14 Kawasaki Disease
Echocardiographic Assessment
Key Points
Background
Echocardiography (echo) is used to monitor for coronary artery involvement with examinations recommended at the time of diagnosis, 2 weeks from diagnosis, and 6 to 8 weeks after diagnosis, but may be done more frequently if a patient is at high risk for the development of aneurysms (Box 14-1). If the echocardiogram is normal at 6 to 8 weeks, then further follow-up by echo is considered optional. Patients with positive echocardiographic findings will require ongoing follow-up studies.
Overview of Echocardiographic Approach
Because Kawasaki disease can affect the coronary arterial system, echo provides an essential part of the evaluation of patients with Kawasaki disease. The initial echocardiogram should be a complete study to rule out any structural cardiac abnormalities, but also be focused to look at findings seen in Kawasaki disease. Careful examination of the coronary arteries is needed, and all major segments of the coronary arteries should be visualized, if possible. In addition, assessment of global ventricular function, presence of valvar regurgitation, and evaluation for pericardial effusion should be performed (Box 14-2).
Initial Echocardiographic Assessment in Kawasaki Disease
Anatomic Imaging
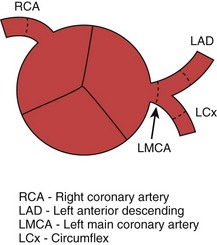
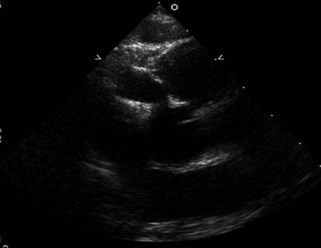
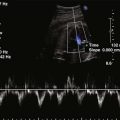
Anatomic imaging in patients with Kawasaki disease focuses on the coronary arteries (Fig. 14-1). However, a complete assessment of the patient needs to be done initially. A complete transthoracic echocardiogram with two-dimensional (2D), spectral, and color Doppler should be performed to assess for any structural cardiac disease. Areas of particular focus are global ventricular function and assessment for focal wall motion abnormalities, coronary artery abnormalities, valve regurgitation, and the presence of a pericardial effusion (Box 14-3).
Goals of Echocardiogram
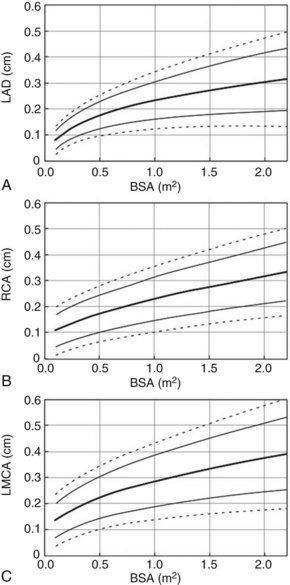
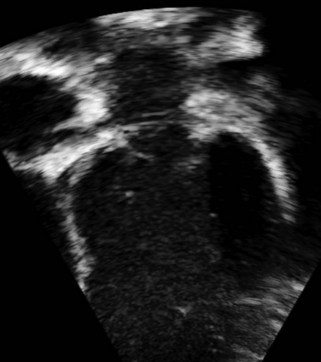
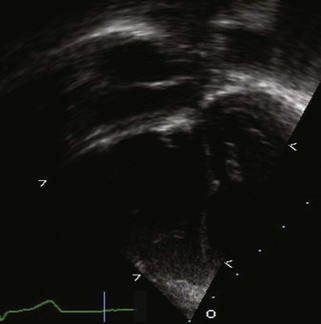
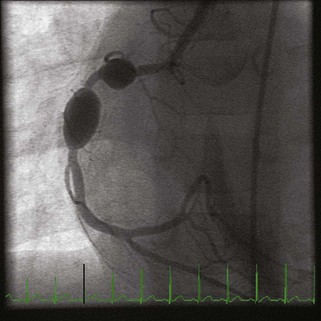
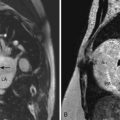
Coronary abnormalities seen in patients with Kawasaki disease include perivascular brightness, a lack of distal tapering of the coronaries, diffuse dilation (typically referred to as ectasia [Fig. 14-2]), and aneurysmal dilation (Figs. 14-3 and 14-4) of the coronary arteries. Aneurysms are rarely seen before 10 days into the illness. Coronary scarring, calcification, and stenosis are typically seen in later phases of the illness. Thrombosis of the coronary arteries can occur at any time during the illness. Aneurysms can be classified as saccular with equal lateral and axial dimensions giving the appearance of a round bead, fusiform with proximal and distal tapering of the aneurysm giving a more tubelike appearance, or giant where the aneurysm measures more than 8 mm in size (Box 14-4).
