SECTION II INVESTIGATIONS OF THE CENTRAL AND PERIPHERAL NERVOUS SYSTEMS
COMPUTERISED TOMOGRAPHY (CT) SCANNING
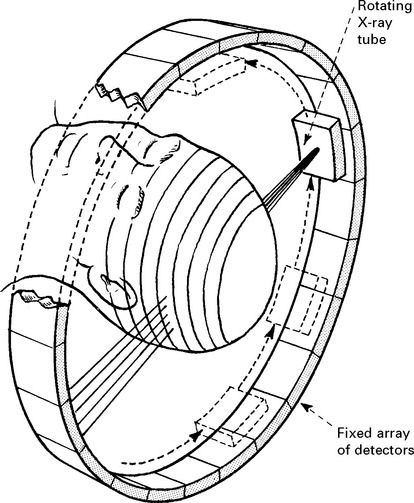
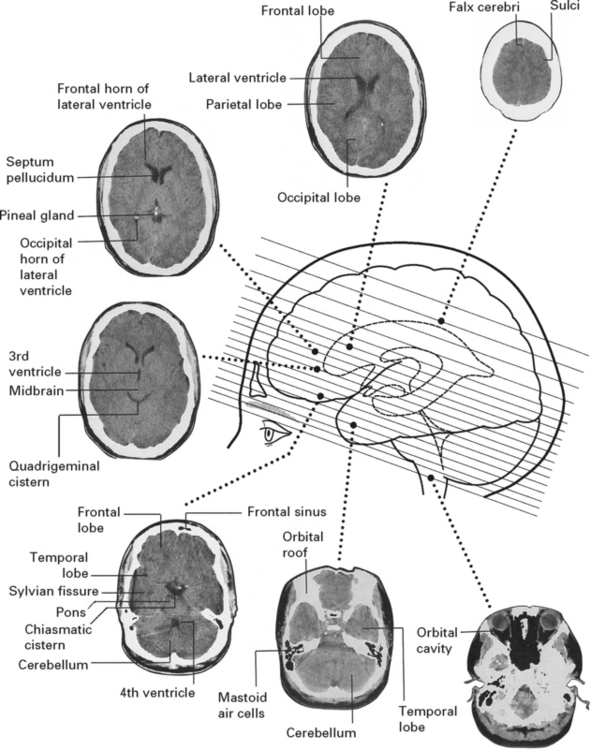
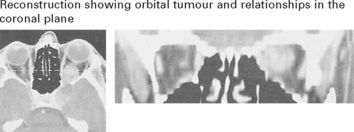
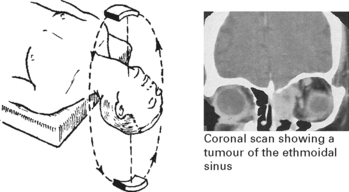
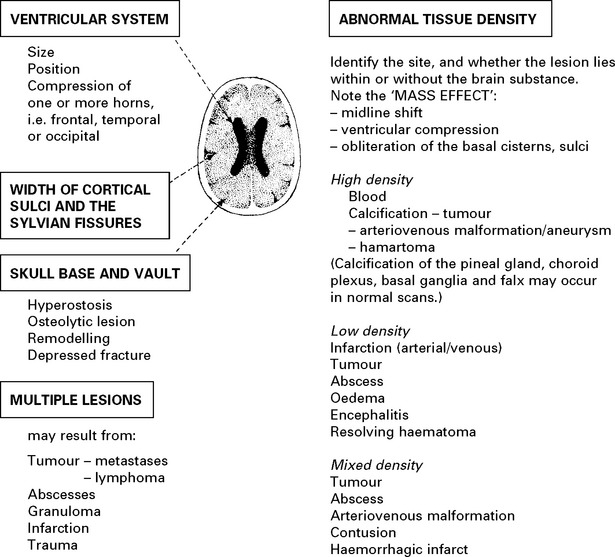
The development of this non-invasive technique in the 1970s revolutionised the investigative approach to intracranial pathology. A pencil beam of X-ray traverses the patient’s head and a diametrically opposed detector measures the extent of its absorption. Computer processing, multiple rotating beams and detectors arranged in a complete circle around the patient’s head enable determination of absorption values for multiple small blocks of tissue (voxels). Reconstruction of these areas on a two-dimensional display (pixels) provides the characteristic CT scan appearance. For routine scanning, slices are 3–5 mm wide. The latest ‘spiral’ or ‘helical’ CT scanners use a large bank of detectors (multislice) and the patient moves through the field during scanning so that the X-ray beams describe a helical path. This considerably reduces scanning time and is of particular value when slices of 1–2 mm thickness provide greater detail. These ‘high definition’ views permit coronal and sagittal reconstructions and allow detailed examination of certain areas e.g. the orbit, pituitary fossa and cerebello-pontine angle.
