K
Kanizsa figure See figure, Kanizsa.
kataphoria 1. A tendency of the visual axes of both eyes to deviate below the horizontal plane, in the absence of a stimulus to fusion. 2. Synonym of alternating deorsumduction. Note: also spelt cataphoria.
See depression; hyperphoria.
Kayser–Fleischer ring See ring, Kayser–Fleischer.
Kearns–Sayre syndrome See ophthalmoplegia, chronic progressive external.
Keith–Wagener–Barker classification See retinopathy, hypertensive.
Kennedy syndrome See syndrome, Foster Kennedy.
Kepler telescope See telescope.
keratectasia See ectasia; staphyloma, anterior.
keratectomy, photorefractive A surgical procedure on the cornea aimed at correcting ametropia. The epithelium is completely removed over a central diameter of about 7 mm and excimer laser ablation is then carried out on the stroma. A bandage soft contact lens is usually worn afterwards for a few days while the epithelium regenerates. Complications are more common than with either LASEK or LASIK. Useful vision recovers more slowly and pain lasts longer than with the latter procedures. Syn. keratorefractive surgery; laser refractive keratoplasty (LRK); refractive keratoplasty.
See ectasia, corneal; keratotomy, radial.
keratic precipitates (KP) Cells (e.g. leukocytes) deposited on the endothelium of the cornea which occur as a result of inflammation of the iris or the ciliary body. They often collect in a triangular pattern with the base down (Arlt’s triangle) on the inferior portion of the endothelial surface. They may also be distributed diffusely over the endothelium, as in Fuchs’ heterochromic iridocyclitis or anterior uveitis, or concentrated in one area, as in disciform keratitis or herpes simplex keratitis. In granulomatous uveitis they are larger than in nongranulomatous uveitis, greasy in appearance (called ‘mutton fat’). Following treatment of the primary cause they usually disappear.
See cornea guttata.
keratitis Inflammation of the cornea. It can arise from various sources, the most common being: infection by bacteria, fungi or viruses, hypersensitivity to staphylococcal exotoxins, nutritional deficiencies, failure of the eyelids to cover the cornea, deficiencies in the precorneal tear film, contact lens wear (especially extended wear), mechanical, radiation or chemical trauma or interruption of the ophthalmic branch of the trigeminal nerve. It is usually characterized by a dullness and loss of transparency of the cornea due to infiltrates, neovascularization, oedema and is accompanied by ciliary injection. The discomfort varies from a foreign body sensation to severe pain, with lacrimation, photophobia, blepharospasm and an impairment of vision. If the condition is severe, ulcers and pus (hypopyon) will appear and the iris and ciliary body may become involved. It is important to identify the cause and the organism in order to treat the condition. Keratitis of bacterial origin is treated with antibiotic drugs. Keratitis of viral origin (e.g. herpes) is treated with antiviral agents and that of fungal origin with antifungal agents.
See corneal infiltrates; keratomalacia; keratomycosis; keratopathy.
acanthamoeba k. A rare type of keratitis caused by the microorganism acanthamoeba, which invades the cornea. The symptoms begin with a foreign body sensation, which turns into pain, photophobia, tearing, blepharospasm and blurred vision. The signs are infiltrates that develop into a ring, and the cornea may eventually become opaque. Diagnosis of the disease is made by laboratory analysis of a corneal scraping. Contact lens wear has been found to be associated with this disease in about threequarters of the cases, especially when the patient has used homemade or unpreserved saline. The other cases were due to contact with stagnant water or following an abraded cornea. The therapy is with repetitive doses of antiamoebic agents (e.g. biguanide) and an antibiotic (e.g. propamidine isethionate) or a combination of propamidine and neomycin. However, strict compliance with contact lens regimens and avoidance of exposure to dirty, stagnant water diminishes the risks of contracting the disease.
See corneal infiltrates; disinfection; propamidine isethionate.
actinic k. See keratoconjunctivitis, actinic.
acute epithelial k. See herpes zoster ophthalmicus.
acute stromal k. A complication of scleritis in which there are superficial and mid-stromal infiltrates in the limbal region. Lesions can also be noted in the central cornea and may develop vascularization and permanent opacification. In cases of scleritis that are limited (i.e. not diffuse), corneal changes are noted only in the bordering corneal region.
dendritic k. See keratitis, herpes simplex.
disciform k. A deep localized keratitis involving the stroma, usually characterized by a disc-shaped grey area (Wessley ring) that may spread to the whole thickness of the cornea. It is due to a viral infection (e.g. herpes simplex virus) or to an immune reaction, or it may also occur as a sequel to trauma. It may heal without residue or may cause scarring and vascularization of the cornea. Treatment is with steroid and antiviral agents.