Acquisition
Initial echocardiogram is used as a baseline and should be a complete study.
Step 1: Complete Transthoracic Echocardiogram
Step 2: Assess Coronary Arteries
Echocardiographic Views for Coronary Arteries
Step 3: Assess Valve Function
Step 4: Assess Ventricular Function
Step 5: Assess Aortic Root
Analysis
Alternate Approaches
1 Baer AZ, Rubin LG, Shapiro CA, Sood SK, Rajan S, Shapir Y, et al. Prevalence of coronary artery lesions on the initial echocardiogram in Kawasaki syndrome. Arch Pediatr Adolesc Med. 2006;160:686-690.
2 Crystal MA, Syan SK, Yeung RS, Dipchand AI, McCrindle BW. Echocardiographic and electrocardiographic trends in children with acute Kawasaki disease. Can J Cardiol. 2008;24:776-780.
3 Fukazawa R, Ogawa S. Long-term prognosis of patients with Kawasaki disease: at risk for future atherosclerosis? J Nippon Med Sch. 2009;76:124-133.
4 Gordon JB, Kahn AM, Burns JC. When children with Kawasaki disease grow up: myocardial and vascular complications in adulthood. J Am Coll Cardiol. 2009;54:1911-1920.
5 Gupta-Malhotra M, Gruber D, Abraham SS, Roman MJ, Zabriskie JB, Hudgins LC, et al. Atherosclerosis in survivors of Kawasaki disease. J Pediatr. 2009;155:572-577.
6 Heuclin T, Dubos F, Hue V, Godart F, Francart C, Vincent P, et al. Increased detection rate of Kawasaki disease using new diagnostic algorithm, including early use of echocardiography. J Pediatr. 2009;155:695. 9.e1
7 JCS Joint Working Group. Guidelines for diagnosis and management of cardiovascular sequelae in Kawasaki disease (JCS 2008)–digest version. Circ J. 2010;74:1989-2020.
8 Mavrogeni S, Papadopoulos G, Karanasios E, Cokkinos DV. How to image Kawasaki disease: a validation of different imaging techniques. Int J Cardiol. 2008;124:27-31.
9 McCrindle BW, Li JS, Minich LL, Colan SD, Atz AM, Takahashi M, et al. Coronary artery involvement in children with Kawasaki disease: risk factors from analysis of serial normalized measurements. Circulation. 2007;116:174-179.
10 McMorrow Tuohy AM, Tani LY, Cetta F, Lewin MB, Eidem BW, Van Buren P, et al. How many echocardiograms are necessary for follow-up evaluation of patients with Kawasaki disease? Am J Cardiol. 2001;88:328-330.
11 Minich LL, Tani LY, Pagotto LT, Young PC, Etheridge SP, Shaddy RE. Usefulness of echocardiography for detection of coronary artery thrombi in patients with Kawasaki disease. Am J Cardiol. 1998;82:1143. 6, A10
12 Newburger JW, Takahashi M, Gerber MA, Gewitz MH, Tani LY, Burns JC, et al. Diagnosis, treatment, and long-term management of Kawasaki disease: a statement for health professionals from the Committee on Rheumatic Fever, Endocarditis, and Kawasaki Disease, Council on Cardiovascular Disease in the Young. American Heart Association. Pediatrics. 2004;114:1708-1733.
13 Ren X, Banker R. Cardiac manifestation of mucocutaneous lymph node syndrome (Kawasaki disease). J Am Coll Cardiol. 2009 Jun 30;54(1):89.
14 Seve P, Stankovic K, Smail A, Durand DV, Marchand G, Broussolle C. Adult Kawasaki disease: report of two cases and literature review. Semin Arthritis Rheum. 2005;34:785-792.