Key diagnostic features of additional soft tissue neoplasms
Images appear in the accompanying soft tissue atlas.
Angiomyofibroblastoma
• Most commonly located on the vulva
• Epithelioid (sometimes spindled) cells with a tendency to cluster near vessels
Angiomyofibroblastoma is a benign genital stromal tumor composed of clustered epithelioid to spindled cells in a myxoid to hyaline vascular stroma. Cellularity is somewhat variable. Tumor cells generally stain with desmin but are negative with actin and CD34. The differential diagnosis includes cellular angiofibroma.
Atypical vascular lesion (AVL)
• Well-circumscribed vessels, with minimal anastomosis, and a single layer of non-atypical appearing endothelial cells
Atypical vascular lesion is generally located on the breast and appears several years after irradiation. Clinically, the lesions are initially small purple-pink to red-brown multifocal papules that are well circumscribed histopathologically. While initially described as benign (acquired progressive lymphangioma or benign lymphangiomatous papules of the skin), many authors now consider these lesions to be potential precursors of angiosarcoma. Thus, close clinical follow-up or sometimes complete excision has been recommended. Amplification of MYC and FLT4 expression suggests a diagnosis of angiosarcoma rather than AVL.
Calcifying aponeurotic fibroma (juvenile aponeurotic fibroma)
• Nodular or infiltrative, variably cellular fibrous tissue
• Foci of calcification with variably chondroid metaplasia
• Stromal fibroblasts have round, plump nuclei and tend to have a linear or parallel arrangement, especially surrounding the calcifications
These tumors have a propensity for recurrence and a predilection for the palms and soles of children.
Carcinosarcoma (biphasic)
Carcinosarcoma is composed of two different malignant cell types: epithelial and mesenchymal spindle cells. Examples of carcinosarcoma in the skin include tumors with foci of basal cell carcinoma or squamous cell carcinoma intimately associated with a malignant spindle cell population that is negative with keratin stains. This spindle cell population sometimes has some resemblance to the cells of atypical fibroxanthoma. The differential diagnosis includes other malignant epithelial and spindle cell tumors, with the key to carcinosarcoma being recognition of the close admixture of two different malignant cell types.
Collagenous fibroma (desmoplastic fibroblastoma)
These tumors most commonly involve the subcutis of adults in a variety of sites, including arms, legs, back, hands, and feet. Typically, they are well-demarcated but can focally infiltrate surrounding tissue and vessels are inconspicuous, differentiating desmoplastic fibroblastoma from the more cellular fibromatosis. Mitoses are not a component. S100, CD34, and desmin are negative. Clonal abnormalities involving 11q12 have been reported.
Cutaneous myoepithelioma
• Epithelioid, spindled, plasmacytoid, or clear cells in nests, cords, or sheets
Myoepitheliomas are often considered in the spectrum with mixed tumor of the skin but lack ductal differentiation. Parachordomas belong to this spectrum but have more cytoplasmic vacuolations (physaliferous cells). Myoepithelioma has a propensity for the limbs of young adults. Expression of cytokeratin and/or EMA, as well as S100 is helpful in diagnosis. Calponin, SMA, and p63 may also be expressed. Malignant and benign tumors exist in this spectrum.
Extra-abdominal desmoid (extra-abdominal fibromatosis)
• Slender myofibroblastic/fibroblastic spindle cells separated by collagen and arranged in long, thin fascicles
Extra-abdominal desmoids originate from the fascia and connective tissue surrounding muscles, especially in the shoulder/pelvic girdle/thighs. Adolescents and young adults are most commonly affected. Although less common in children, extra-abdominal desmoids can present on the head/neck in this age group. Tumors can be multicentric and large and erode into bone or other nearby structures. Histologic findings include slender, elongated, bland spindle cells that are separated by collagen in long fascicles. Tumor cells may infiltrate surrounding structures, especially striated muscle. Tumor cell differentiation is fibroblastic/myofibroblastic, as suggested by positive staining with smooth muscle actin and muscle-specific actin and, rarely, desmin. Tumor cells are also positive with beta-catenin. The main differential diagnosis includes fibrosarcoma and reactive fibroblastic/myofibroblastic proliferations.
