119
Keratoacanthoma

Keratoacanthomas begin as a smooth, dome-shaped, red papule. Lesions grow rapidly.

Keratoacanthomas develop and grow rapidly, forming a keratin-filled necrotic crater.
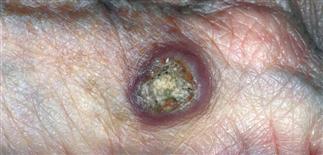
This lesion resembles both a keratoacanthoma and a squamous cell cancer, which is typical of advancing keratoacanthomas. It is best to treat this lesion as a squamous cell carcinoma.

Keratoacanthomas are dome-shaped tumors with a central crateriform crust that grows rapidly. Typical locations include the face, neck, hands and sun-exposed extremities.
DESCRIPTION
Rapidly growing crateriform nodule with distinctive clinical appearance. Best considered as a low-grade squamous cell carcinoma.
HISTORY
• The peak incidence of keratoacanthoma is between ages 50 and 70. This tumor is rare before 40 years of age. • White people with fair complexions are more often affected. • Typical locations include the face, neck, dorsal hands, and sun-exposed extremities. It occurs on the legs more often in women. • The lesion erupts rapidly and is often quite tender. • Chemical exposure and human papillomavirus have been implicated as a cause in animal models, although their role in humans is controversial. • Historically, keratoacanthomas have been regarded as benign regressing lesions; however, they should be thought of as variants of squamous cell carcinoma and treated as such.
PHYSICAL FINDINGS
A keratoacanthoma is a characteristic, solitary, flesh-colored to red, 0.5- to 2.0-cm, crateriform nodule. A central keratotic plug or depression conceals a deep keratinous cavity. This plug or depression gives the nodule its characteristic volcano-like shape. The nodule is firm in texture, tender to palpation or pressure, and can grow rapidly. Keratoacanthoma nearly always appears on sun-damaged skin. Three growth phases are described. • Proliferative phase: a solitary papule appears suddenly and then rapidly grows to its maximum size over 2–4 weeks. • Mature phase: the lesion is stable in size and appearance for weeks to months; it may appear crateriform if the core has been partially removed. • Resolving phase: the base becomes indurated, the central core is expelled, and the base resorbs, leaving a pitted scar over several months.
Rare cases of multiple keratoacanthomas have been reported, both as an eruptive (Grzybowski) form and as a familial adolescent (Ferguson–Smith) form. Patients with Muir–Torre syndrome develop sebaceous adenomas, at times with keratoacanthoma architecture. Such patients should be evaluated for occult gastrointestinal malignancy.
Patients on immunosuppressive therapy after organ transplant are at increased risk of developing keratoacanthomas and invasive squamous cell carcinoma. Examination for enlarged lymph nodes should always be performed in this patient population.
TREATMENT
• Best to presume a diagnosis of squamous cell carcinoma pending biopsy results and clinical follow-up. • An excisional biopsy or shave removal should be performed. It is important to biopsy deep enough to evaluate the dermis for possible invasion. • Treatment options include complete excision with clear margins, and electrodesiccation and curettage for smaller lesions. Any of these options is curative in the vast majority of cases.