See clouding, central corneal; keratic precipitates; ring, Wessley.
epithelial k. See keratitis, punctate epithelial.
exposure k. See keratopathy, exposure.
filamentary k. Keratitis characterized by the presence of fine epithelial filaments. It can occur as a result of herpes, thyroid dysfunction, corneal abrasions, keratoconjunctivitis sicca, etc.
fungal k. A keratitis caused by a fungus, such as Fusarium, Aspergillus, or Candida albicans. The condition may develop after eye injury (e.g. fingernail or contact lens scratch, tree branch), especially in agricultural areas. However, it has become more common since the use of corticosteroids. It may also occur in eyes suffering from corneal disease, after keratoplasty, diabetes or extended-wear contact lenses. It is characterized by greyish-white, rough ulcers with indistinct and feathery edges with filaments infiltrating into the stroma (filamentary keratitis). There is ciliary and conjunctival injection and it may be accompanied by ring abscesses and, in severe cases, hypopyon. The ulcers have oval or round outlines with a plaque-like surface and the cornea is fully oedematous. Differential diagnosis is facilitated by corneal scraping or biopsy of the ulcer. Management consists mainly of antifungal agents. Syn. mycotic keratitis.
See keratomycosis.
herpetic k. Keratitis caused by either herpes simplex or herpes zoster viruses.
See herpesvirus; keratitis, herpes simplex.
herpes simplex k. An inflammation of the cornea, which occurs occasionally as a result of a blepharoconjunctivitis caused by the herpes simplex virus (usually type 1). The disease begins with skin vesicles typically spread over the lids, conjunctiva and periorbital area. Symptoms include irritation, photophobia, tearing, reduced corneal sensation and blurred vision if the central cornea is involved. The characteristic sign is a dendritic ulcer, which enlarges progressively resulting in a configuration referred to as a geographical ulcer. Treatment is with an antiviral agent (e.g. aciclovir) or debridement of the epithelium if unresponsive to antiviral agents. Syn. dendritic ulcer.
See herpesvirus; keratitis, disciform; keratitis, interstitial; keratitis, punctate epithelial; keratitis, ulcerative.
hypopyon k. Purulent keratitis with ulcer resulting in the presence of pus in the anterior chamber, which gravitates to the bottom. The ulcer is a dirty grey colour and the conjunctiva is also inflamed. The usual cause of the infection is the pneumococcus which gives rise to a corneal ulcer (often called serpiginous ulcer because of its tendency to creep forward in the cornea).
See hypopyon; keratitis, ulcerative; ulcer, corneal.
interstitial k. Keratitis involving the stroma. It is characterized by deep vascularization of the cornea and is often associated with iridocyclitis. Formerly, the most common cause was congenital syphilis (syphilitic keratitis). However, nowadays it is usually the result of a herpes simplex infection, or it may be part of a syndrome (Cogan’s) or other systemic diseases (e.g. leprosy, tuberculosis). Management involves cycloplegics, topical antiviral agents and in severe cases corticosteroids. Syn. stromal interstitial keratitis.
See ring, Wessley; sign, Hutchinson’s.
lagophthalmic k. See keratopathy, exposure.
marginal k. A condition characterized by subepithelial peripheral corneal infiltrates which may spread circumferentially and are separated from the limbus by a clear zone, which may eventually become invaded by blood vessels. It is a hypersensitivity response to staphylococcal exotoxins. There is discomfort, pain, redness and photophobia. Treatment is with topical steroids.
microbial k., contact lens induced A keratitis caused by a microorganism such as a bacteria (e.g. Pseudomonas aeruginosa, Serratia marcescens), amoeba (e.g. Acanthamoeba), or less commonly a virus or fungus. The incidence of the condition is relatively low. It has been estimated to be 2 to 5 individuals with daily wear of soft lenses and 10 to 20 with extended wear of soft lenses per 10 000 per year. High oxygen permeability leads to less infection. Signs and symptoms include pain, infiltrates, redness, lacrimation, photophobia, corneal oedema, reduced vision, discharge, swollen lids and aqueous flare. The condition may have been precipitated by non-compliance, poor hygiene, dirty lens case, etc. Management includes cessation of lens wear and drug therapy.
mucous plaque k. See herpes zoster ophthalmicus.
mycotic k. See keratitis, fungal.
non-ulcerative k. See contact lens acute red eye.
neuroparalytic k. Keratitis caused by a failure of blinking or infrequent or incomplete blinking causing inadequate spread of tears.