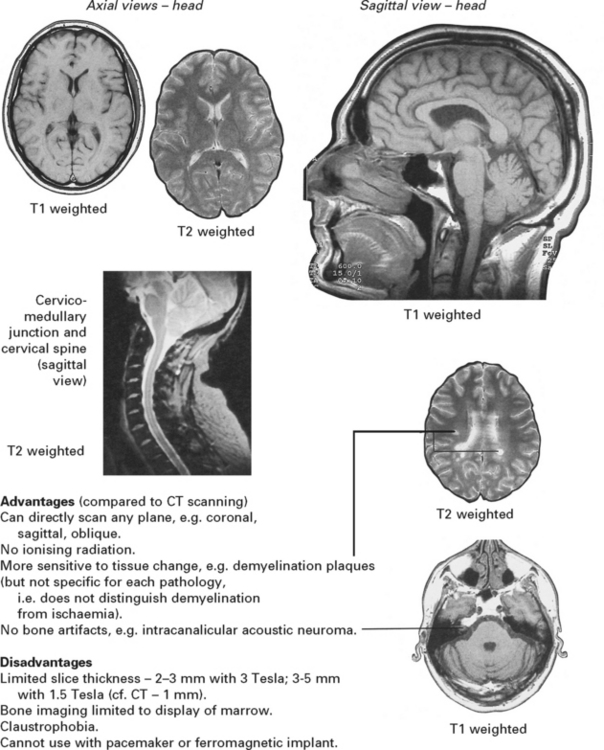
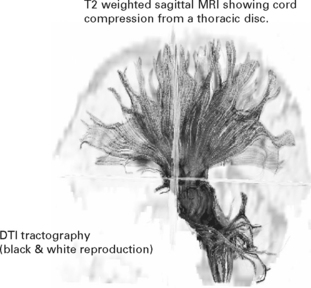
MAGNETIC RESONANCE IMAGING (MRI)
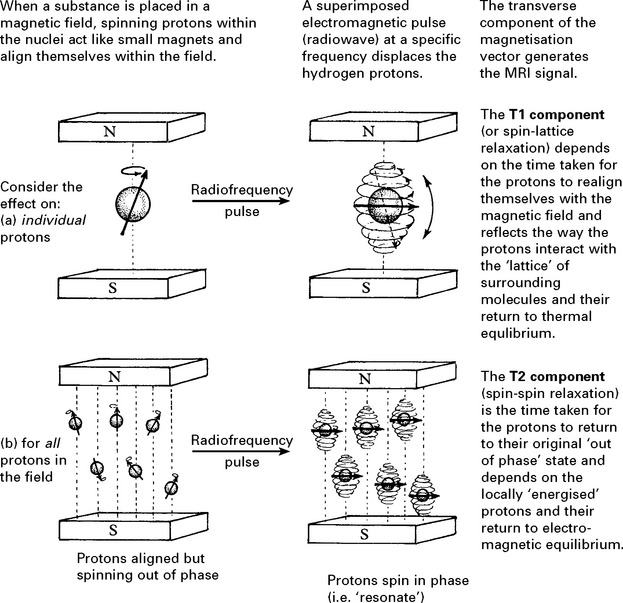
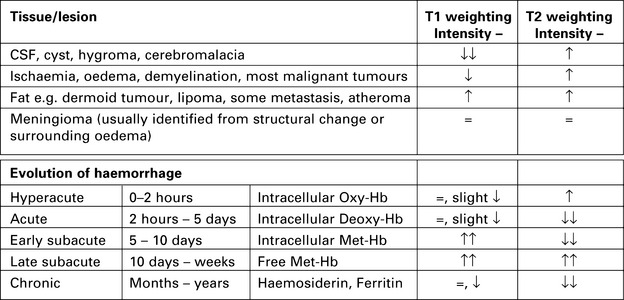
For many years, magnetic resonance techniques aided chemical analysis in the food and petrochemical industries. The development of large-bore homogeneous magnets and computer assisted imaging (as in CT scanning) extended its use to the mapping of hydrogen nuclei (i.e. water) densities and their effect on surrounding molecules in vivo. Since these vary from tissue to tissue, MRI can provide a detailed image of both head and body structures. The latest echo-planer MR imaging permits rapid image acquisition.
