Chapter 94 Is There a Role for Arthroscopy in the Treatment of Knee Osteoarthritis?
Arthroscopy was first described to treat osteoarthritis (OA) of the knee by Burman and coauthors1 in 1934. Over the past several decades, arthroscopic debridement of the degenerative knee has become a commonly performed orthopedic procedure. Despite its popularity, the exact role of arthroscopy in treating OA is controversial. Older, primarily uncontrolled cohort studies have suggested that arthroscopy has a variety of benefits in patients with early OA.2–6 However, a more recent study has suggested that the placebo effect may be responsible for the benefit related to arthroscopic treatment.7 The variety of arthroscopic procedures, the retrospective nature of the majority of published studies, and the lack of control subjects probably adds even more confusion as to which patients will benefit from arthroscopy.8
OPTIONS
Nonoperative management begins with activity modification, physical therapy, and a trial of anti-inflammatory medications. Many patients will often experience significant relief after intra-articular corticosteroid injections and hyaluronate injections. It is important to note that the degree of pain relief, as well as how long it lasts, can be varied.9
EVIDENCE
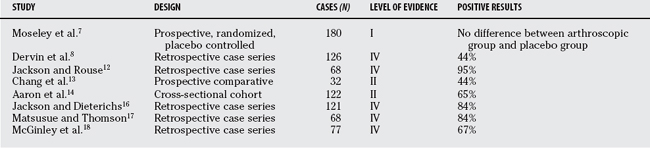
Several studies have been conducted in an effort to examine the effectiveness of arthroscopy in treating OA of the knee (Table 94-1). However, after conducting an evidence-based review of the current literature, we found only 1 study that contained Level I evidence. This study, by Moseley and colleagues,7 was a prospective, randomized, placebo-controlled trial of 180 patients with OA who were assigned to receive arthroscopic debridement, arthroscopic lavage, or placebo surgery. Their inclusion criteria included: (1) age < 75 years, (2) OA as defined by the American College of Rheumatology, (3) knee pain despite at least 6 months of conservative management, and (4) no arthroscopy performed on the knee in the previous 2 years. The severity of OA was assessed radiographically and graded from 1 to 4. The scores from all 3 compartments were added for a total of 0 to 12. Of note, patients were excluded for severe deformity, for a score of more than 9 on the scale, or if there was a medical contraindication. Patients and assessors of outcome were blinded to the treatment group assignment, and outcomes were assessed at multiple points over a 24-month period with the use of 5 self-reported scores. The authors conclude that the outcomes after arthroscopic lavage or arthroscopic debridement were no better than those after a placebo procedure.
TABLE 94-1 Recent studies with their respective levels of evidence regarding the treatment of knee osteoarthritis with arthroscopy
Several details about this study require a more in-depth evaluation because they are certainly relevant to the authors’ conclusion that surgical intervention provided no benefit compared with placebo surgery. Forty-four percent of the eligible participants declined to participate in the study, which creates a selection bias; that is, it is possible that the patients who declined to participate had lower grades of OA and, therefore, might have experienced the best outcome.10 In addition, the presence or absence of joint effusion was not reported. This is significant because some of the indications for knee arthroscopy, such as loose bodies or meniscal tears, can be manifested clinically by a joint effusion. Finally, the method of grading OA may lead to conflicting results. For example, a patient with one severely arthritic compartment may receive the same score as a patient with mild arthritis in all three compartments. These patients are probably not comparable clinically and would most likely have different outcomes after surgical intervention. Despite these criticisms, this investigation is still the only Level I study that addresses the role of arthroscopy in OA; therefore, the authors’ conclusion should be acknowledged and taken into account when treating these patients.