See keratopathy, exposure.
neurotrophic k. See keratopathy, neurotrophic.
peripheral ulcerative k. A severe form of keratitis most often associated with a systemic disease, the most common being rheumatoid arthritis, Wegener’s granulomatosis, lupus erythematosus and polyarteritis nodosa. It is characterized by pain, usually redness and peripheral ulceration with corneal thinning. Treatment is urgent and directed towards the primary cause.
phlyctenular k. See keratoconjunctivitis, phlyctenular.
punctate epithelial k. (PEK) An inflammation of the cornea characterized by either multiple, small, superficial, punctuate lesions or minute, flat, epithelial dots resulting from bacterial infection (e.g. chlamydial, staphylococcal), vitamin B2 deficiency, virus infection (e.g. herpes) and also from exposure to ultraviolet light, injury to the eye with aerosol products or contact lens solutions. The condition is usually associated with conjunctivitis. Treatment depends on the causative agent (e.g. antiviral agents will be used to suppress symptoms in herpes simplex keratitis). Syn. superficial punctate keratitis (SPK), although this term is more often used to describe a PEK of viral origin.
See conjunctivitis, adult inclusion; keratitis, Thygeson’ superficial punctate.
rosacea k. Keratitis associated with acne rosacea of the face. It is characterized by marginal vascularization at the limbus. The vessels extend into the cornea surrounded by a zone of grey infiltration. The infiltrates and vascularization are in the cornea proper and not raised above the surface (unlike phlyctens). There is little tendency to ulcerate. It is usually associated with an inflammation of the conjunctiva (keratoconjunctivitis). Treatment involves topical steroid drops as well as systemic antibiotic therapy.
See acne rosacea; keratoconjunctivitis, phlyctenular.
k. sicca See keratoconjunctivitis sicca.
superficial punctate k. See keratitis, punctate epithelial.
stromal k.; syphilitic k. See keratitis, interstitial.
Thygeson’s superficial punctate k. A rare type of punctate epithelial keratitis. It is characterized by circular or oval, grayish-white epithelial lesions commonly located centrally and slightly elevated with a cluster of granular dots. The lesions show punctate staining with fluorescein. The cause is unknown, although a virus is suspected. It gives rise to mild irritation, photophobia and slight blurring of vision. Treatment includes artificial tears, corticosteroids (but this may induce recurrence) and therapeutic soft contact lenses. Untreated, it may subside within a few years.
ulcerative k. Any keratitis in which there is an ulcer of the cornea. The cause may be bacterial or viral infection, trauma or contact lens wear (particularly extended wear). The ulcer is a dirty grey coloured area on the cornea, the eye is red, the pain can be severe, there is photophobia, lacrimation, and vision may be affected. Immediate treatment is necessary: if due to contact lenses, cessation of wear and topical antibiotics will be used.
See keratitis, herpes simplex; ulcer, corneal.
ultraviolet k. See keratoconjunctivitis, actinic.
keratocele Hernia of Descemet’s membrane through a hole in the cornea caused by a perforating corneal ulcer or wound.
keratoconjunctivitis Inflammation of the conjunctiva and the cornea.
See keratitis, punctate epithelial; keratitis, rosacea.
actinic k. Inflammation of the cornea and conjunctiva caused by exposure to ultraviolet light as, for example, from sun lamps, welder’s arc or reflection from the snow. Both cornea and conjunctiva are usually involved although one tissue may be more affected than the other, hence the terms ‘actinic conjunctivitis’ or ‘actinic keratitis’. Some time after exposure (4–8 hours) to the ultraviolet radiations, the patient experiences a marked sandy feeling in the eye, lacrimation, photophobia, blepharospasm, with congestion of the conjunctiva and swelling of the eyelids. The condition is usually self-limited and heals within 48 hours. Symptoms are relieved with cold compresses, firm patching and an analgesic. A local anaesthetic may sometimes be used, but this delays the regeneration of the corneal epithelium and is not usually recommended. A topical antibiotic may also be used to prevent secondary infection. Sunglasses or suitable protection may prevent the condition. Syn. arc eye; flash blindness; photokeratitis; photokeratoconjunctivitis; photophthalmia; snow blindness (although this is not a strictly correct synonym it is often used as such); sun lamp conjunctivitis; ultraviolet keratitis.
