Chapter 5. Investigations
Although laboratory and radiological investigation of orthopaedic patients is helpful, the single most important step in establishing a diagnosis and determining the management of a patient is a properly taken history. The clinical history yields information that no laboratory or computer can provide.
The second most useful step in determining management is clinical examination. Only when a proper history has been taken and a clinical examination performed should investigations be requested. When these results are available they should be interpreted in the context of the patient’s symptoms, job and home circumstances. To rely on investigations alone, without relating them to the patient’s symptoms and individual circumstances, is wrong.
Radiology
Radiographs are essential in orthopaedics, not only to recognize fractures and other bone lesions but also to determine the best way to treat a fracture, the accuracy of reduction and the state of union. Radiographs are so important that it is sometimes forgotten that the bones they show belong to people and it is all too common an error for treatment to be decided on the basis of radiographs alone. Pain and motivation do not show on a radiograph!
Physics of radiology
The visibility of a structure on a radiograph depends upon the atomic weights of its constituent elements. Calcium, with an atomic weight of 40, is easily visible, and so are barium (137) and iodine (127). Fat, water and carbohydrate, which consist of carbon (12), hydrogen (1) and oxygen (16), are hardly visible but the iron (56) of haemoglobin and fascia, which contains sulphur (32) within the collagen molecule, can be seen more clearly. Careful examination of a radiograph will therefore show far more than just bone. The individual muscles and the fascial sheaths around them can be seen, and a fluid level of fat in a joint is a sure indication of an intra-articular fracture (Fig. 5.1). Although it is fair to say that many of the abnormalities visible radiologically can be detected more easily by clinical examination, it is still helpful to recognize a joint effusion on a radiograph and know that it consists of blood rather than synovial fluid.
 |
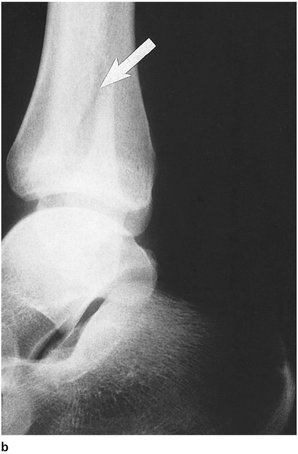
| Fig. 5.1
Haemarthrosis of the knee. Note the fluid level, with fat floating on blood, indicating a fracture within the knee.
|
Looking at a radiograph
Orthopaedic radiographs must always be taken in at least two planes because lesions can be missed if one shadow is superimposed upon another, particularly with fractures, where one view may show gross displacement while the other is anatomical. When one view is good and one is bad, the worse position is always correct because displacement can never be an artefact (Fig. 5.2).
 |
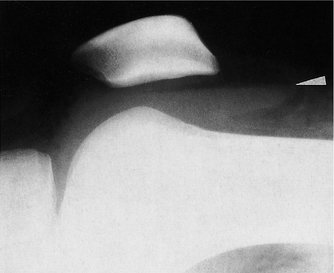
| Fig. 5.2
The worst views are always the most accurate: (a) good alignment may be an artefact but bad alignment can never be; (b), (c) radiographs of the same fracture.
|
All radiographs are eventually examined by a radiologist, but the orthopaedic surgeon has to make a decision on management before the report is available and must therefore examine the films correctly. This is especially true in the accident department, a place rich in pitfalls for the unwary (Fig. 5.3a and Fig. 5.3b). Undisplaced fractures which are missed always slip when the patient reaches home and impacted fractures never disimpact until the patient has been reassured that he has no broken bones.
 |
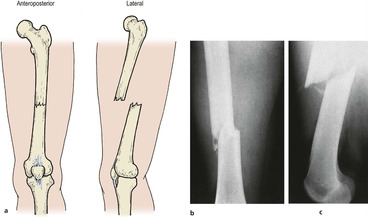
| Fig. 5.3a
The importance of two projections. Can you see the fracture on this X-ray? See (b).
|
 |
| Fig. 5.3b
The fracture is in the fibula.
|
If treacherous fractures are not to be missed, every cortex of every bone must be examined systematically on every view. It helps to trace around the cortices with a pencil (without marking the film) when doing this. Meticulous examination of each bony detail can, however, lead to something very obvious being missed and it is just as important to stand back and view the radiograph as a whole picture, particularly when a structure such as the spine is being examined.