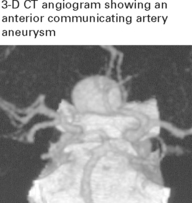
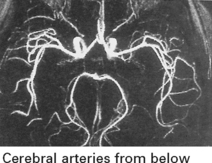
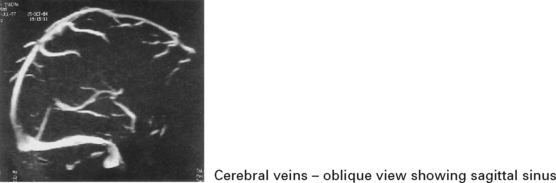
MR Angiography (MRA)
Rapidly flowing protons can create different intensities from stationary protons and the resultant signals obtained by special sequences can demonstrate vessels, aneurysms and arteriovenous malformations. Vessels displayed simultaneously, may make interpretation difficult, but selection of a specific MR section can demonstrate a single vessel or bifurcation. By selecting a specific flow velocity, MRA will show either arteries or veins. The resolution has improved with 3 Tesla MRA, but may still miss aneurysms seen on intra-arterial DSA (see page 45).
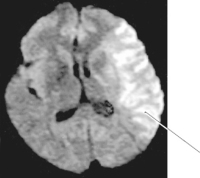
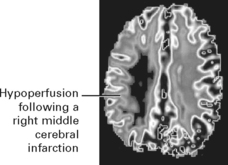
Perfusion-weighted MRI (PWI)
Images are obtained by ‘bolus tracking’ after rapid contrast injection. A delay in contrast arrival and reduced concentration signifies hypoperfusion of that brain region. Soon after onset, ischaemic changes on PWI appear larger than on DWI. The difference between PWI and DWI may reflect dysfunctional salvagable tissue (ischaemic penumbra