See actinic.
atopic k. (AKC) A rare but serious inflammation of the conjunctiva and the cornea caused by a reaction of the tissues to an allergen (e.g. pollen, dust mite) in which there is an exaggerated immune response. This hypersensitivity is often associated with a family history of allergic diseases, such as asthma, atopic dermatitis or eczema. Patients are usually young adults. Common signs are redness, lid eczema, small papillae found on the lower and upper tarsal conjunctiva (unlike the large papillae of vernal conjunctivitis which occur only on the upper conjunctiva). Common symptoms are itching, photophobia, a burning sensation and blurred vision if there is keratitis. Treatment includes mast cell stabilizers and antihistamines, and in severe cases corticosteroids.
epidemic k. See conjunctivitis, contagious.
phlyctenular k. A condition characterized by the presence of phlyctenules (nodules) on the conjunctiva, limbus or even the cornea. It is a delayed hypersensitivity response to bacterial antigens (e.g. Staphylococcus, aureus, Candida albicans, Chlamydia trachomatis). Symptoms are soreness, lacrimation and if the cornea is involved photophobia. The nodules are pinkish-white on the conjunctiva surrounded by hyperaemia and greyish-white at the limbus and on the cornea. They leave a scar on the cornea (but not on the conjunctiva) when healed. The condition may resolve spontaneously but therapy is with topical corticosteroids. It is often associated with blepharitis or bacterial conjunctivitis. Syn. phlyctenulosis.
k. sicca (KCS) A condition affecting the cornea and conjunctiva due to, either a tear deficiency which is divided into two categories: Sjögren syndrome hyposecretive KCS and non-Sjögren syndrome hyposecretive KCS, or to an excessive evaporation of tears (evaporative KCS). KCS linked to Sjögren’s syndrome occurs in two forms: primary in which there is KCS with xerostomia (dry mouth) and secondary in which there is KCS with a systemic autoimmune connective tissue disease such as rheumatoid arthritis, systemic lupus erythematosus and systemic sclerosis. KCS without the association with Sjögren’s syndrome is most commonly age-related, but some cases may be due to injury to the lacrimal tissue by tumour, inflammation (e.g. trachoma), systemic disease (e.g. cicatricial pemphigoid, sarcoidosis,), systemic medications (e.g. antihistamines, antidepressants), xerophthalmia, photorefractive keratectomy, LASIK or congenital disease (e.g. congenital alacrima, Riley–Day syndrome). Evaporative KCS occurs due to an absence of the oily outer surface of the tear film, often as a result of meibomian gland dysfunction or blepharitis, or to abnormal lid-globe congruity, defective blinking, contact lens wear, airconditioning environment or wind.
Common diagnostic tests are tear film break-up time test, Schirmer’s test and rose bengal dye evaluation. Symptoms and signs of the various forms are similar, although they are more severe in patients who have Sjögren’s syndrome. Symptoms are burning, foreign body sensation, itching, photophobia and blurred vision (due to corneal involvement). Signs are mucus discharge (plaques and filaments), decreased tear meniscus and conjunctival injection. Management includes artificial tears, corticosteroids, punctal occlusion and in severe cases closure of the lacrimal puncta or tarsorrhaphy. Syn. dry eye; keratitis sicca.
See alacrima; cytology, impression; eye, dry; glands, meibomian; immunosuppressants; keratitis, filamentary; keratopathy, exposure; occlusion, punctual; test, non-invasive break-up time.
superior limbic k. (SLK) Chronic inflammation of the superior cornea and conjunctiva. It is characterized by hyperaemia, hazy epithelium and, often, corneal filaments near the upper limbus and the adjacent conjunctiva, and with the sensations of burning, itching, photophobia and hazy vision. The condition is bilateral in 50% of cases. Detection of the disease in its mild form is difficult, as it requires lifting the upper eyelid. The condition typically affects middle-aged women with thyroid dysfunction. It may be induced by soft contact lens wear. Smaller hard lenses, especially gas permeable, rarely cause this disease. Management involves several options: application of silver nitrate, topical medication (e.g. sodium cromoglicate), thermal cauterization of the superior bulbar conjunctiva, or occlusion of the lacrimal puncta/um to increase tear volume over the conjunctiva.
See ophthalmopathy, thyroid.
vernal k. See conjunctivitis, vernal.
