J
J receptors, see Juxtapulmonary capillary receptors
J wave, see Hypothermia
Jackson, Charles T (1805–1880). US chemist, present at Wells’ unsuccessful demonstration of N2O in 1846; suggested diethyl ether to Morton for dental topical anaesthesia instead. Applied for the patent rights to ether jointly with Morton, the latter subsequently taking over 90% of Jackson’s share. Jackson later claimed sole credit for the discovery of anaesthesia.
Jackson, Chevalier (1865–1958). Renowned US laryngologist. Perfected a direct-vision laryngoscope in the early 1900s, and wrote extensively on laryngoscopy and tracheal insufflation.
• Normal formation and metabolism of bilirubin:
 haemoglobin is broken down to amino acids and haem in the reticuloendothelial system. Haem is further metabolised to lipid-soluble unconjugated bilirubin that is transported (bound to albumin) to the liver.
haemoglobin is broken down to amino acids and haem in the reticuloendothelial system. Haem is further metabolised to lipid-soluble unconjugated bilirubin that is transported (bound to albumin) to the liver.
 in the liver, unconjugated bilirubin is conjugated with glucuronic acid, rendering it water-soluble.
in the liver, unconjugated bilirubin is conjugated with glucuronic acid, rendering it water-soluble.
 increased bilirubin production, e.g. haemolysis. Usually mild. Unconjugated and conjugated bilirubin levels are raised, with increased urinary urobilinogen.
increased bilirubin production, e.g. haemolysis. Usually mild. Unconjugated and conjugated bilirubin levels are raised, with increased urinary urobilinogen.
 impaired conjugation of bilirubin, e.g. hepatitis, cirrhosis, drug-induced (e.g. α-methyldopa, paracetamol), hepatic failure. Unconjugated bilirubin is raised; urinary urobilinogen may be raised because the liver is unable to re-excrete it.
impaired conjugation of bilirubin, e.g. hepatitis, cirrhosis, drug-induced (e.g. α-methyldopa, paracetamol), hepatic failure. Unconjugated bilirubin is raised; urinary urobilinogen may be raised because the liver is unable to re-excrete it.
 congenital abnormalities of bilirubin transport are rare, except for Gilbert’s syndrome (hepatic glucuronyltransferase deficiency causing mild unconjugated bilirubinaemia with otherwise normal liver function tests and no urinary bilirubin).
congenital abnormalities of bilirubin transport are rare, except for Gilbert’s syndrome (hepatic glucuronyltransferase deficiency causing mild unconjugated bilirubinaemia with otherwise normal liver function tests and no urinary bilirubin).
 obstruction of bile drainage, e.g. gallstones, pancreatic carcinoma, cholangitis, cholecystitis (extrahepatic), primary biliary cirrhosis, drug-induced, e.g. contraceptives. Conjugated bilirubin is raised, often markedly, and is excreted in the urine, which is dark (but with reduced urobilinogen). Faeces are pale and fatty. Itching is common.
obstruction of bile drainage, e.g. gallstones, pancreatic carcinoma, cholangitis, cholecystitis (extrahepatic), primary biliary cirrhosis, drug-induced, e.g. contraceptives. Conjugated bilirubin is raised, often markedly, and is excreted in the urine, which is dark (but with reduced urobilinogen). Faeces are pale and fatty. Itching is common.
The latter two types are frequently mixed and difficult to distinguish.
Jaundice in ICU patients is often part of the presenting problem (e.g. in hepatic failure, biliary obstruction, sepsis) or may result from drug therapy, the development of acalculous cholecystitis, haemolysis of intra-abdominal haematoma, ischaemic hepatitis (in shocked patients) or the administration of TPN. It may also be part of multiple organ dysfunction syndrome.
 support of other organs, e.g. circulation, respiration.
support of other organs, e.g. circulation, respiration.
 treatment of associated clotting abnormalities, e.g. with clotting factors, vitamin K.
treatment of associated clotting abnormalities, e.g. with clotting factors, vitamin K.
 preoperative assessment as above, and for hepatic failure, depending on severity and cause.
preoperative assessment as above, and for hepatic failure, depending on severity and cause.
 risk of perioperative acute kidney injury due to acute tubular necrosis or hepatorenal syndrome:
risk of perioperative acute kidney injury due to acute tubular necrosis or hepatorenal syndrome:
– especially common with obstructive jaundice, since bilirubin levels are often highest.
