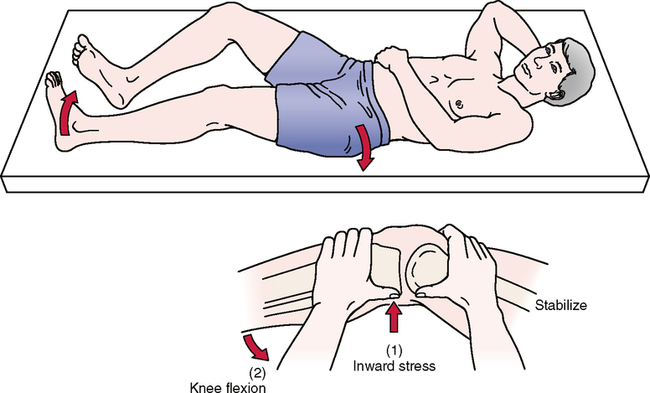
SPECIAL TESTS FOR ONE-PLANE MEDIAL INSTABILITY
Relevant Special Tests
Relevant Signs and Symptoms
• Mild to moderate knee pain is present.
• The patient reports feeling a tearing in the knee, not a “pop.”
• Bruising in the medial knee often is present, because the MCL/TCL is an extra-articular structure.
• Swelling builds up slowly over several days.
• The patient walks with a limp and has pain on knee extension, because extension stretches the ligament.
• Instability and “giving way” may be noted.
• Loss of knee motion and moderate stiffness may be present.
• Medial joint line pain or pain where the ligament attaches to the femur or tibia may be reported.
SPECIAL TESTS FOR ONE-PLANE LATERAL INSTABILITY
Relevant Special Tests
Epidemiology and Demographics
Injury to the LCL/FCL is the least common knee ligament injury. Injuries to the LCL/FCL are rare, accounting for only 2% of all knee injuries. The LCL/FCL is the least likely knee ligament to be sprained, because most LCL/FCL injuries are caused by a blow to the inside of the knee, and that area usually is shielded by the opposite leg.6,7,9–11
Relevant Signs and Symptoms
• Mild to moderate knee pain is present.
• The patient may report feeling a pop in the knee.
• Loss of knee motion and moderate stiffness are present.
• Lateral joint line pain may be reported.
• Bruising in the lateral knee often is present, because the LCL/FCL is an extra-articular structure.
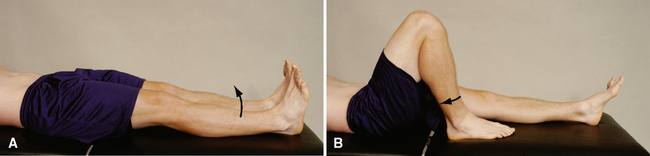
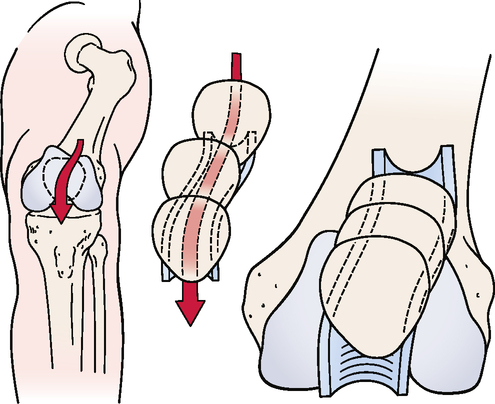
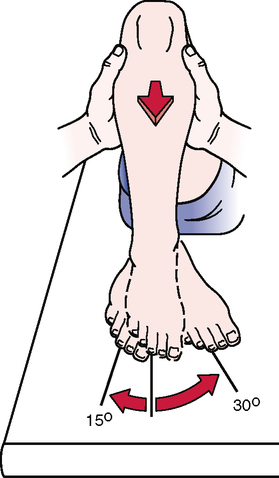
SPECIAL TESTS FOR ONE-PLANE POSTERIOR INSTABILITY
Relevant Special Tests
Posterior sag sign (gravity drawer test)
Drawer sign (see Special Tests for One-Plane Anterior Instability)
Active drawer test (see Special Tests for One-Plane Anterior Instability)
Relevant Signs and Symptoms
Mechanism of Injury
Hyperextension alone may lead to an avulsion injury of the PCL from the origin; this kind of injury may be amenable to repair. An anterior force to the anterior tibia in a hyperextended knee with the foot planted results in combined injury to the knee ligaments, along with knee dislocation.5–7,10,11,14–17
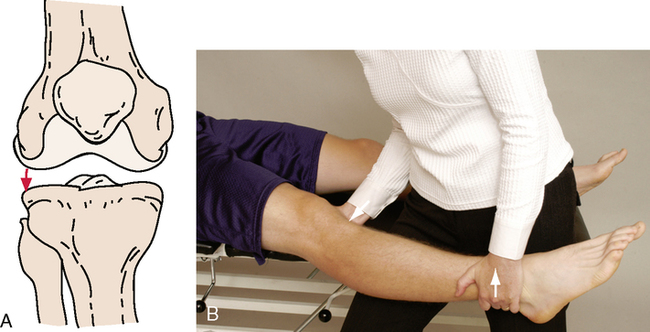
SPECIAL TESTS FOR ONE-PLANE ANTERIOR INSTABILITY
Relevant Special Tests