48. Kearns-Sayre Syndrome
Definition
Kearns-Sayre syndrome is a very rare mitochondrial DNA disorder in which there is marked heterogenicity along with various inheritance patterns. It is distinguished by three features: (1) onset before 20 years of age; (2) a chronic, progressive external ophthalmoplegia; and (3) pigmentary degeneration of the retina.
Incidence
As of 1992, a total of 226 cases of Kearns-Sayre syndrome have been documented in all of medical literature. There is no observed predilection with regard to race or gender.
Etiology
Kearns-Sayre syndrome occurs as the result of mitochondrial DNA (mtDNA) deletions that produce a particular, peculiar phenotype. Most of the mtDNA deletions in this disorder are sporadic but occur most commonly between positions 8469 and 13147.
Signs and Symptoms
• Ataxia
• Cardiac conduction defects
• Cardiomyopathy
• Diabetes mellitus
• Fanconi syndrome (see p. 132)
• Hypothyroidism
• Lactic acidosis
• Muscle weakness
• Ophthalmoplegia
• Peripheral neuropathy
• Pigmentary retinopathy
• Ptosis
• Ragged, red fibers on muscle biopsy
• Sensorineural hearing loss
• Short stature
• Sideroblastic anemia
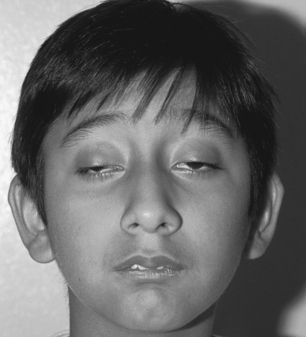 |
| Kearns-Sayre Syndrome. In this patient, note the arching of the brows in an effort to lift the eyelids to reduce the ptosis. |
Medical Management
Therapy to modify (cure) Kearns-Sayre syndrome does not currently exist. Ongoing research is directed at inhibiting replication of the mutant mtDNA or developing a way to encourage replication of wild-type mtDNA (nonmutated mtDNA).
True medical management consists of treatment of specific physiologic problems that may arise in association with the mtDNA mutation: insulin may be required to treat diabetes mellitus; a pacemaker may need to be inserted to treat the development of a harmful heart block; exercise routines may be established to manage myopathy(ies). Various vitamin supplements along with coenzyme Q 10 have demonstrated beneficial effects in individual situations. Death commonly occurs in the third or fourth decade of life.
Complications
• Deterioration of a wide range of observed signs and symptoms
• Heart block
Anesthesia Implications
The patient with an mtDNA disorder such as Kearns-Sayre syndrome is at greater risk for adverse events, including neurologic status deterioration, stroke, seizures, coma, respiratory failure, dysrhythmias, and death. Because of the increased risk for adverse anesthetic outcomes, no particular technique can be distinguished as the “best.”
The patient with an mtDNA disorder is potentially more susceptible to malignant hyperthermia (MH) and/ormyasthenia-like symptoms. In particular, the patient demonstrates greater sensitivity to nondepolarizing neuromuscular blocking agents. Because of the greater potential for MH, it is recommended that MH precautions be employed.
Succinylcholine should be avoided as well as other known MH triggers such as volatile inhalational agents. Total intravenous anesthesia may be a better choice for the patient with Kearns-Sayre syndrome.
Both the anesthetist and the patient should be prepared for the possibility that mechanical ventilatory support may need to be extended into the postoperative period because of residual muscle weakness. Admission to the intensive care unit should be arranged preoperatively so that close monitoring of the patient’s ventilatory status can continue without undue interruption.
Because of the patient’s propensity for lactic acidosis and because diabetes mellitus occurs frequently with this syndrome, the choice of intravenous fluid is important. To decrease the lactate load, lactated Ringer’s solution should not be used. The blood glucose level should be monitored frequently during surgery. Incorporation of glucose-containing solutions may be necessary. Insertion of an arterial pressure catheter may be prudent to facilitate the frequent blood sampling for glucose monitoring, serum lactate concentrations, and/or blood gas analysis.
A patient with an mtDNA disorder usually has poor tolerance for long periods of fasting. Typically the patient has become accustomed to eating frequent, small meals, and an accelerated intake schedule may be difficult to resolve. A possible scenario could be to allow intake of clear liquids containing some calories up to 2 hours preoperatively, with elimination of solid food occurring 8 hours before the surgery and anesthesia. Scheduling the patient’s surgery as the first case of the day will help facilitate patient compliance.