– more likely if dehydration or biliary sepsis is present.
– plasma urea/creatinine is monitored preoperatively.
– preoperative iv hydration is instituted to maintain urine flow above 1 ml/kg/h.
– mannitol may be given if bilirubin is very high or urine output inadequate despite hydration. Furosemide has also been used.
 anaesthetic drugs and techniques as for hepatic failure.
anaesthetic drugs and techniques as for hepatic failure.
• Postoperative jaundice may be due to:
 underlying medical/surgical conditions.
underlying medical/surgical conditions.
 haemolysis, e.g. due to blood transfusion reaction, or following extensive bruising and haematoma.
haemolysis, e.g. due to blood transfusion reaction, or following extensive bruising and haematoma.
Jaundice is particularly hazardous in neonates; the immature blood–brain barrier allows penetration of bilirubin into the basal ganglia of the brain, causing kernicterus (convulsions may occur, leading to brain damage).
Jaw, fractured, see Facial trauma
Jaw, nerve blocks, see Gasserian ganglion block; Mandibular nerve blocks; Maxillary nerve blocks
Jehovah’s Witnesses. Religious group founded in the USA in the 1870s. Believe that they alone will survive the imminent destruction of the world, with a small proportion passing into Heaven to rule over the remainder of worthy individuals who will reside in an earthly paradise. Since 1945, also believe that to receive blood products is against God’s will, thus causing potential difficulties perioperatively. Special consent forms are usually employed. For paediatric surgery, a court order is required in order to overrule parents’ wishes. Although blood, plasma and autologous predonation are unacceptable, cell salvage, cardiopulmonary bypass and recombinant erythropoietin and factor VIIa are usually permitted. Autologous blood transfusion is usually permitted only if contact of blood with the body is not broken. Other factors such as platelets, clotting factors, albumin and intravenous immunoglobulin are ‘matters of conscience’ for individual Witnesses. Special measures to reduce blood loss may be required, e.g. hypotensive anaesthesia, recombinant factor VIIa.
[Jehovah (Old Testament); divine being]
Jet mixing. Effect of a jet of gas (e.g. O2) delivered from a nozzle into ambient gas, e.g. air. Energy is transferred from O2 molecules to adjacent air molecules; the latter are entrained into the jet due to viscous shearing between the gas layers. Employed in injector techniques for IPPV, and in fixed performance O2 masks. In the latter, air is entrained to a fixed degree depending on O2 flow rate and the size of side ports in the entrainment device.
Jet ventilators, see High-frequency ventilation; Injector techniques; Ventilators
JG cells, see Juxtaglomerular cells
Jorgensen technique. Outmoded form of sedation for dental surgery, described in 1953, using pentobarbital, pethidine and hyoscine iv.
[Niels B Jorgensen (1894–1974), Danish-born Californian dentist]
Joule. SI unit of energy. 1 joule = work done when the point of application of a force of 1 newton moves 1 metre in the direction of the force (1 J = 1 N × 1 m).
Joule–Thomson effect (Joule–Kelvin effect). Lowering of temperature when a gas expands, e.g. passing from a cylinder under pressure to a large space. The principle is employed in the cryoprobe. Conversely, temperature rises if gas within a small space is compressed.
Jugular bulb catheterisation. Performed to allow access to the blood draining the brain, and used to estimate the balance between cerebral oxygen delivery and utilisation. The jugular bulb is a dilatation of the internal jugular vein just below the base of the skull and may be catheterised using a Seldinger technique with the needle inserted lateral to the carotid pulsation at the level of the thyroid cartilage and directed cranially towards the external auditory meatus.