Giant cell tumor of the soft tissue
• Well circumscribed multi-nodular, usually subcutaneous tumor
• Mononuclear and osteoclastic giant cells
These lesions, seen most on the limb of adults, are the soft tissue counterpart of giant cell tumor of bone. They are also known as giant cell tumor of low malignant potential. Mitoses can be common but are typical figures. The mononuclear and osteoclastic giant cells are CD68 positive.
Intravascular fasciitis
• Variant of nodular fasciitis that involves the lumen and wall of a peripheral vessel, usually a vein
• Clefts focally separate the proliferation from the vessel wall
Intravascular fasciitis typical presents as a small, sometimes elongate, mass on the upper extremity or head and neck of young adults. While sometimes confused with vascular invasion of a malignancy, these lesions are benign and rarely recur. The histology is similar to nodular fasciitis consisting of fascicles of fibroblasts in a myxoid stroma with typical mitotic figures, and red blood cell extravasation. There may be a greater number of multinucleate giant cells and less prominent mucoid matrix.
Ischemic fasciitis (atypical decubital fibroplasia)
• Fibrinoid necrosis centrally surrounded by reactive atypical appearing, stellate or ganglion-like fibroblasts in a fibrotic to myxoid stroma
• Surrounded by a vascular proliferation (granulation tissue) in a zonal pattern
• Mitoses are frequent but not atypical and there is no hypercellularity
Ischemic fasciitis presents as a subcutaneous mass, typically without overlying ulceration, in an elderly and/or immobilized person. It overlies a bony prominence, such as the hip or shoulder.
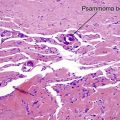
Liposarcoma
• Lipoblasts helpful (but not critical) to the diagnosis
• Simplest to divide liposarcoma into atypical lipomatous neoplasm/well-differentiated and dedifferentiated liposarcoma, myxoid liposarcoma, and pleomorphic liposarcomas
There are many types of liposarcoma, with a simplified classification outlined in Table 20a-1. Lipoblasts can aid in the diagnosis; characteristically they are spindled early on with fat located at the poles of the cell; in a middle stage, the nucleus is eccentric, hyperchromatic, and indented and the cytoplasm becomes rounded; ultimately the cell has striking resemblance to a mature adipocyte. The main differential diagnosis for atypical lipomatous neoplasm/well-differentiated liposarcoma is lipoma. The former is generally larger and based in the subcutis and stains with MDM2 and CDK4.
Low-grade fibromyxoid sarcoma (LGFMS)
• Abrupt transition from collagenous to myxoid areas
• Whorled or fascicular spindle cells
• Deceptively bland spindle cells and low mitotic rate
• Prominent vascularity with perivascular hypercellularity, especially in myxoid areas
LGFMS usually are deep seated tumors of adults in their thirties and forties that present on the proximal extremity or trunk. Hyalinizing spindle cell tumor with giant rosettes is a morphologic variant, where collagenous acellular central areas are cuffed by plump tumor cells. The majority of LGFMS are associated with t(7;16), fusing FUS and CREB3L2.
Metaplastic synovial cyst
This intradermal nodule usually occurs at the site of previous surgery or other trauma. This is a pseudocyst without true epithelial lining. Often inflamed granulation tissue or scar is present. Multinucleated giant cells and multiple normal mitotic figures may be noted.
Multinucleate cell angiohistiocytoma
This lesion is of uncertain histogenesis and may be reactive rather than neoplastic. Middle-aged to elderly women are most commonly affected with solitary or multiple grouped red-brown to violaceous asymptomatic papules to plaques on the dorsal hands, thighs and legs.
Myopericytoma
• Round to ovoid cells with amphophilic cytoplasm
• Concentric onion-skin like layers surrounding vascular channels
Myopericytomas occur most commonly in the dermis or subcutis of middle-aged adults on the distal lower extremity. This well circumscribed tumor is composed of myoid appearing cells in distinct concentric perivascular layers. Tumor cells express SMA, calponin, and caldesmon but only rarely and focally, desmin. Myopericytomas have overlapping features with myofibroma, glomus tumor, hemangiopericytoma and angioleiomyoma. The cells are larger than glomus cells with more cytoplasm.