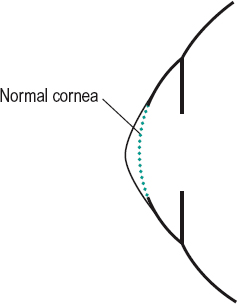
keratoconus (KC) A developmental anomaly in which the central portion of the cornea becomes thinner and bulges forward in a cone-shaped fashion. Two types of cones are commonly described: a round cone and an oval (or sagging) cone. It usually appears around puberty, is bilateral, although one eye may be involved long before the other. Other corneal signs may be Vogt’s striae, Fleischer’s ring, scarring and corneal hydrops, as well as myopia and irregular astigmatism. The condition may be associated with osteogenesis imperfecta, ectopia lentis, aniridia, retinitis pigmentosa, Down’s syndrome, Ehlers–Danlos syndrome, Marfan’s syndrome. The main symptom is a loss of visual acuity due to irregular astigmatism and myopia. Correction is usually best achieved with contact lenses, especially rigid gas permeable, but if these cannot be worn or the condition is very severe, a corneal transplant is carried out (Fig. K1). Syn. conical cornea.
See clouding, central corneal; degeneration, pellucid marginal; ectasia, corneal;hydrops, acute; keratoscope; lens, combination; lens, piggyback; lenticonus; sclera, blue; sign, Munson’s; sign, Rizzuti’s; stria; topography, corneal.
keratoconus fruste Term referring to subtle irregular astigmatism or moderate to high regular astigmatism usually measured by automated corneal topography and simulating keratoconus. However, the condition is usually stationary, corneal thickness is normal and there are none of the biomicroscopic signs of keratoconus (e.g. Vogt’s striae, Fleischer’s ring).
keratoconus, posterior A steep and irregular curvature of the posterior surface of the cornea, usually forming a depression in the central or paracentral area. The anterior surface is normal and vision is rarely affected. The condition is typically congenital, nonprogressive and unilateral, but some cases are associated with some ocular abnormalities, such as anterior polar cataract, lenticonus, ectopia lentis, iris atrophy, etc. As the cornea is much thinner it represents a contraindication to LASIK procedure. The majority of cases do not require treatment. See mesenchymal dysgenesis; videokeratoscope.
keratocyte See corneal corpuscle.
keratoglobus A rare, usually bilateral, protrusion of the cornea with general thinning, especially in the periphery. The condition is usually present at birth and generally does not progress. Some cases may be acquired perhaps as the end-stage of keratoconus. The diameter of the cornea is normal or slightly increased and the intraocular pressure is normal as the condition is not associated with congenital glaucoma. Complications include perforation after minor trauma and corneal hydrops. It is sometimes associated with Leber’s congenital amaurosis, Ehlers–Danlos syndrome and blue sclera. Syn. macrocornea.
See megalocornea.
keratolysis A severe corneal disorder in which the corneal stroma melts, which may result in descemetocele or even perforation. It is believed to be due to an altered epithelial barrier, which results in inflammatory mediators entering the stroma. The condition may occur as a complication of necrotizing scleritis or a severe inflammation of the peripheral cornea, especially in patients with a severe dry eye.
keratomalacia Vitamin A deficiency in which the cornea becomes desiccated at first and then softens, at which stage it is associated with infiltration, pannus, necrosis, opacification and the eye becomes blind. There is also a lack of reaction to inflammation leading to a destruction of the eye if infection occurs. It is part of a general systemic condition due to malnutrition. Associated with this condition are night blindness, faulty growth of bone, xerophthalmia, etc.
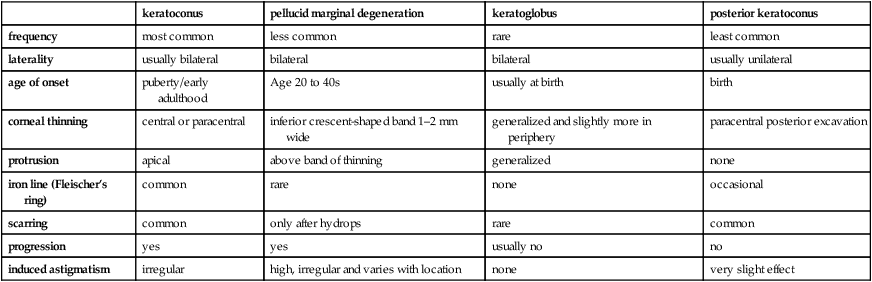
Table K1
Differential diagnosis between keratoconus and related thinning disorders. (Adapted from Krachmer JH, Feder RS, Belin MW. Surv Ophthalmol 1984; 28:293–322)
| keratoconus | pellucid marginal degeneration | keratoglobus | posterior keratoconus | |
| frequency | most common | less common | rare | least common |
| laterality | usually bilateral | bilateral | bilateral | usually unilateral |
| age of onset | puberty/early adulthood | Age 20 to 40s | usually at birth | birth |
| corneal thinning | central or paracentral | inferior crescent-shaped band 1–2 mm wide | generalized and slightly more in periphery | paracentral posterior excavation |
| protrusion | apical | above band of thinning | generalized | none |
| iron line (Fleischer’s ring) | common | rare | none | occasional |
| scarring | common | only after hydrops | rare | common |
| progression | yes | yes | usually no | no |
| induced astigmatism | irregular | high, irregular and varies with location | none | very slight effect |
See hemeralopia.
keratome A surgical instrument with a sharp edge for incising the cornea.
