Chapter 1 Key Concepts
Please go to expertconsult.com for supplemental chapter material.
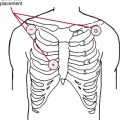
The device used to obtain and display the conventional ECG is called the electrocardiograph, or ECG machine. It records cardiac electrical currents (voltages or potentials) by means of conductive electrodes selectively positioned on the surface of the body.∗
Essential Cardiac Electrophysiology
Electrical Activation of the Heart
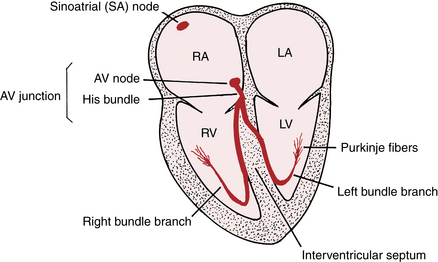
In simplest terms, therefore, the heart can be thought of as an electrically timed pump. The electrical “wiring” is outlined in Figure 1-1.
The AV junction, which acts as an electrical “relay” connecting the atria and ventricles, is located at the base of the interatrial septum and extends into the interventricular septum (see Fig. 1-1).
The lower (distal) part of the AV junction is called the bundle of His. The bundle of His then divides into two main branches: the right bundle branch, which distributes the stimulus to the right ventricle, and the left bundle branch,† which distributes the stimulus to the left ventricle (see Fig. 1-1).
The His bundle, its branches, and their subdivisions are referred to collectively as His-Purkinje system. Normally, the AV node and His-Purkinje system form the only electrical connection between the atria and the ventricles (unless a bypass tract is present; see Chapter 12). Disruption of conduction over these structures will produce AV heart block (Chapter 17).
Cardiac Automaticity and Conductivity: “Clocks and Cables”
Normally, the relatively more rapid intrinsic rate of SA node firing suppresses the automaticity of these secondary (ectopic) pacemakers outside the sinus node. However, sometimes, their automaticity may be abnormally increased, resulting in competition with the sinus node for control of the heartbeat. For example, a rapid run of ectopic atrial beats results in atrial tachycardias (Chapter 14). A rapid run of ectopic ventricular beats results in ventricular tachycardia (Chapter 16), a potentially life-threatening arrhythmia.
If you understand the normal physiologic stimulation of the heart, you have the basis for understanding the abnormalities of heart rhythm and conduction and their distinctive ECG patterns. For example, failure of the sinus node to effectively stimulate the atria can occur because of a failure of SA automaticity or because of local conduction block that prevents the stimulus from exiting the sinus node. Either pathophysiologic mechanism can result in apparent sinus node dysfunction and sometimes symptomatic sick sinus syndrome (Chapter 20). These patients may experience lightheadedness or even syncope (fainting) because of marked bradycardia (slow heartbeat).
Blockage of the spread of stimuli through the AV node or infranodal pathways can produce various degrees of AV heart block (Chapter 17), sometimes with severe, symptomatic ventricular bradycardia, necessitating placement of a temporary or permanent placement pacemaker.
Disease of the bundle branches, themselves, can produce right or left bundle branch block (resulting in electrical dyssynchrony, an important contributing mechanism in many cases of heart failure; see Chapters 7 and 21).
Preview: Looking Ahead
The first part of this book is devoted to explaining the basis of the normal ECG and then examining the major conditions that cause abnormal depolarization (P and QRS) and repolarization (ST-T and U) patterns. This alphabet of ECG terms is defined in Chapter 2.
Concluding Notes: Why is the ECG So Clinically Useful?
• It is the essential initial clinical test for diagnosing dangerous cardiac electrical disturbances related to conduction abnormalities in the AV junction and bundle branch system and to brady- and tachyarrhythmias.
• It often provides immediately available information about clinically important mechanical and metabolic problems, not just about primary abnormalities of electrical function. Examples include myocardial ischemia/infarction, electrolyte disorders, and drug toxicity, as well as hypertrophy and other types of chamber overload.
• It may provide clues that allow you to forecast preventable catastrophies. A good example is a very long QT(U) pattern preceding sudden cardiac arrest due to torsades de pointes.
∗ As discussed in Chapter 3, the ECG “leads” actually record the differences in potential among these electrodes.
† The left bundle branch has two major subdivisions called fascicles. (These small bundles are discussed in Chapter 7 along with the fascicular blocks or hemiblocks.)