Although bones are easily seen, soft tissues also cast shadows, but the brightness of the viewing box makes them difficult to see. Because the area of viewing box not covered by the radiograph is very bright, the examiner’s iris constricts and obscures detail in the darker areas. It is surprising how much more of the soft tissues can be seen if the exposed area of the viewing box is masked; try looking down a tube of rolled up radiograph to confirm this.
Special techniques
Tomograms
The X-ray source and plate are moved to produce a blurred radiograph that leaves only one plane or slice of tissue in focus. Tomograms are useful in the investigation of defects deep within a bone, but they have their limitations (Fig. 5.4). To make tomographic cuts less than 1 cm apart is difficult and lesions less than 1 cm in diameter are easily missed. These shortcomings have made the technique almost obsolete but it is important to understand the principles because it is the forerunner of computed tomography (CT), which has largely superseded plain tomography.
 |
| Fig. 5.4
A tomogram showing an area of avascular bone and depressed cortex in a joint.
|
Contrast studies
Structures that are not normally seen on a radiograph can be made visible by coating them with a radiopaque material such as iodine or barium, by filling cavities with gas, or both. The use of two materials, gas and a solution opaque to X-rays, is double-contrast radiography and is particularly useful in the investigation of joints, when it becomes double-contrast arthrography.
Radiculography and myelography. Iodine solutions can be injected into the spinal theca to outline the spinal canal and nerve roots stretched over a prolapsed intervertebral disc.
Arthrography. Double-contrast arthrography can outline the menisci and other intra-articular structures with great clarity (Fig. 5.5). A radiopaque medium is injected first, left in the joint long enough to spread over the intra-articular structures, and the joint inflated gently with gas, usually carbon dioxide, to outline the intra-articular surfaces more clearly. Carbon dioxide is used because it is more rapidly absorbed; if air or nitrogen is used the joint can make an unpleasant squelching noise for as long as a week.
 |
| Fig. 5.5
An arthrogram showing a torn meniscus, a deep meniscosynovial sulcus, articular cartilage and bone.
|
Although double-contrast arthrography is helpful in outlining solid structures, it is less useful in showing irregularities of joint surfaces or inflammation of soft tissue. Particular applications of double-contrast arthrography are in the investigation of internal derangements of the knee or shoulder and in congenital dislocation of the hip in children.
Discography. Radiopaque medium can be injected into the intervertebral discs to demonstrate lesions in the body of the disc. Apart from making the disc lesions visible, the increase of intradiscal pressure caused by an injection may reproduce the patient’s symptoms and confirm the diagnosis.
Stress radiographs
Joints with doubtful stability can be examined under load to detect abnormal joint laxity and are particularly useful at the ankle and knee if plain films are unhelpful (Fig. 5.6).
 |
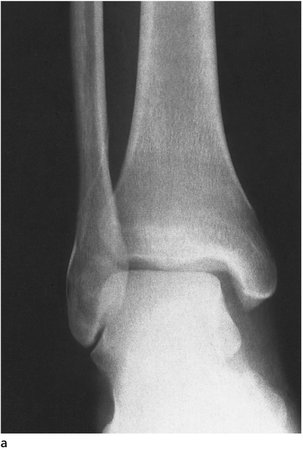
| Fig. 5.6
Stress radiographs. Stress is applied to a knee with a ligament rupture. The shadow is the surgeon’s hand in a lead glove.
|
Computed tomography
Slight differences between the radiodensities of various elements can be enhanced by computer. If radiographs are made at different angles and in different planes, the computer can integrate the information to produce pictorial ‘slices’ of the body and demonstrate structures not recognizable on a standard radiograph or tomogram. New developments include a ‘three-dimensional’ presentation of the image which displays an entire bone as if it were a shaded drawing (Fig. 5.7). A disadvantage, doubtless soon to be overcome, is an inability to show metal without distorting the rest of the image.