Patients with symptomatic OA of the knee have a reported incidence rate of meniscal tears in up to 91% of magnetic resonance imaging (MRI) scans.11 Some surgeons have proposed that patients who have pain secondary to clinically significant meniscal tears will benefit from arthroscopic mensical debridement. Dervin and investigators,8 in a Level IV study, attempted to elicit preoperative factors that would predict a successful outcome after arthroscopy for OA of the knee. They conclude that three variables were significantly associated with clinical improvement: the presence of medial joint line tenderness, a positive Steinman test, and the presence of an unstable meniscal tear at arthroscopy. Jackson and Rouse,12 in a Level IV study, reported 95% good to excellent results obtained with arthroscopic partial meniscectomy for clinically significant meniscal tears in the setting of substantial OA. Although Chang and colleagues13 (Level II) conclude that patients with OA did not experience consistent relief after arthroscopy, they do point out that the subset of patients with anterior two-thirds medial mensical tears and any lateral meniscal tears did improve significantly. It can be difficult to determine which meniscal tears are clinically significant; many authors will use the term mechanical symptoms, which includes locking and catching, and generally refers to unstable mensical tears. Some authors have attempted to determine whether mechanical symptoms are a prognostic factor associated with a positive outcome after arthroscopic debridement. The results have been mixed. Chang and colleagues13 conclude that patients with mechanical symptoms tended to benefit, whereas Aaron and coworkers14 (Level II) and Livesley and coauthors15 found that the type of symptoms did not predict outcome. The term mechanical symptoms has a different meaning for different clinicians. Mechanical locking, which is when the knee becomes suddenly stuck in one position requiring manipulation that allows the knee to suddenly unlock, generally indicates the presence of a loose body or an unstable flap of meniscus or articular cartilage. Arthroscopy reliably eliminates this phenomenon even in the presence of arthritis. However, arthritis symptoms may not be relieved by the procedure. Lastly, the term mechanical symptoms is not specific to this type of locking.
Several authors have proposed that patients with low-grade OA can have substantial and long-lasting improvement after knee arthroscopy, whereas patients with high-grade OA fare less well. For example, Jackson and Dieterichs,16 in a Level IV study, note 91% excellent results at 4 to 6 years after debridement for knees in which degenerative change was limited to fibrillation, which they rate as stage 2. When the disease progressed to fragmentation of the cartilage (stage 3), results deteriorated to 77% fair or good. Aaron and coworkers14 and Livesley and coauthors15 note similar trends: Patients with low grades of OA had acceptable pain relief that lasted up to 3 years, while patients with higher grades of OA had significantly worse results. Aaron and coworkers14 also note that patients who had a joint space of 3 mm or larger on radiographs improved after arthroscopic debridement, whereas those with a joint space less than 2 mm rarely had a substantial relief of symptoms. It is fair to say that joint space directly correlates with the varying stages of OA; therefore, this finding supports the notion that patients with mild OA or larger joint spaces have better outcomes than those with higher grades of OA or smaller joint spaces. Matsusue and Thomson17 (Level IV) stratified their results of meniscal tear debridement based on coexisting degenerative changes within the involved compartment. They found that patients with early degenerative changes, classified as grade I or II, had 87% excellent results, whereas only 7% of the patients with grade III or IV changes experienced an excellent result. Finally, McGinley and coworkers18 (Level IV) note that greater than 80% grade 4 changes within a single compartment was a risk factor for total knee arthroplasty within 2 years. Although it is difficult to compare and contrast these different studies, because many of the investigators used a different system for grading the severity of OA, there certainly seems to be a trend toward patients with early OA having better outcomes than those with advanced OA.
In a Level V article, Stuart and Lubowitz19 propose that loose bodies within the knee joint is another prognostic factor associated with a positive result after arthroscopy in patients with OA. However, we have been unable to find data to support this statement. Aaron and coworkers14 were unable to find an association between having loose bodies and a good result after arthroscopy, although only 9 of 122 patients in their study were identified as such.
Patients with fixed varus or valgus deformity, particularly valgus deformity, have consistently demonstrated poor results after arthroscopic debridement.14,20 Likewise, patients with bilateral disease are considered poor candidates and were reported to undergo total knee arthroplasty at a greater rate (64%) when compared with a similar group of patients with unilateral disease (33%).18
GUIDELINES
Lastly, we counsel patients that arthritis symptoms tend to worsen over the long term, and that this is what they can expect over years in the future after arthroscopy in this setting. Table 94-2 provides a summary of recommendations.