See keratomileusis; LASIK.
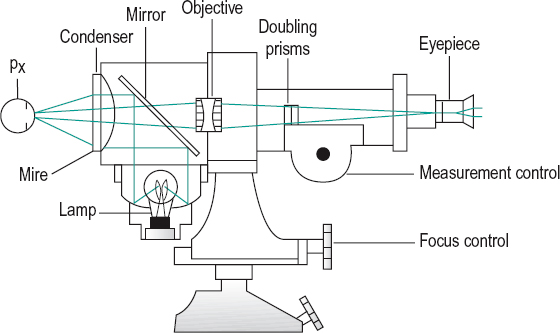
keratometer Optical instrument for measuring the radius of curvature of the cornea in any meridian. By measuring along the two principal meridians, corneal astigmatism can be deduced. The principle is based on the reflection by the anterior surface of a luminous pattern of mires in the centre of the cornea in an area of about 3.6 mm in diameter. Knowing the size of the pattern h and measuring that of the reflected image h’ and the distance d between the two, the radius of curvature r of the cornea can be determined using the approximate formula.
r = 2d (h’/h)
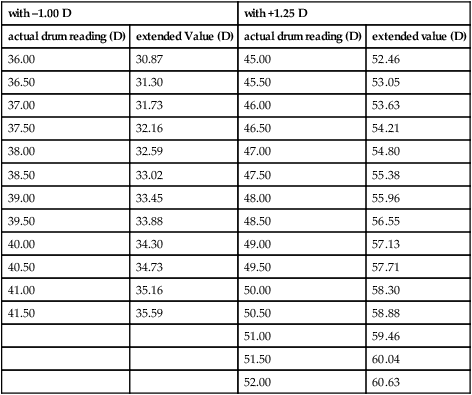
In addition, a doubling system (e.g. a bi-prism) is also integrated into the instrument in order to mitigate the effect of eye movements, as well as a microscope in order to magnify the small image reflected by the cornea. This instrument is used in the fitting of contact lenses and the monitoring of corneal changes occurring as a result of contact lens wear (Fig. K2). The range of the instrument can be extended approximately 9 D by placing a +1.25 D lens in front of the objective to measure steeper corneas. The range in the other direction can be extended by approximately 6 D using a –1.00 D lens to measure flatter corneas. Syn. ophthalmometer.
See fitted on K; keratoscope; lens, liquid; photokeratoscopy; prism, Wollaston; rule, Javal’s; Topogometer; videokeratoscope.
keratometer, auto A keratometer using a microprocessor computer to facilitate the rapid measurement of the corneal curvature. Such instruments usually provide measurements of the peripheral and central corneal curvatures at different points providing a contour of the cornea in several meridians, as well as of the corneal apex.
keratomileusis A surgical procedure on the cornea aimed at correcting ametropia. An anterior layer of the cornea is sliced off with a microkeratome, frozen, ground to a new curvature and sutured back in the same location. There are many complications and technical difficulties associated with this procedure. Syn. refractive keratoplasty and keratorefractive surgery (both terms also include epikeratoplasty, keratophakia and radial keratotomy).
See epikeratoplasty; Intacs; keratectomy, photorefractive; keratome; keratophakia; LASEK; LASIK.
keratomycosis A fungus infection of the cornea, which may result in keratitis and ulceration. It is usually introduced by injury and is characterized by an ulcer, which appears as a fluffy white elevated protuberance surrounded by a shallow crater on the edge of which is a sharply demarcated halo. There is ciliary and conjunctival injection. Diagnosis is best provided by laboratory analysis of a specimen of these fungal organisms, which are obtained by scraping the base of the ulcer.