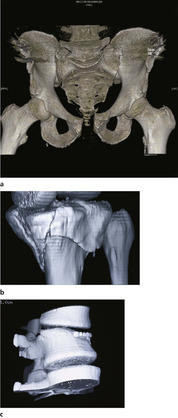 |
| Fig. 5.7
(a) CT 3D reconstruction of pubic diastasis and damage to sacroiliac joint; (b) reconstruction tibial plateau fracture; (c) reconstruction vertebral crush fracture.
|
CT has made an enormous impact on the management of soft tissue lesions in the abdomen and central nervous system, including prolapsed intervertebral discs, and is now essential to determine the exact anatomy of complicated spinal and pelvic fractures (Fig. 5.8). CT scans give precise information and reveal spicules of bone that might damage nerve roots or the spinal cord. A practical problem is that CT equipment is so large and cumbersome that severely injured patients and those with multiple fractures cannot easily be examined, and this limits its usefulness.
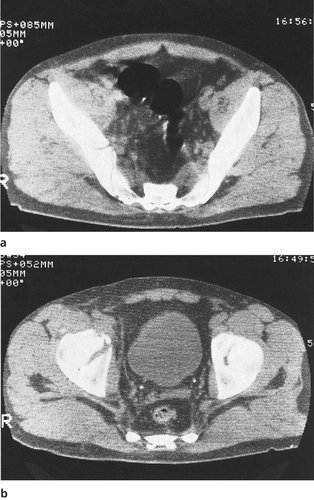 |
| Fig. 5.8
CT scans showing (a) fracture through the ilium; (b) fracture of the right acetabulum.
|
Magnetic resonance imaging
Magnetic resonance imaging (MRI), sometimes known as nuclear magnetic resonance (NMR), depends on the behaviour of protons in a magnetic field rather than radiodensity. The protons, or hydrogen nuclei, are first made to line up by exposing the body to a powerful magnetic field. Once they are aligned, the body is exposed to a radiofrequency stimulus which reorientates the nuclei. When the radiofrequency stimulus is withdrawn, the nuclei swing back to their previous position and this movement can be displayed visually (Fig. 5.9).
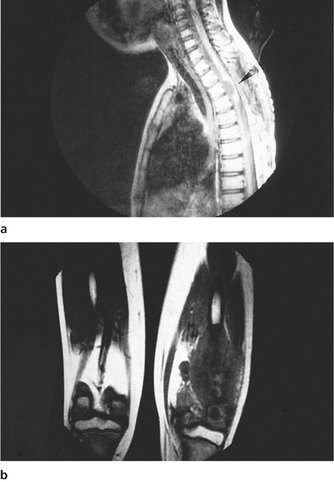 |
| Fig. 5.9
MRI scans showing: (a) a space-occupying lesion in the spinal canal of a child; (b) a tumour in the tissues in the back of the right thigh in a child.
By kind permission of the MRIS Unit, Addenbrooke’s Hospital, Cambridge.
|
Different elements behave differently and the technique can be used to display, for example, the distribution of phosphate. Hydrogen is generally used because it provides the best images of soft tissues, which are shown more clearly than with CT and without the need to expose the patient to radiation.
MRI is invaluable in the investigation of intracranial lesions but is less useful in bone, which contains less water and thus fewer hydrogen nuclei. It can also show changes in the vascularity of bone following trauma and degenerative change in the intervertebral discs and ligaments. It is now widely used in soft tissue injuries around a joint, assessing the chondral surfaces, menisci and ligamentous structures. It is also very useful in the assessment of benign and malignant bone tumours, their characteristics, spread and involvement of other tissues. MRI is now a routine investigation.
Radioisotope scanning
Radioactive isotopes (radioisotopes) can be used to ‘tag’ radicals, such as phosphate, which are metabolically active in bone and other skeletal structures. Compounds made radioactive in this way can be injected intravenously and will find their way to the target tissue, where they can be demonstrated by scanning the body for radioactivity.