Myxofibrosarcoma (myxoid malignant fibrous histiocytoma)
Myxofibrosarcoma classically is composed of relatively bland spindle cells in a prominent myxoid stroma. Occasionally, myxofibrosarcoma can have high-grade atypia. There are often intermixed curvilinear vessels. The differential diagnosis includes other tumors with myxoid stroma, including nodular fasciitis and low-grade fibromyxoid sarcoma.
Myxoinflammatory fibroblastic sarcoma
Myxoinflammatory fibroblastic sarcoma can resemble myxofibrosarcoma but is more inflamed. There is a mix of spindle cells, bizarre cells, and multivacuolated cells.
Nuchal-type fibroma (collagenosis nuchae)
Nuchal fibromas tend to occur as diffuse induration and swelling of the posterior neck in young to middle aged men but can occur at other locations including the shoulder, back, face or extremities where they are referred to as nuchal-type fibroma. There is an association with scleredema and diabetes. Histologically, the lesions are indistinguishable from the fibromas in Gardner’s syndrome. This syndrome should be considered when multiple lesions present during childhood. Desmoid fibromatosis can be confused with nuchal fibroma but desmoids are typically more cellular and prominently infiltrate the surrounding tissue.
Ossifying fibromyxoid tumor of soft parts
• Well circumscribed and lobular
• Cords or nests of small, round to polygonal cells embedded in fibromyxoid matrix
This lesion usually presents as a subcutaneous mass involving the extremity of a middle-aged adult. Widespread immunoreactivity for S100 protein is noted. Malignant cases are distinguished by high nuclear grade, high cellularity and mitotic rate of greater than two mitoses in 50 HPFs.
Pleomorphic hyalinizing angiectatic tumor of soft parts (PHAT)
• Non-encapsulated, infiltrative mass
• Hyalinized ectatic vessels and hyperchromatic spindle or pleomorphic cells, occasionally with nuclear pseudoinclusions
This soft tissue neoplasm is found in a wide age range (10–89 years, median 51), most commonly on the lower extremity. A myxoid matrix can be identified. While considered borderline lesions because of a 33–55% recurrence rate, they have a low mitotic index and have not been reported to metastasize. Immunohistochemically, PHAT is strongly positive for vimentin and CD34 but negative for S100, CD31, desmin, SMA, MSA, cytokeratin, and EMA. CD99 and VEGF reactivity has been reported.
Plexiform xanthomatous tumor
Plexiform xanthomatous tumor has a plexiform architecture with admixed epithelioid and xanthomatous cells. There may be cholesterol clefts or Touton giant cells. The cells are CD68-positive and -negative with S-100, CD34, and cytokeratins. The differential diagnosis includes plexiform fibrohistiocytic tumor.
Rhabdomyosarcoma
• Rhabdomyoblasts have cross-striations (sometimes subtle) and are helpful to the diagnosis when present
There are many subtypes (and different classifications) of rhabdomyosarcoma (see Table 20a-2), including embryonal/botryoid, alveolar, and pleomorphic. Different subtypes preferentially affect different age groups. Rhabdomyosarcoma is desmin positive and positive for other skeletal muscle markers like myogenin and MyoD1. The differential diagnosis varies depending on the subtype of rhabdomyosarcoma but includes other small blue tumors (e.g. neuroblastoma, synovial sarcoma).
Table 20a-2
| Subtype | Age of diagnosis | Histopathology |
| Embryonal | Average 7 | Primitive-appearing oval/round/spindle cells |
| Alternating cellular and myxoid zones | ||
| Rare rhabdomyoblasts | ||
| Botryoid | Average 7 | Polypoid shape |
| “Grenz zone” with increased cellularity below it | ||
| Primitive-appearing oval/round/spindle cells | ||
| Myxoid stroma | ||
| Rare rhabdomyoblasts | ||
| Alveolar | Average 16 | Poorly cohesive round to oval cells in “lumens” |
| “Lumens” lined by single layer of round/oval cells | ||
| Sometimes more solid growth pattern | ||
| Rare rhabdomyoblasts | ||
| Pleomorphic | Adults > 45 | Large, pleomorphic cells with eosinophilic cytoplasm |
Solitary fibrous tumor
• Patternless pattern of fascicles
• Hypo and hypercellular areas alternate separated by hyalinized collagen
Solitary fibrous tumor was initially described in the pleura but is seen in numerous other sites, including the soft tissue. There is not a clear correlation between morphology and behavior but the soft tissue tumors rarely metastasize. These lesions are diffusely positive for CD34, bcl-2, and CD99.
