12 ITU
Shock
Case history (1)
On examination he is pale and clammy. His pulse is 100/min, poor volume and BP 90/60.
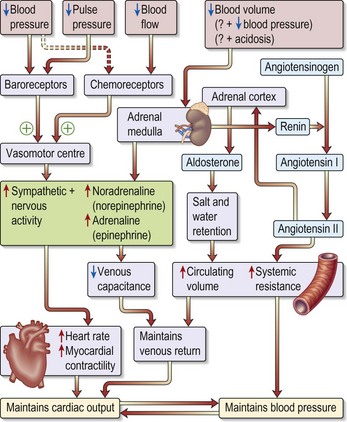
Physiology (Fig. 12.1)
Shock is ‘inadequate tissue oxygenation’ where there is failure of the circulatory system due to:
Causes of shock
Is the shock state in Case 1 due to myocardial infarction, an obstructed circulation or other shock-inducing factors?
Clinical examination
In assessing the shocked patient the following indices should be monitored:
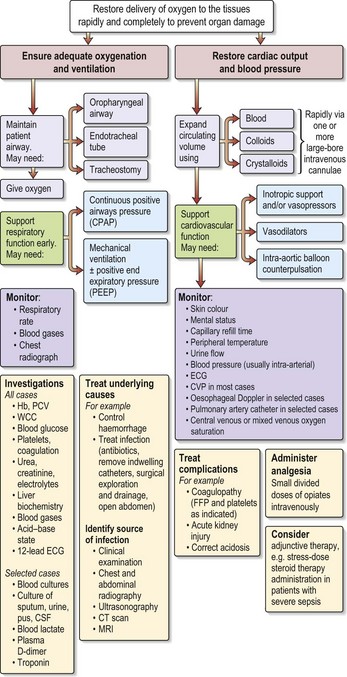
Other investigations (see Fig 12.2)
• Arterial blood gas analysis: in hypovolaemic shock (as in all shock states) there is a metabolic acidosis with a high hydrogen ion concentration and low bicarbonate concentration. In cases with respiratory complications the pO2 and pCO2 values will help indicate the need for ventilatory support.
• Lactate levels: blood lactate levels rise approximately in proportion to the severity of the shock.
• X-rays: these are usually of little value in the acute stages of shock management. A CXR will exclude any treatable pathology, such as a pneumothorax or haemothorax often complicating insertion of monitoring lines. A CT scan may be helpful in, for example, a case of trauma.
How would you treat?
Case 1
Case 2
In hypovolaemic hypotension the principal issues are the reduction in further fluid loss and simultaneously restoring fluid volumes via wide-bore intravenous cannulae. Infusion of red cells provides sufficient oxygen transport capacity (a target of 7–9 g/dL is broadly accepted). Fresh frozen plasma (e.g. to obtain a target INR of < 1.5) might be necessary. At the earliest opportunity the patient with haematemesis will require endoscopy to find the bleeding lesion and treat (see p. 67).
How would you manage this case? (see Fig. 12.2)
Immediate action
• Correct hypoxaemia: high-flow O2 via a face mask.
• Determine cause: examination, chest and abdominal X-ray, ECG, ABGs, FBC, U&Es, amylase, blood cultures.
• Initiate treatment: IV fluid resuscitation with 0.9% saline, inotropes if no response to fluid resuscitation.
Shock is a medical emergency. The longer it persists, the lower the chance of recovery because secondary injury, from coexistent hypoxaemia and delayed reperfusion, is now recognised to cause further cytokine activation and the development of multiple organ failure (MOF).
Further management
• Early antibiotic therapy, e.g. Piperacillin with Tazobactam, as it was felt to be an upper GI perforation.
• Attempted early control of the source of infection: seek surgical opinion for treatment of abdominal condition.
• Central line for CVP measurement.
• Titrate fluid resuscitation to provide adequate cardiac output with good urine output.
• Inotropic support: give dopexamine, a dopamine analogue which is useful in patients with septic shock, as in this man with a low cardiac output and peripheral vasoconstriction.
• CPAP or intubation and IPPV.
• Early recourse to stress-dose steroid therapy if requiring vasoconstrictor therapy.
Acute lung injury/Acute Respiratory Distress Syndrome (ARDS)
What are the possible causes of depressed consciousness and what are your immediate actions?
• You need to consider intoxication, hypoglycaemia, respiratory failure, head injury or a post-ictal state.
On examination, look for evidence of focal neurological signs, pinpoint pupils, trauma to the head or evidence of seizures such as tongue laceration, incontinence.
What do these results indicate?
• Acute type 1 respiratory failure with a metabolic (lactic) acidosis.
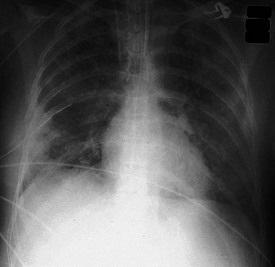
• There is vomitus around the mouth and on his clothing. The chest X-ray shows patchy shadowing at the right base.
• Following naloxone administration he becomes agitated, moving all limbs, but does not respond purposely to command.
Key features of acute lung injury/ARDS
• Pulmonary infiltrates: due to an increase in lung interstitial fluid not related to heart failure; by definition pulmonary artery occlusion pressure < 18 mmHg.
• A reduction in pulmonary compliance: i.e. stiff lungs, resulting in high inflation pressures.
• Profound gas exchange abnormalities defined as PaO2 : FiO2 ratio < 300 mmHg for acute lung injury (ALI) or < 200 mmHg for ARDS.
Pathophysiology
• Endothelial dysfunction leads to widespread interstitial oedema and impaired alveolar capillary perfusion.
• The stiff (low-compliance) lungs result in reduced tidal volume and reduced end expiratory lung volume – this then causes small airway collapse. Once collapsed, Laplace’s law explains why it is difficult to re-expand the airway (consider the difficulty in initially blowing up a balloon).
• Additional small airway pathology, particularly with direct lung injury, e.g. smoke inhalation.
• The lung can be likened to a wet sponge – the dependent sponge is waterlogged and the air spaces collapsed. Only the non-dependent areas of the lung might be contributing to gas exchange. The additional component of airway inflammation in some causes of ARDS explains the high mortality associated with direct lung injury (> 60%).
Management
• Deep sedation and neuromuscular paralysis to increase chest wall compliance. A semi-recumbent bed position unless contraindicated.
• Small tidal volumes (6 mL/kg of predicted body weight) and prolonged inspiratory time to limit airway pressure.
• Use of a minimum amount of PEEP (positive end-expiratory pressure) to recruit lung units.
• Prone positioning to improve {Vdot}/{Qdot} matching and clearance of lung secretions.
Experimental methods include:
Herridge MS, Tansey CM, Matte A, et al. Functional disability 5 years after acute respiratory distress syndrome. N Engl J Med. 2011;364:1293–1304.
Patekh D, Dancer RC, Thickett DR. Acute lung injury. Clin Med. 2011;11:615–618.
Wheeler AP, Bernard GR. Acute lung injury and the acute respiratory distress syndrome. Lancet. 2007;369:1556–1565.