Available radioisotopes
The choice of radioisotope depends on the specificity of the radioisotope for individual tissues, its half-life, and its availability.
The preparation of the radioisotopes poses practical problems. Most must be prepared in an atomic pile and used promptly before the radioactivity decays. A short half-life minimizes the dose of radiation to the patient but, if too short, it can be impossible to get the isotope into the patient before it decays. Technetium-99m is widely used because it has a half-life of only 6 hours but can be prepared daily in the hospital by eluting with saline an ion-exchange column containing molybdenum-99.
Patients are often concerned, and rightly so, about the dosage of radiation from a ‘whole body nuclear isotope scan’. Comparison of radiation doses from different investigations is not as simple as it might appear because the amount of radiation received by the skin, bone marrow and the deep structures is not strictly comparable. In simple terms, a skeletal scan involves a higher dose of radiation than a chest or pelvis radiograph, but not as much as a barium meal or intravenous urogram.
Technetium-99m
Technetium-99m combined with a phosphate compound is deposited in areas of osteoblastic activity, and is commonly used to outline bone lesions. The compound is only taken up by bone that is being laid down or resorbed – ‘coming and going bone’. Areas of dead or sclerotic bone appear as ‘cold’ areas (Fig. 5.10 and Fig. 5.11). Although this limits its value, there is no other way to demonstrate the metabolic state of individual areas of the skeleton and the technique is complementary to conventional radiography (Fig. 5.12). In children with acute osteomyelitis (p. 311), the technetium scan is usually positive long before radiographs show the lesion.
 |
| Fig. 5.10
Isotope scan of a child showing increased activity at the most active epiphyses. Note that there is more activity at the knees than at the hips or ankles, and at the shoulders than at the elbows or wrists.
|
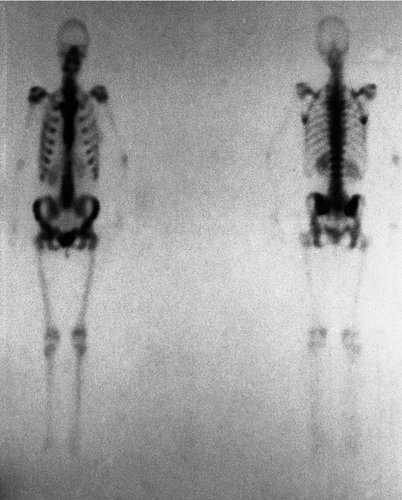 |
| Fig. 5.11
Isotope scan. A technetium-99m scan of a normal adult skeleton from front ( left) and back ( right).
|
 |
| Fig. 5.12
(a) An isotope scan to show a destructive lesion of the bone; also visible radiologically (b).
|
Gallium-67
Gallium-67 has less affinity for bone but is taken up by proteins found in healing bone and many tumours. Gallium-67 gives a fair indication of the presence of infection, although it is far less specific for pus than technetium-99m is for bone lesions.
Indium-111
Indium-111 can be used to label leucocytes, which are found at sites of infection. It is better than gallium-67 for soft tissue infections but gallium is more reliable for infections in bone.
‘Blood pool’ image
To learn as much as possible from the investigation, the body is scanned twice, once shortly after injection of the radioisotope and the second time a little later. The first ‘blood pool’ image shows how quickly the radioisotope reaches the lesion and is an indication of its vascularity. The delayed image, obtained several hours later, shows how long it remains in the lesion and demonstrates its osteoblastic activity.
Indications
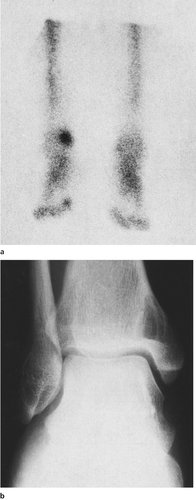
Isotope scans are particularly useful in the investigation of persistent pain for which no clinical or radiological cause can be found. A fatigue fracture of the tibia, for example, may not be visible radiologically but shows up clearly on a radioisotope scan as a hot spot, as do small vascular lesions such as osteoid osteomas (Fig. 5.13). Conversely, a normal radioisotope scan can confirm that there is no abnormal bone activity, and that if pathology is present it probably lies elsewhere.