Synovial sarcoma
• Variable microscopic appearance, with a biphasic pattern (mixed epithelial and spindle cells) being most common
The diagnosis of synovial sarcoma can be challenging because of diverse microscopic findings. Tumors can be biphasic (like carcinosarcoma, with intimate admixture of epithelial cells and spindle cells) or monophasic, with epithelial or fibrous cells predominating, or poorly-differentiated. Molecular genetic abnormalities [t(X;18)(p11;q11)] and immunohistochemical staining patterns (cytokeratin and epithelial membrane antigen positive, TLE1 positive) link these heterogeneous tumor types.
Bhawan, J, Dayal, Y, González-Serva, A, et al. Cutaneous metaplastic synovial cyst. J Cutan Pathol. 1990; 17(1):22–26.
Choonhakarn, C, Tang, S. Cutaneous metaplastic synovial cyst. J Dermatol. 2003; 30(6):480–484.
Erdag, G, Qureshi, HS, Patterson, JW, et al. Solitary fibrous tumors of the skin: a clinicopathologic study of 10 cases and review of the literature. J Cutan Pathol. 2007; 34(11):844–850.
Evans, HL. Low-grade fibromyxoid sarcoma: a clinicopathologic study of 33 cases with long-term follow-up. Am J Surg Pathol. 2011; 35(10):1450–1462.
Folpe, AL, Morris, RJ, Weiss, SW. Soft tissue giant cell tumor of low malignant potential: a proposal for the reclassification of malignant giant cell tumor of soft parts. Mod Pathol. 1999; 12(9):894–902.
Graham, RP, Dry, S, Li, X, et al. Ossifying fibromyxoid tumor of soft parts: a clinicopathologic, proteomic, and genomic study. Am J Surg Pathol. 2011; 35(11):1615–1625.
Hornick, JL, Fletcher, CD. Cutaneous myoepithelioma: a clinicopathologic and immunohistochemical study of 14 cases. Hum Pathol. 2004; 35(1):14–24.
Ke, Q, Erbolat, Zhang, HY, et al. Clinicopathologic features of pleomorphic hyalinizing angiectatic tumor of soft parts. Chin Med J (Engl). 2007; 120(10):876–881.
Mentzel, T, Dei Tos, AP, Sapi, Z, et al. Myopericytoma of skin and soft tissues: clinicopathologic and immunohistochemical study of 54 cases. Am J Surg Pathol. 2006; 30(1):104–113.
Miettinen, M, Fetsch, JF. Collagenous fibroma (desmoplastic fibroblastoma): a clinicopathologic analysis of 63 cases of a distinctive soft tissue lesion with stellate-shaped fibroblasts. Hum Pathol. 1998; 29(7):676–682.
Patchefsky, AS, Enzinger, FM. Intravascular fasciitis: a report of 17 cases. Am J Surg Pathol. 1981; 5(1):29–36.
Pérez, LP, Zulaica, A, Rodríguez, L, et al. Multinucleate cell angiohistiocytoma. Report of five cases. J Cutan Pathol. 2006; 33(5):349–352.
Smith, ME, Fisher, C, Weiss, SW. Pleomorphic hyalinizing angiectatic tumor of soft parts. A low-grade neoplasm resembling neurilemoma. Am J Surg Pathol. 1996; 20(1):21–29.
Smolle, J, Auboeck, L, Gogg-Retzer, I, et al. Multinucleate cell angiohistiocytoma: a clinicopathological, immunohistochemical and ultrastructural study. Br J Dermatol. 1989; 121(1):113–121.
Zamecnik, M, Michal, M. Nuchal-type fibroma is positive for CD34 and CD99. Am J Surg Pathol. 2001; 25(7):970.