Cerebral oxygenation can only be accurately monitored if the dominant jugular bulb is used. The right side is often chosen as it is usually dominant; more accurate identification of dominance can be made by ultrasound examination of the internal jugular veins or by identifying the larger increase in intracranial pressure that occurs during manual compression of each internal jugular vein.
Blood may be sampled for PO2 and O2 saturation (SjO2), giving an indication of cerebral blood flow (lower values reflecting greater uptake by the brain and therefore less blood flow, assuming O2 consumption remains constant), and concentrations of lactate and other substances. Indwelling fibreoptic sensors may also be placed to give a continuous reading of global cerebral O2 saturation; this has been used particularly during cardiopulmonary bypass, in neurosurgery and after head injury. Desaturation (SjO2 < 55%) indicates impending cerebral ischaemia, e.g. caused by hypotension, hypocapnia, increasing cerebral oedema.
Jugular veins. Include the internal, external and anterior jugular veins (Fig. 93; see also Fig. 113; Neck, cross-sectional anatomy).
 passes through the jugular foramen at the base of the skull, draining the intracranial structures via the sigmoid sinus.
passes through the jugular foramen at the base of the skull, draining the intracranial structures via the sigmoid sinus.
 lies at first posterior, then lateral, to the internal carotid artery. Contained within the carotid sheath with the carotid artery and vagus nerve; the cervical sympathetic chain lies behind the sheath.
lies at first posterior, then lateral, to the internal carotid artery. Contained within the carotid sheath with the carotid artery and vagus nerve; the cervical sympathetic chain lies behind the sheath.
 has a dilatation at each end (jugular bulb), with valves above the lower bulb.
has a dilatation at each end (jugular bulb), with valves above the lower bulb.
See also, Cerebral circulation; External jugular venous cannulation; Internal jugular venous cannulation; Jugular bulb catheterisation
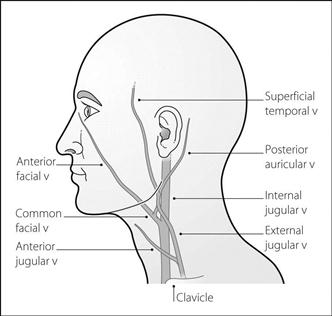
Fig. 93 Venous drainage of head and neck
Jugular venous pressure (JVP). Assessed by observing the height (in cm) of visible pulsation in the jugular veins above the sternal angle, with the patient reclining at 45°. The normal value is zero; i.e. the venous pulsations are not normally visible. The JVP falls during inspiration, and rises during expiration and when pressure is applied to the abdomen (Q sign). Pulsations are usually non-palpable. The venous waveform may be apparent. JVP may be difficult to identify in obese patients.
Useful as a clinical guide to right atrial pressure; raised in right-sided cardiac failure, hypervolaemia and mechanical obstruction, e.g. tricuspid stenosis or superior vena caval obstruction.
Junctional arrhythmias (Nodal arrhythmias). Arrhythmias arising from the atrioventricular node. Common during anaesthesia, especially deep inhalational anaesthesia.
On the ECG, inverted P waves may precede, follow or be hidden by the (normal) QRS complexes. Usually of little clinical significance, although cardiac output may be reduced. Cannon waves may be visible in the jugular venous waveform.
Atropine and ephedrine have been used to restore sinus rhythm in bradycardia; junctional tachycardias may respond to lidocaine and similar drugs.
Juxtaglomerular apparatus. System adjacent to renal glomeruli, composed of:
Responds to reductions in renal perfusion pressure by secreting renin, although the exact mechanism is unclear. Possibly renal vasodilatation is involved, since β-adrenergic receptor agonists, prostacyclin, bradykinin, dopamine, furosemide and vasodilator drugs all increase renin secretion. Conversely, α-adrenergic receptor agonists, vasopressin, and angiotensin reduce renin secretion.
Juxtapulmonary capillary receptors (J receptors). Receptors present in alveolar walls near the pulmonary capillaries. Thought to be responsible for the tachypnoea seen in pulmonary oedema and interstitial lung disease, via vagal afferent fibres. Their role in normal lungs is unknown.