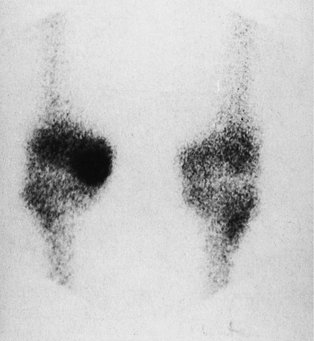 |
| Fig. 5.13
Isotopic hot spots. An isotope scan showing an area of increased activity in the medial femoral condyle of a knee.
|
A specific use of bone scanning is in the assessment of prosthetic joints that are painful after joint replacement. If the prosthesis has loosened and there is a foreign body reaction around the prosthesis, the affected area will be seen on the bone scan as a hot area. A technetium scan will not show if there is infection as well as loosening, but a gallium scan may give some indication of this.
Thermography
Thermography creates a pictorial representation of the warm areas around a joint, which gives an indication of blood supply and thus areas of inflammation or vascular disease.
Because the instruments are very sensitive, great care must be taken to avoid artefacts. The ambient temperature must be carefully controlled and the affected area must be allowed to reach a steady temperature before the investigation is performed, particularly if the patient has been wearing a bandage or dressing. The limb must also be positioned correctly and consistently.
Thermograms can be used to assess the progress of chronic joint disease, particularly rheumatoid arthritis and its response to treatment, but it is a non-specific investigation in that it will determine only where the areas of inflammation are and not the pathology that is responsible for them. Like a radioisotope scan, the thermogram provides an indication of tissue activity unobtainable in any other way.
Arthroscopy
An arthroscope is nothing more than a telescope used to look inside joints and inspect nooks and crannies not accessible even through a full arthrotomy. Fine detail, including the synovial capillaries, can be seen. Arthroscopy involves more than just the visual inspection of the interior of a joint. The individual structures can be manipulated with a probe or hook, and the movement of one structure on another observed as the joint is moved (Fig. 5.14).
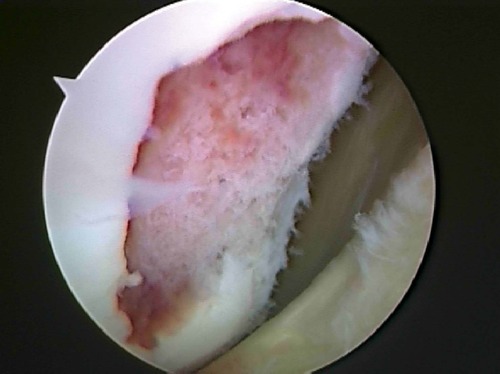 |
| Fig. 5.14
Arthroscopic view of an osteochondral defect in the medial femoral condyle of a knee.
|
The principal use for arthroscopy is in the management of internal derangements of various joints, most commonly the knee. It is possible to operate inside the knee and other joints while looking through the arthroscope and perform extensive surgery through two small puncture wounds instead of the long incision of an arthrotomy. The technique is now developed to the point that open procedures upon these joints are seldom required. Even major reconstructive work can be done with relative ease.
Examination under anaesthetic
It is difficult to examine a painful joint thoroughly with the patient awake, particularly if ligamentous instability is suspected. Examination with the patient asleep and fully relaxed allows the integrity of the ligaments to be assessed and the range of movement measured accurately. In practice, examination under anaesthetic (EUA) is usually combined with arthroscopy and is seldom performed as an isolated procedure.
Laboratory investigations
Orthopaedic surgeons make few routine demands upon the laboratory.
Uric acid or urate estimation is needed if gout is included in the differential diagnosis but is not a routine investigation. Remember that the levels are variable and that a single normal level does not exclude the diagnosis of gout.
Tests for rheumatoid arthritis vary from hospital to hospital and it is sensible to use the same tests as the local rheumatologists. The Rose–Waaler, or sheep cell agglutination test (SCAT) and the latex test are both used but, like the uric acid estimation, need not be performed as routine.