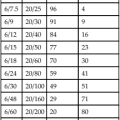
Table K2
Extended keratometer range
| with –1.00 D | with +1.25 D | ||
| actual drum reading (D) | extended Value (D) | actual drum reading (D) | extended value (D) |
| 36.00 | 30.87 | 45.00 | 52.46 |
| 36.50 | 31.30 | 45.50 | 53.05 |
| 37.00 | 31.73 | 46.00 | 53.63 |
| 37.50 | 32.16 | 46.50 | 54.21 |
| 38.00 | 32.59 | 47.00 | 54.80 |
| 38.50 | 33.02 | 47.50 | 55.38 |
| 39.00 | 33.45 | 48.00 | 55.96 |
| 39.50 | 33.88 | 48.50 | 56.55 |
| 40.00 | 34.30 | 49.00 | 57.13 |
| 40.50 | 34.73 | 49.50 | 57.71 |
| 41.00 | 35.16 | 50.00 | 58.30 |
| 41.50 | 35.59 | 50.50 | 58.88 |
| 51.00 | 59.46 | ||
| 51.50 | 60.04 | ||
| 52.00 | 60.63 | ||
See keratitis, fungal; ulcer, corneal.
keratopathy A non-inflammatory disease of the cornea.
actinic k. A form of corneal degeneration characterized by white or yellowish stromal deposits consisting of cholesterol, fats and phospholipids, and in some cases corneal vascularization. The condition may be caused by exposure to sunlight (especially ultraviolet radiations) or trauma. The deposits are usually present within the pupillary area, often as elevated nodules distributed in a band-shaped configuration, and can have a dramatic effect on visual function. The damage is similar to that found in pterygium and pinguecula. Treatment consists of resorbing the lipid infiltrates and, in severe cases, keratoplasty. Syn. Bietti’s band-shaped nodular dystrophy; climatic droplet keratopathy; Labrador keratopathy; lipid droplet degeneration.
band k. A disorder characterized by the deposition of calcium salts in the anterior layers of the cornea, such as the basement membrane, Bowman’s layer and the anterior stromal lamellae. They appear as opacities forming a more or less horizontal band with clear holes within the band giving it a Swiss cheese appearance. The causes may be systemic (e.g. hypercalcaemia, familial, old age, chronic renal failure) or ocular (e.g. chronic anterior uveitis, interstitial keratitis, silicone oil in the anterior chamber, phthisis bulbi). It is commonly associated with juvenile idiopathic arthritis and sarcoidosis. Symptoms include irritation and blurring of vision. Treatment may be necessary for cosmetic or visual reasons. It consists of removal of the calcium salts by scraping the corneal epithelium followed by irrigation with EDTA, or laser keratectomy. Syn. band-shaped corneal dystrophy.
See arthritis, juvenile idiopathic; ethylenediamine tetraacetic acid (EDTA).
bullous k. Degenerative condition of the cornea characterized by the formation of epithelial blebs or bullae, which burst after a few days. This condition may follow cataract surgery, corneal trauma, severe corneal oedema, glaucoma, iridocyclitis, etc. Soft contact lenses have often been found useful to relieve pain in this condition by protecting the denuded nerve endings.
See cornea guttata; dystrophy, Fuchs’ endothelial; lens, therapeutic soft contact.
climatic droplet k.; Labrador k. See keratopathy, actinic.
exposure k. A disorder caused by the failure of the eyelids to cover the globe, resulting in improper wetting of the ocular surface by the tears with consequent desiccation of the corneal epithelium. This condition may be caused by facial nerve disorders in which the orbicularis oculi muscle is paralysed, or sleep lagophthalmos, or as a result of hard contact lens wear. The cornea presents punctate epithelial erosions, which may develop, into ulcers. Treatment is with frequent lubrication and if severe, lid surgery may be required. Syn. lagophthalmic keratitis; neuroparalytic keratopathy.
See keratitis, neuroparalytic; staining, 3 and 9 o’clock.
neurotrophic k. Condition characterized by an anaesthesia of the cornea. It results in a breakdown of the corneal epithelial layer allowing trauma, desiccation and infection. It is believed to occur as a result of the loss of trophic influence of the nerve supply to the cornea and/or of reduced blinking and the loss of lacrimation. Causes include herpes simplex virus, herpes zoster, lattice dystrophy, fifth nerve lesion and diabetes mellitus. Treatment mainly consists of tear substitute and intermittent or constant lid taping, but anti-infective regimen, punctal occlusion, tarsorrhaphy or neurosurgical intervention may be necessary. Syn. neurotrophic keratitis.
keratophakia A surgical procedure on the cornea aimed at correcting ametropia. A donor corneal disc (or lenticule) that was previously frozen and reshaped is inserted into the host cornea to modify the anterior corneal curvature. There are many complications and technical difficulties associated with this procedure. Syn. refractive keratoplasty and keratorefractive surgery (both terms also include epikeratoplasty, keratomileusis and radial keratotomy).