see page 245). Early resolution of the PWI abnormality indicates recanalisation of an occluded vessel, whereas in those who do not recanalise the DWI volume expands to fill a large part of the original PWI lesion.
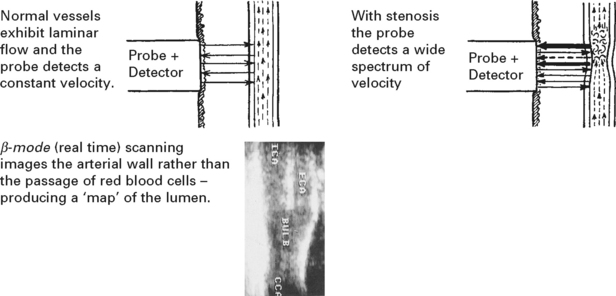
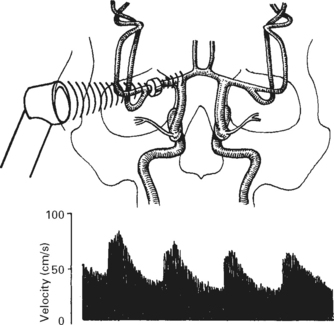
ULTRASOUND
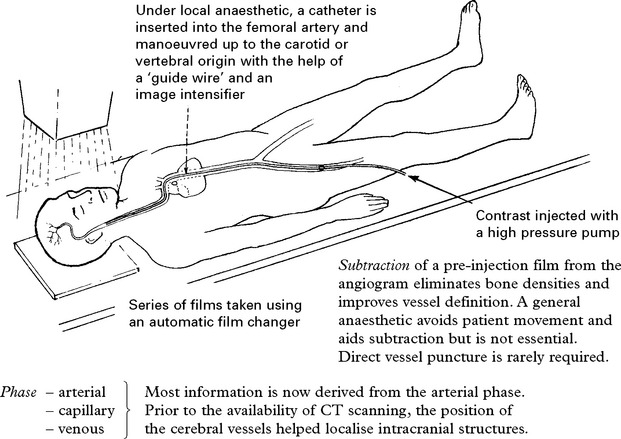
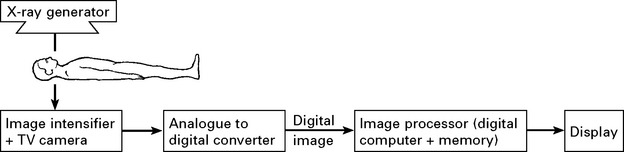
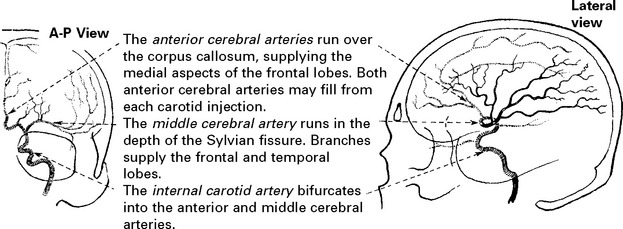
ANGIOGRAPHY
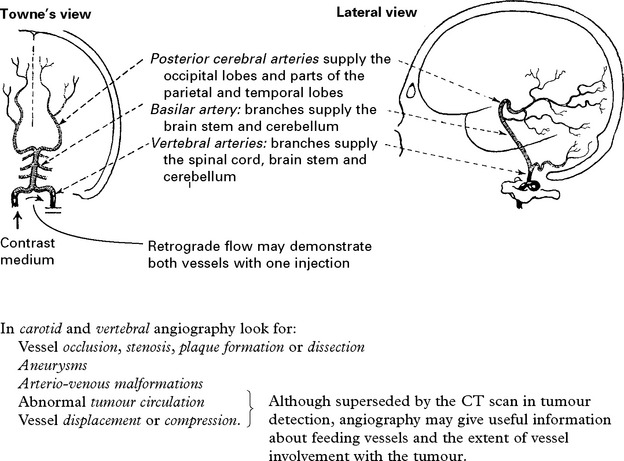
VERTEBRAL ANGIOGRAPHY
INTERVENTIONAL ANGIOGRAPHY
Platinum coils inserted into the aneurysm fundus through a special catheter can produce complete or partial obliteration. Many centres now use this technique as a first line treatment for intracranial aneurysms, particularly those at the basilar bifurcation (see page 288). Temporary inflation of a balloon within the parent vessel during coiling can help prevent occlusion of the parent vessel in wide necked aneurysms (balloon remodelling) (see page 289).
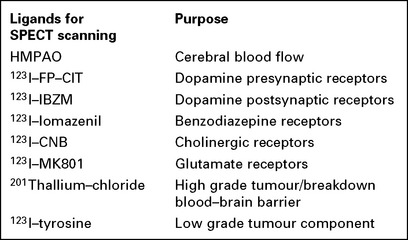
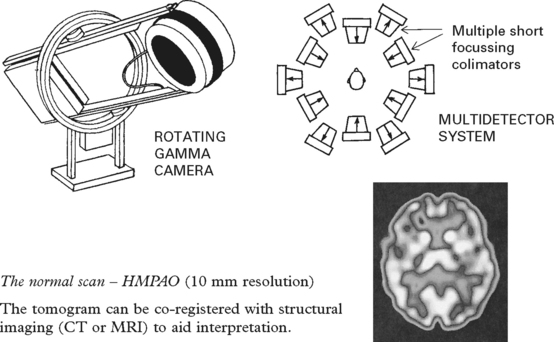
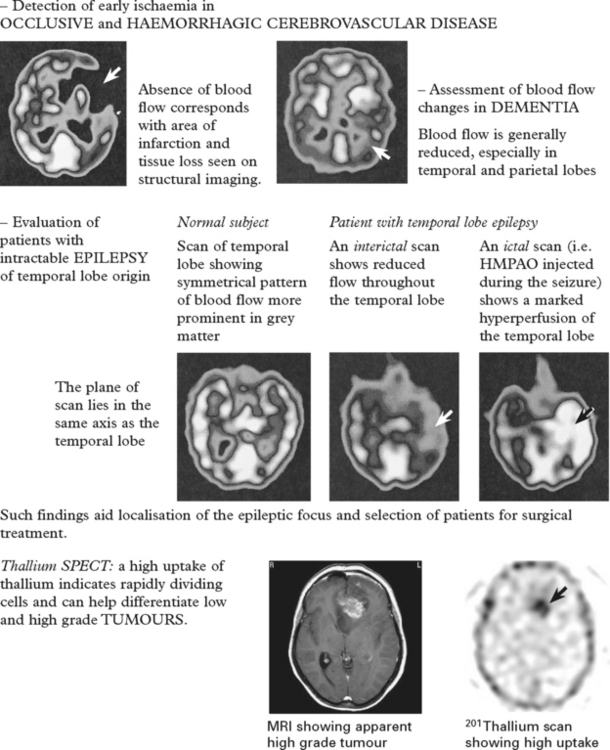
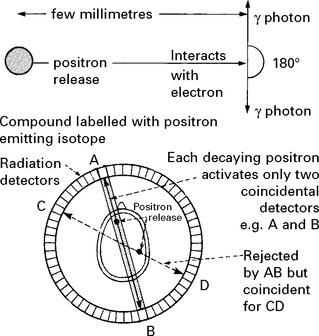