Biochemical investigations, including serum calcium, phosphorus and alkaline phosphatase, are essential in the investigation of metabolic bone disease, as described on p. 317.
Synovial fluid may be examined for crystals, cells and blood. Viscosity and biochemical investigations on synovial fluid are also possible.
Preoperative assessment
Routine investigations for patients having operations are the same as those for other surgical patients.
Haemoglobin estimation
Haemoglobin estimation and white cell count should be done in every patient if blood loss is likely or anaemia is a possibility, but can be omitted before very minor elective procedures.
Cross-match
The appropriate quantity of blood should be cross-matched after giving the laboratory adequate notice.
MRSA
Swabs should be taken from elective surgery patients to screen for MRSA.
Urea and electrolytes
These should be estimated in patients over 60 and those who have been taking diuretics or non-steroidal anti-inflammatory drugs (NSAIDs) for long periods, or have a history of renal disease.
Erythrocyte sedimentation rate
An erythrocyte sedimentation rate (ESR) is useful if a total joint replacement is to be performed because patients with a loose or infected prosthesis usually have a raised ESR and a preoperative figure is useful as a baseline for comparison. The test is also valuable in investigating acute infections and tumours. Although a normal ESR cannot exclude a condition completely, a normal reading makes it most unlikely that the patient has a bone infection, tumour or rheumatoid arthritis.
Blood gases
PCO 2, PO 2 and pH should be measured in patients who have suffered major trauma.
Electrocardiogram
An electrocardiogram (ECG) is advisable for men over 55, women over 65, and anybody with cardiovascular disease.
Chest radiograph
A chest radiograph is needed for the following:
• Patients over 65.
• Patients with symptoms or signs in the respiratory or cardiovascular systems.
• Patients with a history of chest disease.
• Patients with malignant disease.
• Recent immigrants.
Radiographs
A recent radiograph of the part to be operated on is needed unless it is soft tissue only.
Electrical studies
Nerve conduction studies
Nerve conduction studies are tedious to perform, uncomfortable for the patient, and may be difficult to interpret. They should not be requested without a very good reason.
The conduction velocity in the myelinated fibres of a peripheral nerve can be measured by stimulating the nerve with a square wave pulse of 50–250 V lasting 0.05–0.2 ms using surface electrodes and recording its arrival either further along the nerve or at the muscle it supplies.
Pressure on a peripheral nerve may cause local demyelination or axonal degeneration, which slows conduction through the damaged segment and reduces the amplitude of the recorded response, yielding information about the performance of the nerve.
Demyelination slows nerve conduction or blocks it completely and this reduces the amplitude of the recorded response.
Abnormalities may be localized, as in traumatic lesions, or generalized, as in a peripheral neuropathy, but lesions of the central nervous system, such as multiple sclerosis, show no abnormality in the peripheral nerves.
Motor nerves
The normal conduction velocity in a peripheral motor nerve is about 50 m/s in the arm and 45 m/s in the leg, but the velocity varies with temperature and the age of the patient. Conduction is slower in neonates and the elderly, and the velocity falls 2 m/s for every 1°C drop in temperature. The values may vary according to the technique and equipment used and most laboratories have their own set of ‘normal’ values.
Sensory nerves
The conduction velocities in peripheral sensory nerves are similar to those in motor nerves, but a little faster, and subject to the same variables.
Sensory conduction can be measured orthodromically; i.e. as the impulse travels towards the central nervous system, or antidromically, in the opposite direction. Antidromic stimulation, e.g. by stimulating the median nerve at the wrist and recording the arrival of the impulse in the index, is easier to perform and gives greater amplitudes.