See epikeratoplasty; Intacs; keratomileusis; keratectomy, photorefractive; LASIK; LASEK; lenticule.
keratoplasty Excision of corneal tissue and its replacement by a cornea from a human donor. This can be done either over the entire cornea (total keratoplasty) or over a portion of it (partial keratoplasty). Two main techniques are used: (1) the penetrating keratoplasty in which the entire thickness of the cornea is removed and replaced by transparent corneal tissue; (2) the lamellar keratoplasty in which a superficial layer is removed and replaced by healthy tissue. Common indications to perform keratoplasty are therapeutic (e.g. keratoconus, corneal ulcer) or cosmetic (e.g. removing an unsightly opacity). Syn. corneal transplant.
See ciclosporin; dystrophy, granular; eye bank; graft, corneal; immunosuppressants.
keratoplasty, laser refractive; refractive
See keratectomy, photorefractive.
Keratoprosthesis A corneal implant.
keratoreformation The process of improving vision following photorefractive keratectomy by correcting a residual ametropia and an irregular corneal topography. This is usually accomplished by contact lenses.
keratorefractive surgery See epikeratoplasty; Intacs; keratomileusis; keratophakia; keratectomy, photorefractive; LASEK; LASIK.
keratoscleritis Inflammation of both the cornea and the sclera.
keratoscope Instrument for examining the front surface of the cornea. It consists of a pattern of alternately black and white concentric rings reflected by the cornea and seen through a convex lens mounted in an aperture at the centre of the pattern. Such an instrument gives a qualitative evaluation of large corneal astigmatism, and is useful in cases of irregular astigmatism as in keratoconus, for example (Fig. K3). Syn. Placido disc.
See corneal topography; photokeratoscopy; videokeratoscope.
keratosis nigricans See acanthosis nigricans.
keratosis, seborrhoeic Lesion of the skin appearing as brown or yellowish thickening of the skin of the face, eyelids and/or conjunctiva. It is common in the elderly and may be a precursor to squamous cell carcinoma. Management includes cryotherapy, local surgical excision or radiotherapy.
keratotomy, radial (RK) A surgical procedure on the cornea aimed at correcting ametropia. It consists of making incisions in the anterior part of the cornea in order to flatten it and thereby produce a reduction of its power. The incisions are usually radial, extending from the limbus to about halfway towards the centre like the spokes of a wheel, but other patterns of incision are also used. In some cases, the procedure does not produce a perfect correction and vision is poor, especially in the dark. The use of the excimer laser provides greater accuracy and success. The technique is then called laser refractive keratoplasty (LRK) or photorefractive keratectomy (PRK). Syn. refractive keratoplasty and keratorefractive surgery (both terms also include epikeratoplasty, keratomileusis and keratophakia).
See cornea; epikeratoplasty; keratectomy, photorefractive; keratomileusis; keratophakia; keratoreformation; LASEK; LASIK.
Kestenbaum’s rule See rule, Kestenbaum’s.
ketoconazole See antifungal agent.
ketotifen See antihistamine.
ketorolac See antiinflammatory drug.
keyhole bridge; pupil; visual field See under the nouns.
kinescope 1. An instrument for determining the refraction of the eye by having the subject observe the apparent ‘with’ or ‘against’ movement of a test object through a stenopaeic slit moved across the front of the eye. 2. An instrument for recording television programmes.
See disc, stenopaeic.
kinetic depth effect See effect, kinetic depth.
kinetic perimetry See perimetry, kinetic.
Kirschmann’s law See law, Kirschmann’s.
Knapp procedure See transposition.
Koeppe lens; nodules See under the nouns.
Kollner’s rule See rule, Kollner’s.
König bars Target used to measure visual acuity consisting of two bars on a white background. The length of each bar is usually three times its width but the space between the bars is always equal to the width of one bar. The smallest pair of bars that can be perceived as separate gives a measure of the acuity.
Krause’s end bulbs Nerve endings enclosed by a capsule from 0.02 mm to 0.1 mm in length. They probably act as cold receptors. Their regular presence in the corneal limbus has been questioned.
Krause, glands of See glands of Krause.
Krimsky’s method See method, Krimsky’s.
Krukenberg’s spindle A more or less vertical spindle-shaped deposition of brownish pigment on the corneal endothelium. It is often accompanied by pigment deposits on the lens, zonule, anterior surface of the iris and trabecular meshwork and may form part of the pigment dispersion syndrome. The pigment comes from the iris pigment epithelium, but the cause of its shedding is not established and may be strenuous exercise, mechanical rubbing by the zonules due to posterior bowing of part of the iris or degenerated pigment. It occurs in young to middle-aged myopic individuals and sometimes following uveitis.
krypton laser See laser, krypton.
Kuhnt, central meniscus of See membrane, Elschnig’s inner limiting.