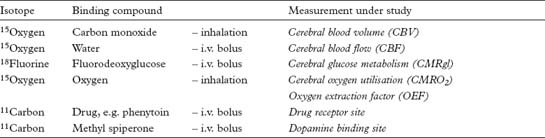
RADIONUCLIDE IMAGING
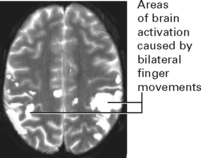
Clinical and research uses
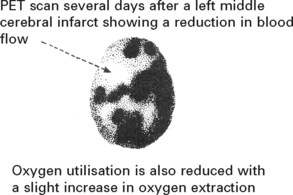
PET scanning is used primarily as a research tool to elucidate the relationships between cerebral blood flow, oxygen utilisation and extraction in focal areas of ischaemia or infarction (page 245) in patients with dementia, epilepsy and brain tumours. Identification of neurotransmitter and drug receptor sites aids the understanding and management of psychiatric (schizophrenia) and movement disorders. Whole body PET scans can also identify occult tumour in patients with paraneoplastic syndromes (page 549).
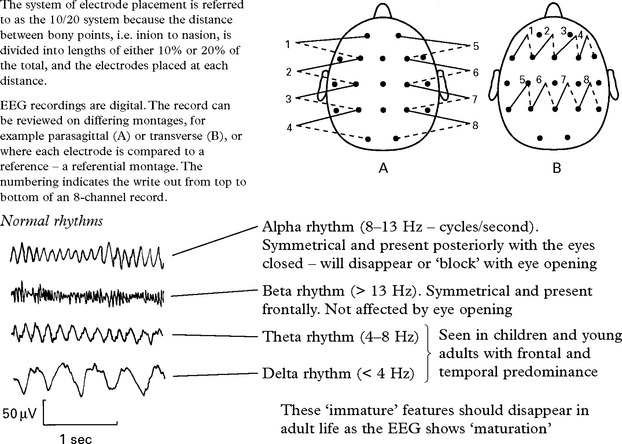
ELECTROENCEPHALOGRAPHY (EEG)
More advanced methods of telemetry and foramen ovale recording may be necessary
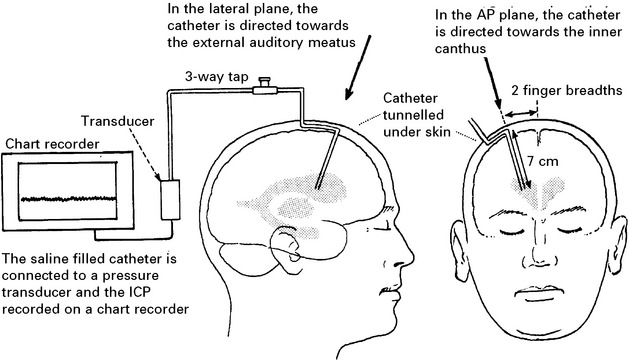
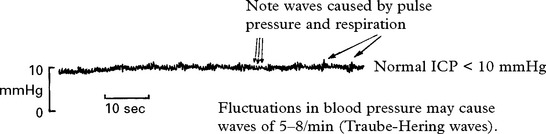
INTRACRANIAL PRESSURE MONITORING
CLINICAL USES OF ICP MONITORING
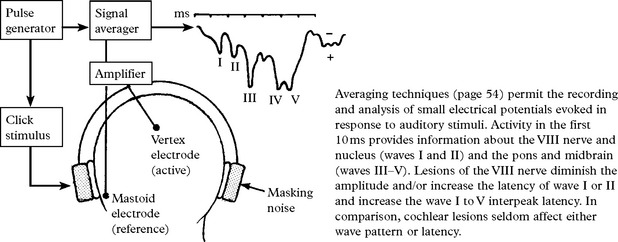
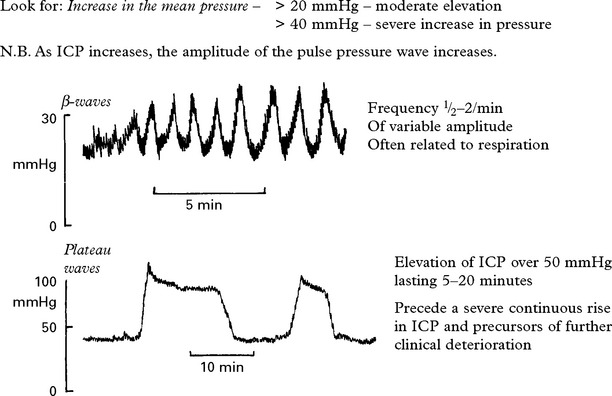
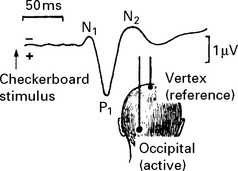
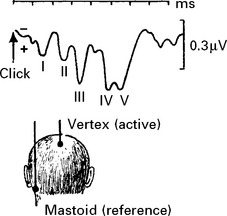