Electromyogram (EMG)
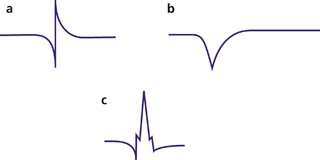
The electrical activity of muscles can be detected with a needle electrode in the muscle belly and demonstrated visually on an oscilloscope or audibly through a loudspeaker. At rest, a normal muscle is silent but if its nerve supply has undergone axonal degeneration the individual muscle fibre will contract spontaneously and rhythmically. This activity can be recorded easily in relaxed muscle as ‘positive sharp waves’ or ‘fibrillation potentials’; these indicate serious damage to the nerve but may take as long as 3 weeks after injury to appear (Fig. 5.15).
 |
| Fig. 5.15
EMG traces: (a) normal appearance; (b) positive sharp wave of denervation; (c) polyphasic wave seen in myotonia.
|
Different lesions cause different appearances. The individual wave formations are called ‘units’. Large units can indicate anterior horn disease, while small polyphasic units are seen in inflammatory muscle disease and peripheral neuropathies. The duration and stability of a unit can also give useful information but careful interpretation is needed.
Bacteriology
Culture and sensitivity
Obscure infections with fungi or exotic bacteria are seen occasionally and need the closest possible cooperation with the bacteriology department. Because many bacteria are very difficult to culture in the laboratory, it is essential that the right specimen reaches the laboratory, in the best condition possible, and in the correct transport medium. In many instances, there is only one chance to obtain a good specimen and a brief telephone call to the laboratory before it is sent can avoid the catastrophe of finding that the specimen reached the laboratory in an unusable condition. Polymerase chain reactions may improve the sensitivity of the normal culture methods.
Smear
Do not forget that a simple smear and Gram stain may sometimes yield valuable information in less than 10 minutes.
Serology
Serological tests for infection, such as the antistreptolysin and antistaphylolysin titres, may also be needed, but the cases in which they are relevant are so rare that it is wise to discuss the problem with the laboratory beforehand to ensure that the investigations are appropriate. New investigations and new antibiotics are constantly being introduced and it is impossible for the clinician to keep absolutely up to date with all of them.
Case report
The following is an example of the way in which an orthopaedic patient might be investigated.
History
A 68-year-old retired farmer, who lives with his wife in a two-storey cottage, attends hospital with pain in the groin following total hip replacement 2 years earlier. The pain is worse when he bears weight on the leg and the hip is painful at the extremes of movement. The patient is otherwise well.
Examination
On clinical examination, the patient appears fit and the hip movements are as follows:
• Flexion: 80°.
• Extension: 30° (i.e. a fixed flexion deformity of 30°).
• Internal rotation: 20°.
• External rotation: 30°.
• Abduction: 20°.
• Adduction: 20°.
Inspection, palpation and stressing the joint reveal nothing.
Investigations
Radiographs
Plain radiographs show the prosthesis in good position but there is a narrow transradiant line between cement and bone near the tip of the femoral component.
Laboratory investigations
Haemoglobin and white cell count are normal, but the ESR is raised at 45 mm/h, compared with 15 mm/h before operation, which is consistent with either loosening or infection around the prosthesis. Urea and electrolytes, requested because the patient is over 60, are normal.
Isotope scan
A technetium bone scan is performed and reveals a hot spot around the lower end of the prosthesis. A gallium scan is also hot in this area, suggesting that there may be an infection.
Operation
The patient’s symptoms become worse and it is decided to explore the hip prosthesis and, if possible, replace it. An ECG is normal; 4 units of blood are cross-matched; 500 mg flucloxacillin is given intramuscularly with the premedication and the bacteriologist told that this has been given.
Bacteriology
The bacteriologist requests specimens of cement from the area of the hot spot, swabs from the cavity in the femoral shaft, and tissue from the same area.
No frank infection is found at operation, the cavity is curetted thoroughly and fresh specimens are sent to the laboratory. Aerobic, anaerobic and micro-aerophilic cultures are set up within 30 min of collection and a new hip prosthesis is secured with antibiotic-loaded cement.
The laboratory cultures Staphylococcus albus from the specimens. S. albus is normally found on the skin and is not usually considered to be a pathogen, although it can give rise to a low grade infection in the presence of a foreign body such as a prosthesis. It is sensitive to flucloxacillin.
Progress
The patient made a satisfactory recovery and 2 years later still had a pain-free hip.