Jaundice
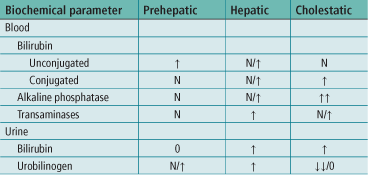
Jaundice is yellow discoloration of the tissues, noticed especially in the skin and sclera (Figs 28, 37), due to accumulation of bilirubin. For jaundice to be clinically apparent, the circulating bilirubin levels should be in excess of 35 μmol/L. Jaundice may be prehepatic (due to haemolysis), hepatic (due to intrinsic liver disease) or cholestatic (due to either intrahepatic cholestasis or post-hepatic biliary tract obstruction).

Figure 37 Jaundiced sclera in a patient with hepatitis.
Mild jaundice is evident in the sclera. There is no obvious jaundice in the skin. Jaundice in the sclera is usually clinically apparent when the circulating bilirubin levels are in excess of 35 μmol/L.
History
General
Fever, malaise, weight loss, dark urine, pale stools, itching.
Newborn
Biliary atresia presents as deepening jaundice within 2–3 days of birth. Liver failure develops over 3–6 months. Physiological jaundice is common and is due to immaturity of liver function. It usually settles within the first week of life.
Prehepatic
Ask about family history, racial origin, drugs, haematuria, history of anaemia. Gilbert’s disease is inherited as an autosomal dominant. There is a failure of uptake of unconjugated bilirubin by the hepatocyte. Crigler–Najjar syndrome is a failure of conjugation within the hepatocyte.
Hepatocellular
Occupation. Contact with jaundice. Travel. Alcohol. Sexual activity. Drugs (tablets, injections, anaesthetic agents, drug abuse). Exposure to industrial solvents. Previous episodes of jaundice. Infection. Influenza-like symptoms. Rashes. Joint pains. Blood transfusions.
Examination
Prehepatic (haemolytic)
Often the jaundice is not intense, with only a mild lemon tinge. Anaemia. Splenomegaly.
Hepatic
Tender liver in hepatitis. Signs of liver failure: spider naevi, palmar erythema, leuconychia, clubbing, gynaecomastia, testicular atrophy, ascites, peripheral oedema, bruising, Dupuytren’s contracture, caput medusae, liver flap. Haematemesis may have occurred from bleeding oesophageal varices.
Cholestatic
Hepatomegaly – usually smooth liver with ‘sharp’ edge. Palpable gall bladder (Courvoisier’s law – in the presence of obstructive jaundice if the gall bladder is palpable, the cause is unlikely to be due to gallstones). Epigastric mass, e.g. carcinoma of the pancreas. Other abdominal masses, e.g. carcinoma of the stomach and carcinoma of the colon with secondary deposits in the porta hepatis. Recent surgical scars. Scratch marks on abdomen from itching.
General Investigations
■ FBC, ESR, blood film
Hb ↓ malignancy, haemolysis. WCC ↑ infection, e.g. hepatitis, cholangitis. ESR ↑ infection, malignancy. Blood film – spherocytosis.
■ Reticulocyte count
Haemolysis.
■ U&Es
Deranged renal function with hepatorenal syndrome.
■ Viral antibodies
Hepatitis A, hepatitis B, hepatitis C, CMV, EBV.
■ US
Gallstones. Dilated biliary tree. Level of obstruction (may not show cause of obstruction). Hepatic secondaries. Cirrhosis.
■ ERCP
Periampullary carcinoma. Stones in common bile duct. Tumour of common bile duct. Stricture of common bile duct. Biopsy. Brush cytology. Stenting.
■ PTC
Undertaken if ERCP fails.
■ MRCP
Bile duct anomalies. Stones.
■ CT
Carcinoma of the head of the pancreas – assess spread and local resectability. Liver secondaries.
Specific Investigations
■ Serum copper
Reduced in Wilson’s disease.
■ Serum ceruloplasmin
Reduced in Wilson’s disease.
■ Serum α1-antitrypsin
α1-Antitrypsin deficiency. Serum iron and TIBC.
Iron raised in haemochromatosis. TIBC saturation>70%.
■ Leptospirosis complement fixation test
Leptospirosis.