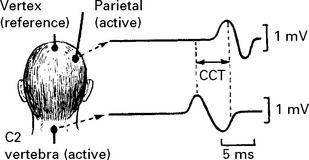
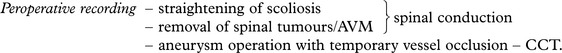
EVOKED POTENTIALS – VISUAL, AUDITORY AND SOMATOSENSORY
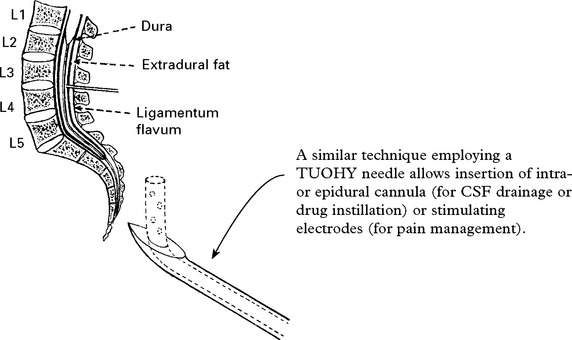
MYELOGRAPHY
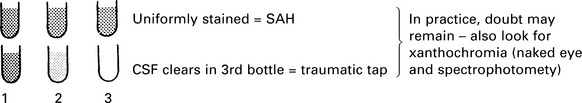
LUMBAR PUNCTURE (LP)
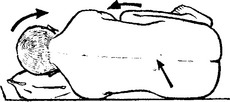
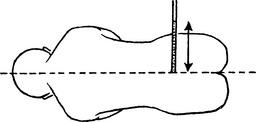
TECHNIQUE
ELECTROMYOGRAPHY/NERVE CONDUCTION STUDIES
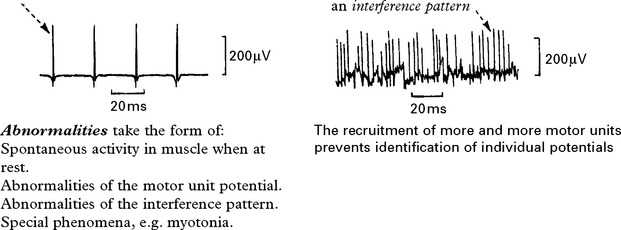
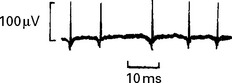
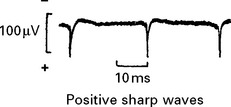
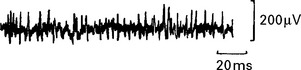
Needle electromyography records the electrical activity occurring within a particular muscle.
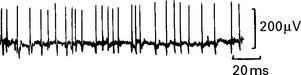
Nerve conduction studies measure conduction in nerves in response to an electrical stimulus.
Both are essential in the investigation of diseases of nerve (neuropathy) and muscle (myopathy).

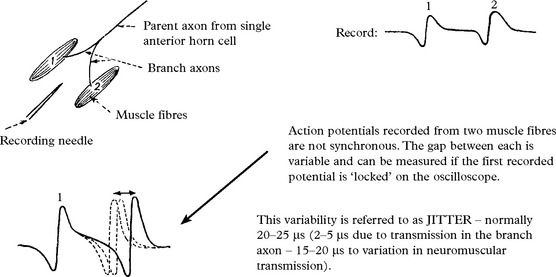
 wire is the active electrode and the outer casing the reference electrode. This records from an area of 300μ radius.
wire is the active electrode and the outer casing the reference electrode. This records from an area of 300μ radius.