TABLE 94-2 Grades of Recommendation for Summaries or Reviews of Orthopedic Surgical Studies
| STATEMENTS | LEVEL OF EVIDENCE/GRADE OF RECOMMENDATION |
|---|---|
1 Burman MS, Finkelstein H, Mayer L. Arthroscopy of the knee joint. J Bone Joint Surg Am. 1934;16A:255-268.
2 Baumgaertner MR, Cannon WDJr, Vittori JM, et al. Arthroscopic debridement of the arthritic knee. Clin Orthop Relat Res. 1990;253:197-202.
3 McLaren AC, Blokker CP, Fowler PJ. Arthroscopic debridement of the knee for osteoarthrosis. Can J Surg. 1991;34:595-598.
4 Ogilvie-Harris DJ, Fitsialos DP. Arthroscopic management of the degenerative knee. Arthroscopy. 1991;7:151-157.
5 Rand JA. Arthroscopic management of degenerative meniscus tears in patients with degenerative arthritis. Arthroscopy. 1985;1:253-258.
6 Yang SS, Nisonson B. Arthroscopic surgery of the knee in the geriatric patient. Clin Orthop Relat Res.; 316; 1995; 50-58.
7 Moseley JB, O’Malley K, Petersen NJ, et al. A controlled trial of arthroscopic surgery for osteoarthritis of the knee. N Engl J Med. 2002;347:81-88.
8 Dervin GF, Stiell IG, Rody K, et al. Effect of arthroscopic debridement for osteoarthritis of the knee on health-related quality of life. J Bone Joint Surg Am. 2003;85:10-19.
9 Leopold SS, Redd BB, Warme WJ, et al. Corticosteroid compared with hyaluronic acid injections for the treatment of osteoarthritis of the knee. A prospective, randomized trial. J Bone Joint Surg Am. 2003;85A:1197-1203.
10 Siparsky P, Ryzewicz M, Peterson B, et al. Arthroscopic treatment of osteoarthritis of the knee. Clin Orthop Relat Res.; 455; 2007; 107-112.
11 Bhattacharyya T, Gale D, Dewire P, et al. The clinical importance of meniscal tears demonstrated by magnetic resonance imaging in osteoarthritis of the knee. J Bone Joint Surg Am. 2003;85:4-9.
12 Jackson RW, Rouse DW. The results of partial meniscectomy in patients over 40 years of age. J Bone Joint Surg Br. 1982;64:481-485.
13 Chang RW, Falconer J, Stulberg SD, et al. A randomized controlled trial of arthroscopic surgery versus closed-needle joint lavage for patients with osteoarthritis of the knee. Arthritis Rheum. 1993;36:289-296.
14 Aaron RK, Skolnick AH, Reinert SE, et al. Arthroscopic debridement for osteoarthritis of the knee. J Bone Joint Surg Am. 2006;88:936-943.
15 Livesley PJ, Doherty M, Needoff M, et al. Arthroscopic lavage of osteoarthritic knees. J Bone Joint Surg Br. 1991;73:922-926.
16 Jackson RW, Dieterichs C. The results of arthroscopic lavage and debridement of osteoarthritic knees based on the severity of degeneration: A 4-to-6 year symptomatic follow-up. Arthroscopy. 2003;19:13-20.
17 Matsusue Y, Thomson NL. Arthroscopic partial medial meniscectomy in patients over 40 years old: A 5 to 11 year follow-up study. Arthroscopy. 1996;12:39-44.
18 McGinley BJ, Cushner FD, Scott WN. Debridement arthroscopy: 10-year follow-up. Clin Orthop Relat Res. 1999;367:190-194.
19 Stuart MJ, Lubowitz JH. What, if any, are the indications for arthroscopic debridement of the osteoarthritic knee? Arthroscopy. 2006;22:238-239.
20 Harwin SF. Arthroscopic debridement for osteoarthritis of the knee: Predictors of patient satisfaction. Arthroscopy. 1999;15:142-146.







